Preventive care is all about identifying potential health issues early to keep costs down and outcomes better, perfectly in line with the principles of value-based care. For instance, research shows that every $1 spent on preventive care saves approximately $2.20 in healthcare costs by reducing hospitalizations and managing chronic diseases earlier. In this blog, we’ll dive into some exciting strategies that are taking preventive care to the next level. We’ll also explore how providers can tap into advanced technologies and streamlined care coordination to deliver patient-centered preventive care. The goal? To promote health equity, ensure proactive care delivery, and make healthcare more effective and accessible for everyone. Let’s unpack these impactful strategies together!
Imagine a healthcare system that focuses on keeping you healthy in the first place, rather than just stepping in when you’re sick. That’s the heart of value-based care. It’s a proactive approach where patients are empowered to take charge of their health, and healthcare providers work on strategies to prevent issues before they arise. The result? Fewer health problems, lower costs, and a win-win for everyone involved.
Value-based care policies are pivotal in shifting the norm from reactive, illness-focused care to proactive well-being. By incentivizing prevention and early intervention, these policies lay the groundwork for a healthcare system designed to address risk factors and promote long-term health outcomes. This transformation from treating sickness to promoting well-being encourages providers to focus on keeping patients healthy, rather than solely treating them when problems occur.
By shifting from reactive care to a proactive mindset, value-based care tackles risk factors early, stopping potential problems from snowballing into serious conditions. This boosts patients’ overall well-being and slashes the need for expensive treatments and hospital stays. But here’s the big question: as healthcare organizations transition to this model, how do they integrate preventive measures without throwing their day-to-day operations off balance?
In this blog, we explore some of the proven preventive strategies that providers can consider implementing at their organizations with the help of the right digital health tools. blueBriX is here to equip healthcare providers with tailored technology solutions for value-based care that don’t just improve patient outcomes but also keep financial performance strong and satisfaction scores soaring. Let’s explore!
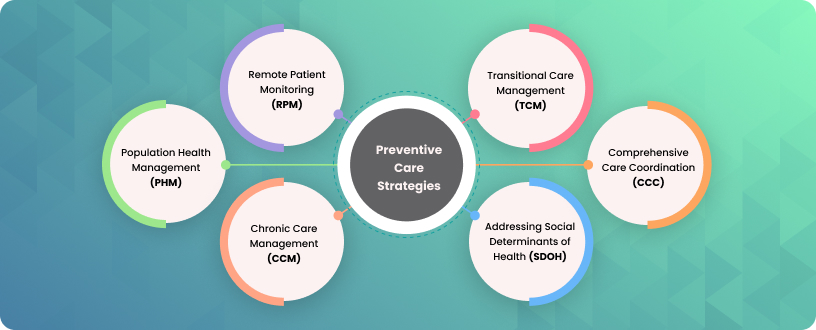
Effective Prevention Techniques in Value-Based Models
The key to success for value-based healthcare organizations lies in weaving preventive care into every step of patient management. Whether it’s through early screenings or lifestyle interventions, prevention not only improves the quality of care but also builds stronger patient relationships and supports long-term wellness.
In this blog, we’ll dive into six essential preventive care strategies that healthcare organizations can use to thrive in value-based models. These strategies are interconnected, working together to create a comprehensive approach where prevention takes center stage in delivering quality care. This approach not only improves patients’ well-being but also reduces the need for costly treatments and hospitalizations.
Let’s uncover how these strategies can shape a healthier future together!
Remote Patient Monitoring (RPM)

Remote patient monitoring (RPM) is changing the game in healthcare by using technology to keep track of patients’ health outside the traditional clinic or hospital setting. It’s like having a continuous check-in on chronic conditions and overall wellness, no matter where the patient is. With real-time insights, RPM helps spot potential health issues early, empowers patients to take charge of their health, and reduces the chances of hospital readmissions.
For organizations focused on value-based care, RPM is a win-win. It not only boosts efficiency but also improves care quality, lowers costs, and ensures timely interventions that align perfectly with value-based payment models. By tapping into the data RPM provides, healthcare providers can create personalized health plans, track how well patients stick to treatment protocols, and encourage proactive health habits. The result? Better outcomes for individuals and stronger population health overall.
