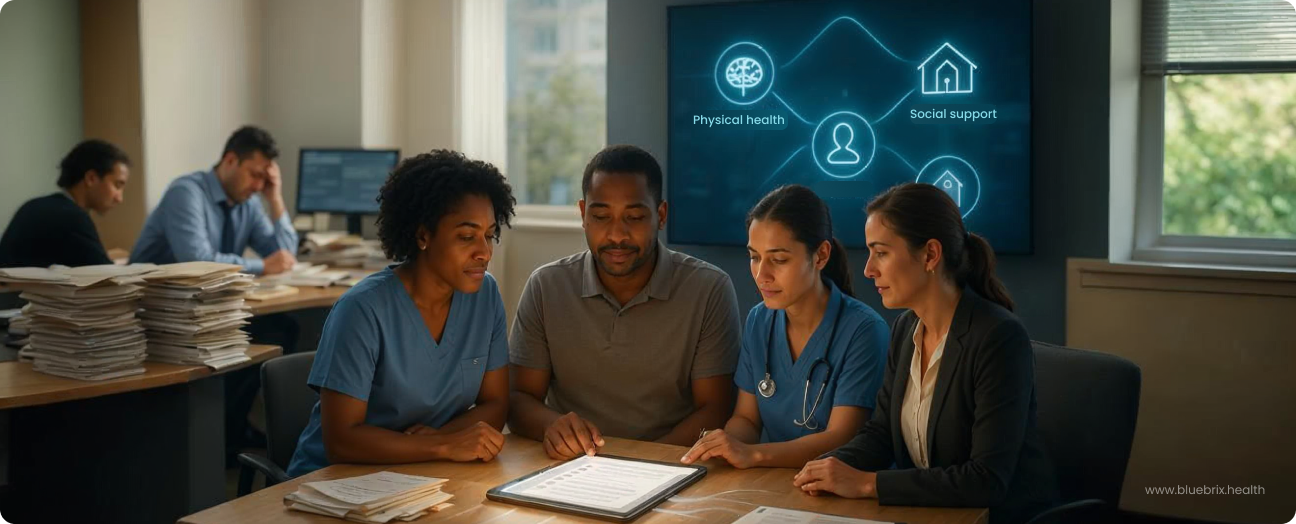
Is your Coordinated Behavioral Care (CBC) network battling fragmented data, data silos, and manual tasks? You’re not alone. The promise of integrated care—unifying mental health, substance use services, physical health, and social support—is powerful, but its delivery is often hindered by systemic hurdles that directly impact patient outcomes and staff well-being. This blog reveals how the blueBriX platform transforms these operational challenges into opportunities for stronger care coordination, financial health, and workforce empowerment.
The unspoken challenges: pain points for coordinated behavioral care providers
Even with the best intentions and the most dedicated teams, delivering truly coordinated behavioral care faces systemic hurdles. These aren’t just minor inconveniences; they directly impact patient outcomes, operational efficiency, and the well-being of staff.
Data silos and fragmented information
Imagine a patient seeing a primary care physician, a therapist, and an addiction counselor, with each provider holding critical pieces of their health story in separate systems. This is the reality for many organizations. Patient information often remains locked in disconnected silos, making it nearly impossible for care teams to get a complete, real-time view of a patient’s journey. This fragmentation leads to redundant assessments, missed interventions, and a higher risk of adverse events. It compromises the very essence of “whole-person care.”
The burden of manual processes and administrative overload
The administrative tasks in healthcare are immense. For providers in coordinated care settings, this often means navigating multiple portals, re-entering data, and managing complex referral processes manually. This isn’t just inefficient; it’s a significant drain on valuable time and resources. Clinicians, who entered the field to help people, find themselves bogged down by paperwork, contributing to burnout and taking precious time away from patient interaction. Scheduling complexities and “referral leakage” – when patients don’t follow through on critical referrals – are common frustrations that undermine continuity of care.
Navigating the complexities of care coordination
The ideal of seamless care transitions often bumps into the reality of fragmented systems. How do organizations ensure a smooth handoff when a patient moves from inpatient to outpatient care? How do they maintain a truly aligned treatment plan when multiple providers are involved, potentially using different documentation methods? Closing the loop on patient progress, ensuring follow-ups are completed, and sharing vital information between different providers can feel like a constant uphill battle.
