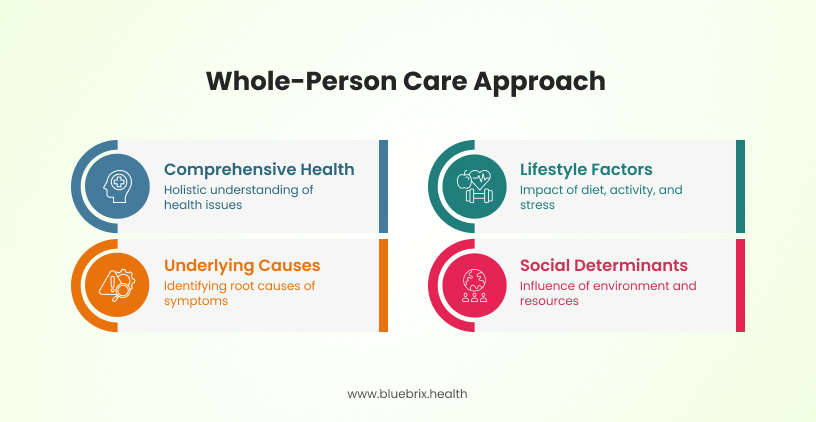
Modern healthcare has recognized that our well-being isn’t solely defined by physical health and the fragmented approach in traditional healthcare leads to less-than-optimal outcomes. Enter whole person care, a transformative model that integrates behavioral health into primary care settings. By considering the complete spectrum of a patient’s needs—physical, mental, emotional, and social—whole-person care aims to provide more comprehensive and effective healthcare.
The importance of whole-person care
Whole-person care goes beyond treating isolated symptoms—it focuses on identifying and addressing the underlying causes of health issues. Instead of solely managing symptoms, this approach looks “upstream” to uncover contributing factors, ensuring that patients receive comprehensive, long-term solutions rather than “temporary fixes”.
While certain factors like genetics and biology are beyond our control, lifestyle choices and behavioral factors play a significant role in overall health. Elements such as diet, physical activity, stress levels, and sleep quality have a direct impact on well-being. Additionally, a person’s social determinants of health—including their living and working environments, socioeconomic status, and access to resources—can shape health outcomes. By promoting self-care, healthy habits, and behavioral interventions, individuals can optimize their health—even when managing chronic conditions.
For instance, symptoms like nausea, constipation, diarrhea, and cramping may not just be isolated digestive issues but could stem from anxiety, hormonal imbalances, food intolerances, or infections. The whole-person care approach does not simply involve prescribing anti-emetics medication or laxative; instead, healthcare providers assess broader factors that may be influencing these symptoms and develop a holistic treatment plan that addresses root causes.
A notable example of this approach is the Whole Health Action Management (WHAM) program. WHAM is a peer-led intervention designed to promote self-management and resiliency among individuals with mental illnesses, substance use disorders, and chronic physical health conditions. The program focuses on various health factors, including stress management, healthy eating, physical activity, and building support networks. Participants receive training to set and achieve whole health goals, fostering a sense of empowerment and proactive health management.
Implementing whole person care models like WHAM has demonstrated significant benefits:
- Enhanced patient activation: Participants exhibit increased confidence in managing their health responsibilities, leading to more effective self-care practices.
- Improved general health: Self-reported health outcomes improve notably, with many participants experiencing better overall health.
- Increased optimism and confidence: There’s a marked improvement in hopefulness and optimism among participants, contributing to better mental well-being.
- Higher employment rates: Participants are more likely to secure employment, indicating broader life improvements associated with the program.
These outcomes highlight the efficacy of whole person care models in enhancing patient engagement, health outcomes, and socioeconomic status. By integrating such approaches into healthcare systems, providers can better align with value-based care principles, ultimately leading to more sustainable and effective healthcare delivery.