Transitional Care Management (TCM)

Leaving the hospital should feel like a big step toward recovery, but for many patients, it can be a tricky time filled with uncertainty. That’s where Transitional Care Management (TCM) comes in, acting as a crucial safety net to guide patients through this vulnerable phase. Think of it as a bridge that connects the care you received in the hospital to the care you need at home. Whether it’s arranging follow-up visits, managing medications, or coordinating home care, TCM ensures that no patient falls through the cracks.
Essentially, TCM focuses on the first 30 days after a patient leaves an acute care setting, like a hospital. It’s all about smoothing out the transition, reducing preventable readmissions, catching potential medical errors, and addressing common gaps in care. For value-based care organizations, TCM is a game-changer. It boosts patient satisfaction, keeps them engaged, and aligns perfectly with performance-based goals by improving health outcomes and cutting down unnecessary healthcare costs.
The key to effective TCM is planning. Identifying high-risk patients, prioritizing timely outreach, scheduling follow-ups, and tailoring care plans to meet each patient’s specific needs are all essential strategies. When done right, TCM ensures continuity of care, enhances patient outcomes, and supports the overall success of value-based care models.
Population Health Management (PHM)

Population Health Management (PHM) employs a smart, data-driven approach to improving the health of specific groups by focusing on tailored care, analytics, and coordination. A key component of PHM is risk stratification, which involves systematically categorizing patients based on their health status and other factors. This process enables providers to identify the right level of care and services for distinct subgroups of patients, ensuring that resources are allocated efficiently and effectively. This allows healthcare providers to address the population’s needs through early interventions such as screenings, vaccinations, and lifestyle changes preventing chronic illnesses and keeping people healthier. For example, preventive services like lifestyle advice, screening tests to detect asymptomatic disease, and vaccinations are essential components of PHM.