Meeting the demands of value-based care and compliance
The shift from fee-for-service to value-based care emphasizes outcomes over volume. While laudable, this transition demands robust data collection, accurate outcome measurement, and sophisticated reporting capabilities – areas where many behavioral health providers have historically lagged. Furthermore, navigating ever-evolving regulations like HIPAA, the 21st Century Cures Act, and the emerging TEFCA standards, along with specific requirements like CFR 42 Part 2 for substance use disorder records, adds layers of complexity to daily operations and billing. Proving the value delivered for reimbursement becomes a significant challenge without the right tools.
Engaging patients effectively in their own journey
True coordination includes the patient as an active partner. However, many systems lack intuitive tools for patient engagement, making it difficult for individuals to access their health information, track their progress, or communicate easily with their care team. This can lead to lower adherence to treatment plans and a reduced sense of ownership over their own health, undermining the collaborative spirit of coordinated care.
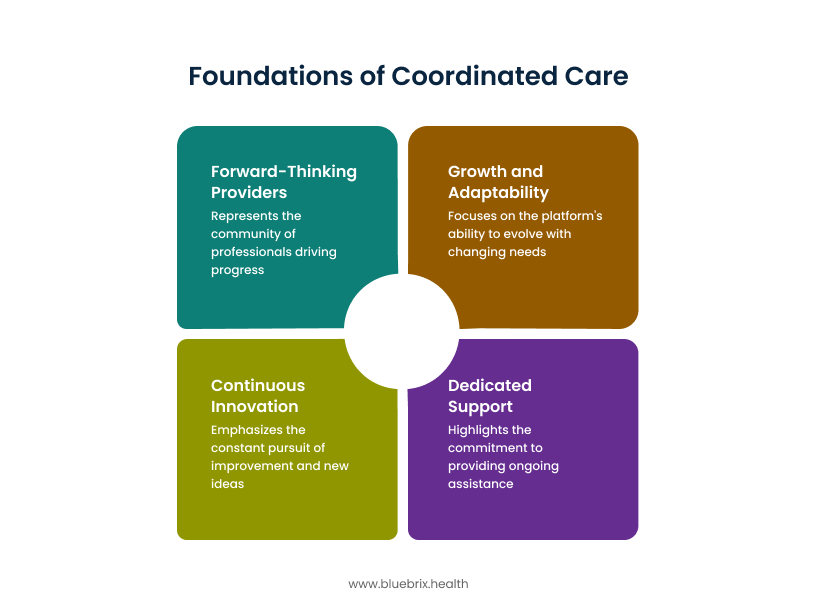
Tailored solutions for coordinated behavioral care excellence from blueBriX
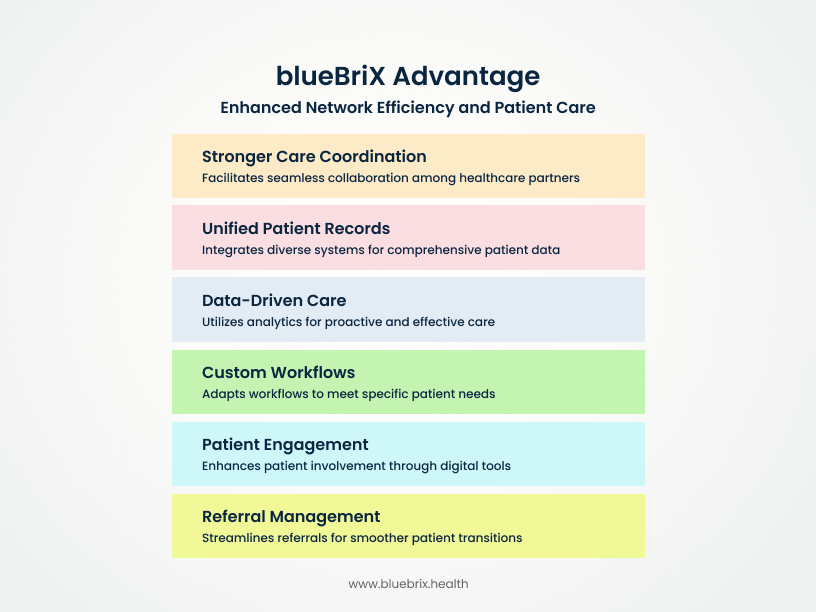
At blueBriX, we’ve designed our platform with a deep understanding of these challenges, crafting solutions that empower organizations and their networks to overcome obstacles and excel in delivering truly coordinated behavioral care.
Breaking down silos with a unified platform
- Integrated behavioral health EHR: Imagine a single, comprehensive electronic health record system that centralizes all patient data – from mental health and substance use disorder treatment to physical health and social determinants of health. blueBriX provides this unified view, ensuring that every authorized provider in a network has immediate access to a complete, up-to-date patient history. Our EHR is built for the nuances of behavioral health, offering customizable workflows that adapt to clinical needs, not the other way around. This means less time wrestling with generic systems and more time focusing on what matters most: patients.