The growing need for integrated behavioral health
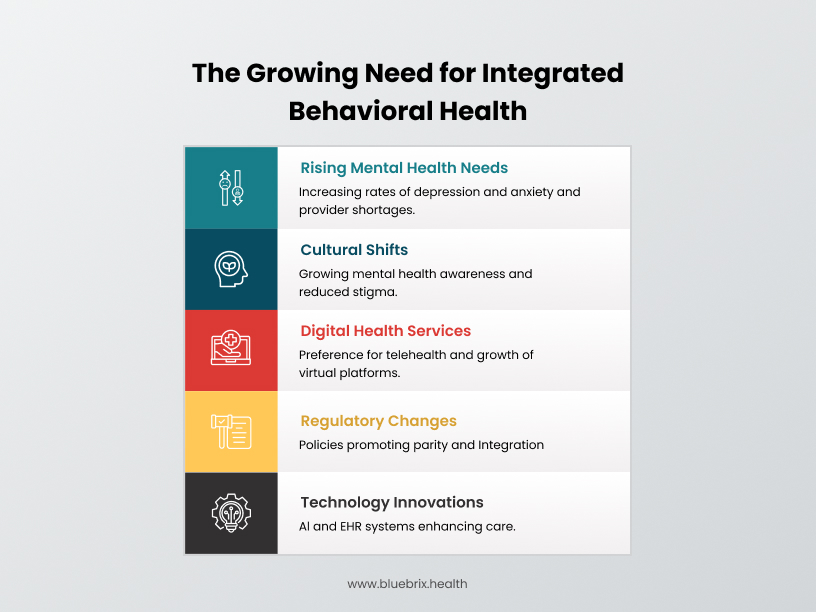
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), one in five U.S. adults experiences a clinically significant mental health or substance use disorder. Additionally, mental health conditions among children and adolescents have risen sharply in prevalence and severity. Yet, why do so many people struggle to get mental health care?
A promising solution to bridge this gap—particularly for those with mild to moderate conditions—is behavioral health integration. A 2020 RAND study, conducted in collaboration with the American Medical Association (AMA), highlights the potential of integrating behavioral health into primary care as a means to expand access, improve outcomes, and enhance overall patient care.
What’s driving the shift?
1. Rising mental health needs
- Depression and anxiety rates have surged by 25% since the pandemic (World Health Organization).
- Shortage of mental health providers—there are only 30 psychologists per 100,000 people in the U.S., creating massive care gaps.
2. Cultural shifts toward mental health awareness
- Google searches for “mental health help” increased 60% in the past three years.
- Social media influencers and athletes openly discussing mental health have reduced stigma, encouraging more people to seek care.
3. Expansion of digital health services
- 75% of young adults prefer telehealth for mental health support (American Telemedicine Association).
- Virtual mental health platforms like Talkspace and BetterHelp have seen 400% growth since 2020, highlighting demand for digital-first care.
4. Regulatory & policy changes
- The 2024 Mental health parity and addiction equity act (MHPAEA) mandates insurers to provide equal access to mental and physical healthcare.
- CMS’s Making Care Primary (MCP) Model incentivizes behavioral health integration with value-based reimbursement programs.
5. Technology-driven innovation
- AI-powered clinical decision support improves diagnosis accuracy and care coordination.
- Interoperable EHR systems reduce administrative burden, making integration seamless.
The growing need for integrated behavioral health
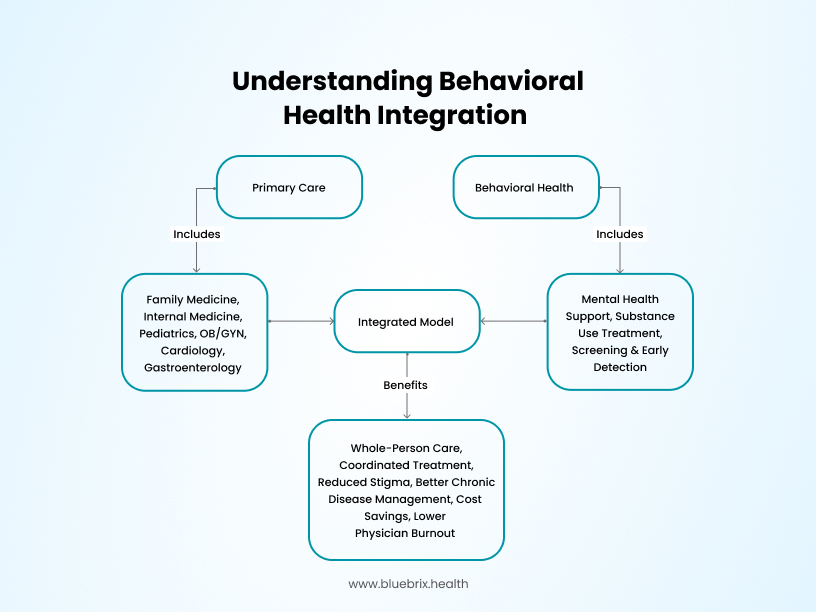
Understanding behavioral health integration
Primary care physicians (PCPs) are often the first to recognize behavioral health concerns, and in an integrated model, they can immediately connect patients to appropriate mental health support—often within the same clinic. A combination of cultural, regulatory, and technological advancements is driving the need for integrating mental health, crisis management, and addiction services into primary care.