For value-based care organizations, PHM reduces unnecessary healthcare use, improves patient satisfaction, and drives better health outcomes—all while keeping costs in check. The key is leveraging data to segment populations, prioritize high-risk patients, and deliver personalized, evidence-based care that focuses on prevention and holistic wellness. Community-based tools like remote monitoring, personalized coaching, and medication support play a big role in identifying health issues early. This proactive approach tackles the root causes of frequent hospital visits, improves individual and community health, and lowers long-term healthcare costs.
With technologies like blueBriX, providers gain the tools to analyze data effectively and design patient-centered care strategies. The result? Better health outcomes for patients and improved financial and operational performance for healthcare organizations.
Chronic Care Management (CCM)
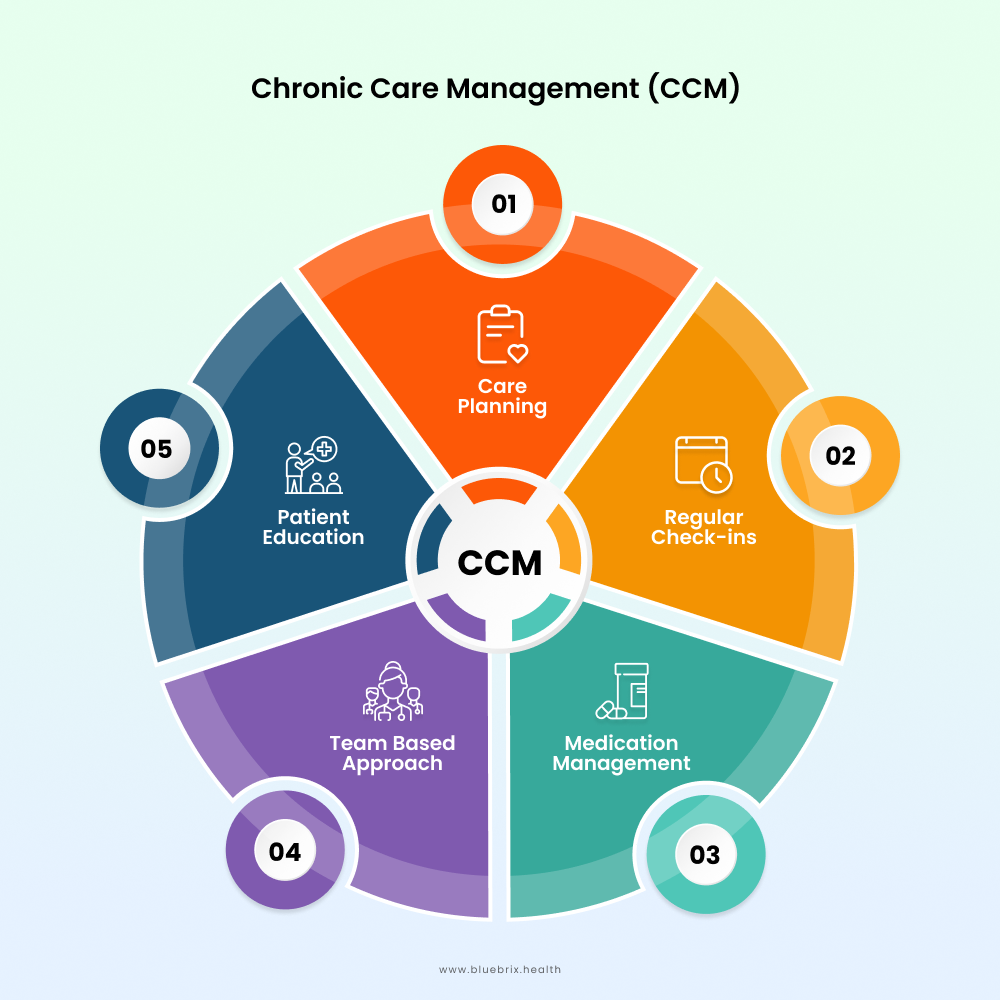
Chronic Care Management (CCM) is vital in supporting people living with two or more chronic conditions, such as diabetes, hypertension, asthma, arthritis, or heart disease. These conditions often last a year or longer and managing them requires more than just occasional doctor’s visits. That’s where CCM steps in—it’s all about providing ongoing, coordinated care to keep patients healthier and prevent complications.
CCM helps by focusing on early interventions, managing risk factors, and slowing the progression of chronic illnesses. Services like remote patient monitoring, medication management, and personalized care plans make it easier for patients to stay on track and for providers to deliver consistent care.
For value-based care organizations, CCM is a win-win. It improves patient outcomes, reduces hospital readmissions, and aligns perfectly with reimbursement models that reward quality care and cost-efficiency. By using tools like comprehensive care plans, patient engagement technology, and seamless coordination across providers, healthcare teams can offer proactive, holistic management that benefits everyone involved.
In short, CCM isn’t just about managing chronic conditions—it’s about empowering patients, enhancing care quality, and creating a sustainable path forward in today’s healthcare landscape.
Addressing Social Determinants of Health (SDOH)
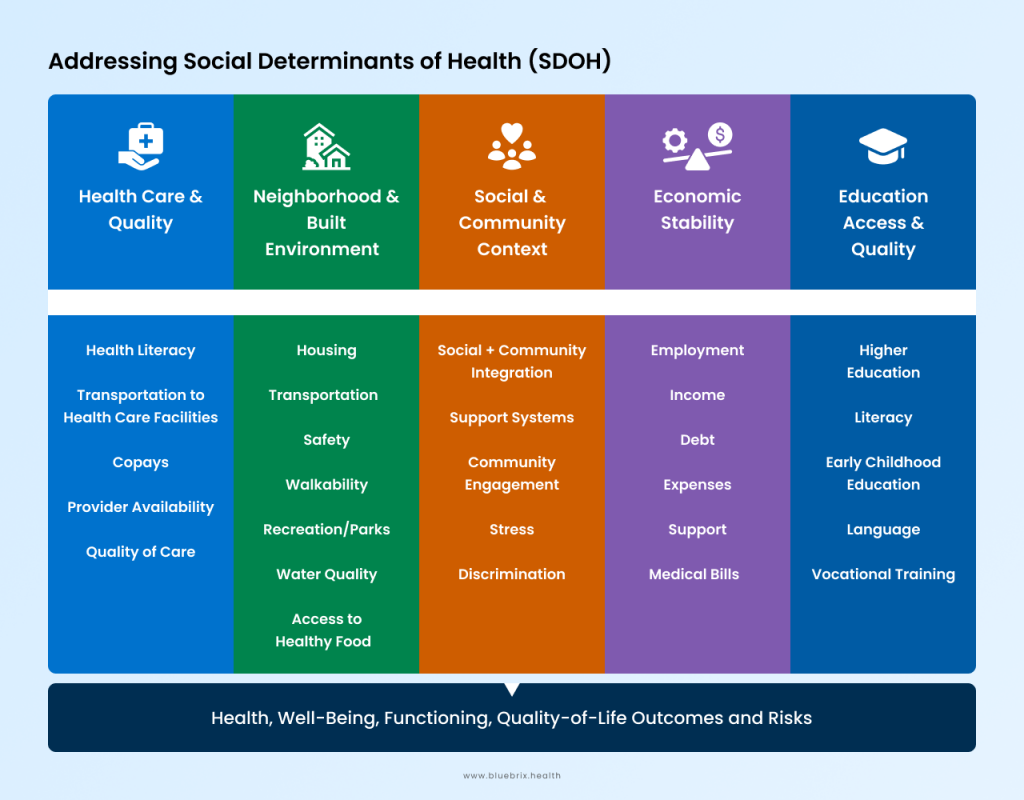
Social Determinants of Health (SDOH) — the non-medical factors that can shape your health, such as your income, education, living environment, housing stability, transportation access, food security, and healthcare availability all play a big role in your health. These factors can make a huge difference in whether someone can keep up with preventive care, like regular screenings, vaccinations, or check-ups.