- Robust Interoperability: We recognize that these networks don’t exist in a vacuum. blueBriX is built on open standards like HL7 and FHIR, ensuring seamless, secure data exchange with other healthcare systems – be it primary care EHRs, hospitals, or social service agencies. Our platform acts as a central hub, connecting all applications and integrations, effectively eliminating manual data entry, reducing errors, and ensuring that critical information flows freely and securely across the entire network. This is the foundation of true coordinated care.
Together, these capabilities break down the silos and fragmented data that derail whole-person care.
Streamlining operations and empowering your workforce
Intelligent care coordination platform: Forget endless phone calls and scattered notes. blueBriX provides a dynamic care coordination platform with customizable dashboards that offer immediate, real-time visibility into patient progress across their entire journey. Our automated referral management system ensures that no patient “falls through the cracks,” with real-time tracking, automated follow-up alerts, and secure communication channels with external providers. Smart task routing keeps care teams aligned, reducing administrative burden and ensuring efficient, proactive patient management.
Automated workflows & no-code customization: We believe technology should work for the provider, not the other way around. Our platform features a no-code app builder, allowing teams to easily build and adapt workflows without needing specialized IT knowledge. This means automated scheduling, appointment reminders, and routine outreach can be set up quickly, freeing up staff to focus on higher-value activities. With purpose-built templates for behavioral health documentation (e.g., streamlined group therapy notes), blueBriX simplifies charting and ensures compliance, giving clinicians more time for direct patient care and reducing burnout.
In doing so, blueBriX eliminates the burden of manual processes and administrative overload that steal time from patients.
Driving superior patient engagement and outcomes
- Comprehensive patient engagement suite: Empowering patients is key to better outcomes. blueBriX offers a full suite of patient engagement tools, including secure patient portals and mobile apps that allow individuals to access their health information, track their progress, and communicate securely with their care team. Our remote patient monitoring (RPM) capabilities facilitate continuous care and early intervention, extending reach beyond the clinic walls. Personalized reminders and digital intake forms enhance patient adherence and streamline administrative processes, fostering a more collaborative and informed patient journey.
- AI-powered clinical decision support & care planning: Leverage the power of data to make smarter, more informed clinical decisions. blueBriX uses AI agents to optimize workflows, provide intelligent clinical decision support, and enhance care planning. Our predictive analytics tools can help identify at-risk populations, enabling proactive interventions and preventive care. With flexible, dynamic treatment plans that adapt in real-time to evolving patient needs, interventions can always be precise and impactful.
These tools directly address the challenge of engaging patients as active, informed partners in their own care.
Achieving financial health and regulatory confidence
- Optimized revenue cycle management: blueBriX simplifies revenue cycle management with automated claims generation, robust eligibility verification, and streamlined denial management. Our platform provides audit-ready reporting, helping organizations navigate complex billing models – whether fee-for-service, capitation, or various value-based contracts – with confidence. This ensures they get paid efficiently for the high-quality, coordinated care they deliver.
- Built-in compliance & security: Data security and regulatory compliance are non-negotiable, especially with sensitive behavioral health information. blueBriX is engineered with end-to-end HIPAA compliance, secure audit trails, and automated alerts to keep data safe and operations compliant. We provide robust consent management tailored specifically for behavioral health data (like CFR 42 Part 2 requirements) and comprehensive disaster recovery plans, giving networks peace of mind.
This equips providers to thrive under value-based care models while staying ahead of compliance demands.
Why technology is no longer optional, but essential
Technology plays a big role in helping CBC achieve its mission. Here’s how it makes a difference:
- Keeps everyone connected: CBC works with over 50 partner organizations. Technology helps all these providers stay in sync—making it easier to share updates, make referrals, and coordinate care for people with complex needs.
- Looks at the whole person: Good care means understanding both medical and social needs—like housing, food, or mental health. Technology helps collect and share this information so that every part of a person’s life is considered in their care.
- Uses what works: CBC relies on proven care models. Technology helps track what’s working and where changes are needed, so the best approaches can be used across the network.
- Expands access to care: Tools like telehealth, digital records, and online resources help more people—especially those in remote areas or with limited mobility—get the care they need, when they need it.
- Makes work easier and smarter: Technology can handle routine tasks, track outcomes, and simplify paperwork. This gives care teams more time to focus on helping people directly.
- Keeps CBC flexible: The world is always changing. With the right tech, CBC can adapt quickly, roll out new services, and meet people’s needs in real-time.