Behavioral health integration (BHI) brings together primary care teams and behavioral health professionals to deliver comprehensive, patient-centered care through a structured approach. This integration can be applied across various healthcare settings, including family medicine, internal medicine, pediatrics, obstetrics and gynecology, as well as specialty areas such as cardiology and gastroenterology.
Why it works:
- Eliminates referral delays: On average, patients wait 25 days to see a mental health provider. With Behavioral health integration , they receive behavioral health support during primary care visits, preventing long delays.
- Reduces provider burnout: 60% of primary care physicians report burnout due to managing behavioral health cases without support. Collaborative care models distribute workload effectively.
- Improves chronic disease management: 40% of patients with chronic conditions also have mental health concerns, making integrated care essential for better outcomes.
- Lowers healthcare costs: A study in Utah found that BHI implementation resulted in $115 per patient per year in cost savings and a 76% reduction in unnecessary primary care visits.
Behavioral health integration is like having a team of doctors working together, making sure patients get whole person care without delays or gaps. Research has shown that embedding behavioral health within primary care settings can lead to improved depression outcomes, increased treatment adherence, reduced healthcare costs, and lower physician burnout.
Integrated behavioral health in primary care: Clinical, operational, and financial advantages
Integrating behavioral health into primary care represents a transformational shift in healthcare delivery. Behavioral health integration delivers significant clinical, operational, and financial benefits helping practices reduce overall utilization, increase revenue, and enhance patient satisfaction. While implementation can present challenges, technology-driven solutions can streamline workflows, improve care coordination, and maximize financial performance.
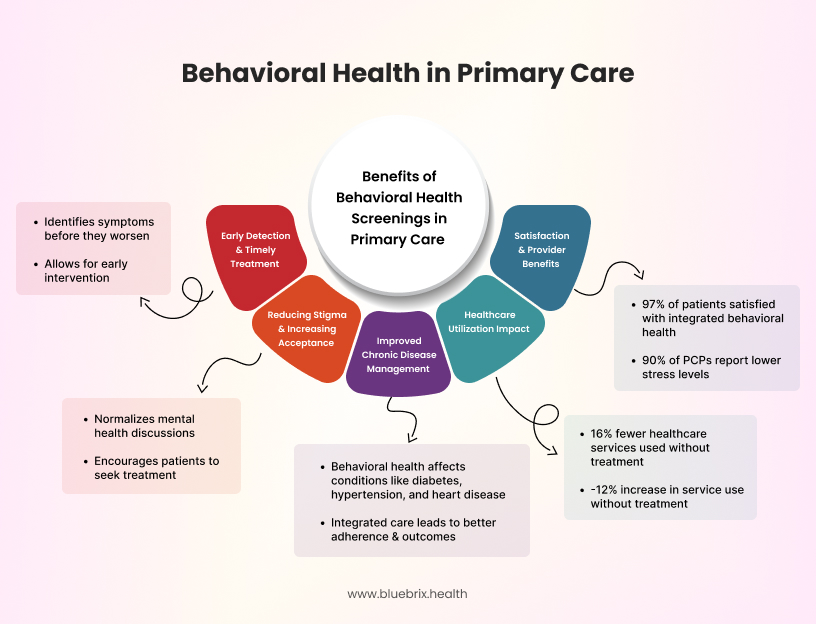
Clinical benefits: Improving patient outcomes
Integrating behavioral health into primary care allows for earlier diagnosis and intervention, leading to improved patient outcomes. Studies show that:
- Patients in integrated care models see higher rates of depression remission, as they receive timely treatment through collaborative care.