Addressing SDOH is critical for creating a fairer healthcare system. By identifying and tackling the barriers people face, providers can promote health equity and help patients stay healthier in the long run. For example, patients in underserved areas often struggle to access preventive services, which leads to delayed diagnoses and higher medical costs. Value-based care organizations, in particular, see big benefits by focusing on SDOH—they can cut costs, improve outcomes, and address the root causes of health disparities, which drive up to 80% of health outcomes.
Integrating SDOH into care strategies is all about being proactive. It starts with identifying at-risk groups, targeting interventions, and allocating resources where they’re needed most. Tools like the Plan-Do-Study-Act (PDSA) framework and digital health solutions make it easier to pinpoint social risks and connect patients to the right community resources.
By addressing these challenges head-on, providers can improve individual and community health, reduce costs, and meet the goals of value-based care. It’s not just about delivering care—it’s about creating a system that works for everyone.
Comprehensive Care Coordination

Let’s talk about care coordination and why it’s so important, especially for preventive care and value-based care models. At its core, effective care coordination is about teamwork—getting primary care doctors, specialists, home care providers, and even community resources to work together smoothly. This kind of collaboration ensures patients get the right care at the right time, closing gaps in treatment and reducing the risk of medical errors.
In simple terms, care coordination means organizing all aspects of a patient’s care and making sure everyone involved is on the same page. When done right, it improves preventive care by ensuring timely screenings, helping manage chronic conditions, and addressing health risks early. The result? Fewer complications, fewer hospital visits, and healthier patients overall.
For organizations focused on value-based care, care coordination is a game-changer. It cuts down on unnecessary tests, boosts efficiency, and improves patient satisfaction—all while keeping costs in check. How do providers make it happen? By building integrated care teams, using digital tools for real-time communication, and creating personalized care plans that factor in patients’ unique needs and social challenges.
Care coordination tools are also key. They help identify what kind of support each patient needs, assign clear roles to the care team, and ensure everyone is accountable for delivering the best outcomes. Ultimately, it’s about creating a system that’s not just efficient but also equitable and patient-centered. When the entire healthcare team is aligned, everyone wins—especially the patient.
Get Proactive, Emphasize on Preventive Care
As healthcare moves toward value-based care, stepping up preventive care strategies has become more important than ever. Think of the basics—regular check-ups, vaccinations, cancer screenings like mammograms and pap smears, cholesterol tests, and blood pressure or diabetes screenings. Pair those with counseling on healthier lifestyle choices, such as quitting smoking, managing stress, and maintaining a balanced diet, and you’ve got the foundation for proactive healthcare.
But here’s the thing—these traditional methods become even more powerful when combined with advanced tools and strategies like Remote Patient Monitoring (RPM), Transitional Care, Chronic Care Management, Population Health Management, Social Determinants of Health (SDOH), and Comprehensive Care Coordination. Together, they enable providers to shift from simply reacting to health problems to delivering truly value-based care.
And let’s not forget the critical role of technology in this transformation. Scalable, adaptable, and interoperable digital health solutions are the backbone of modern preventive care. These tools allow healthcare providers to seamlessly integrate patient data, manage complex care delivery systems, and connect with diverse patient populations in meaningful ways. The result? Closing care gaps, improving patient outcomes, and reducing costs.
blueBriX is leading the charge in this space, offering innovative solutions that empower healthcare providers to stay ahead in value-based care. With the right tools and strategies, organizations can transform how care is delivered—making it more proactive, patient-centered, and effective.