- Behavioral Health Integration reduces emergency department visits and hospitalizations by providing proactive mental health interventions.
- Patients with chronic conditions (diabetes, hypertension, heart disease) experience improved health management when behavioral health is addressed within primary care.
Operational benefits: Enhancing efficiency & care coordination
Behavioral Health Integration improves provider workflows, reduces administrative burdens, and enhances care coordination. Key operational advantages include:
- Less time spent on documentation & compliance tracking through automation.
- Streamlined provider workflows, allowing primary care teams to integrate behavioral health screenings into existing EHR workflows.
- Enhanced care coordination between PCPs, behavioral health specialists, and case managers, ensuring that patients receive the right care at the right time.
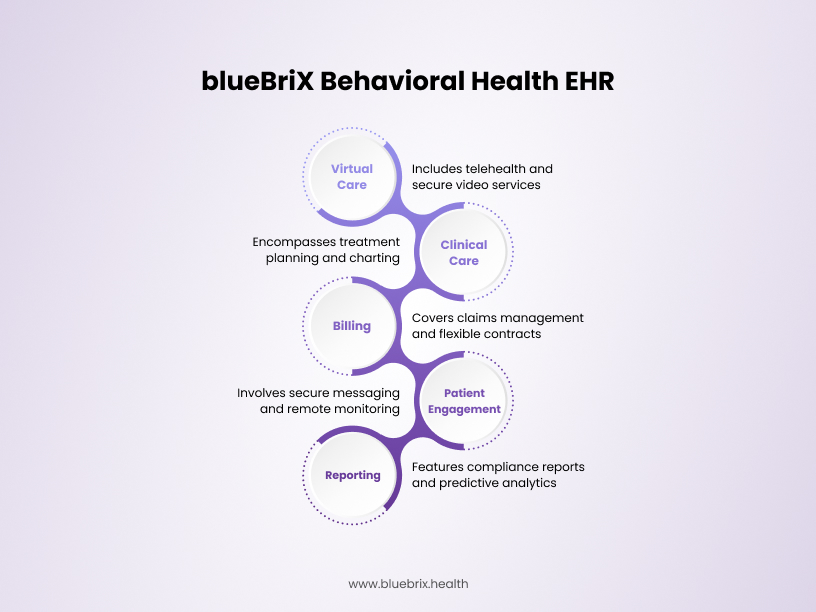
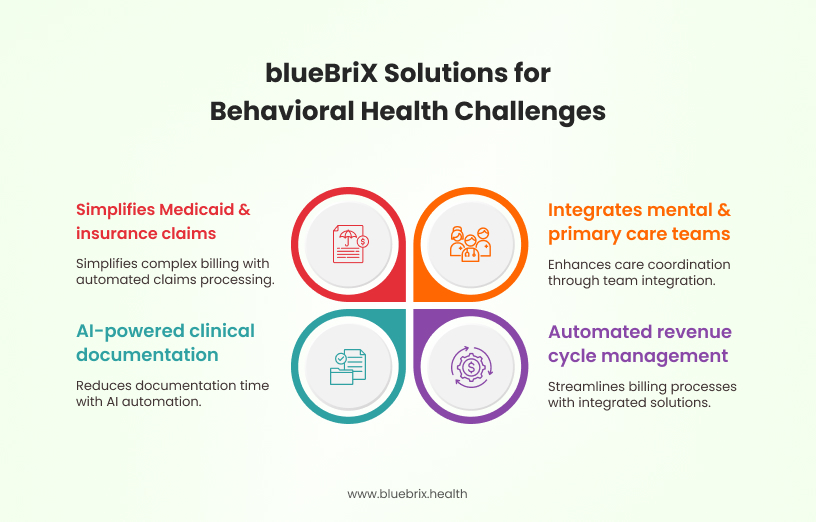
Additionally, specialized digital health tools such as blueBriX offers:
- Clinical decision support tools to assist primary care providers (PCPs) in making informed behavioral health decisions.
- Secure information exchange, enabling seamless interoperability between medical and behavioral health professionals.
- Medication-Assisted Treatment (MAT) support, helping manage substance use disorders within primary care settings.
Financial benefits: Driving revenue growth & maximizing reimbursements
Integrating behavioral health not only improves patient care but also optimizes financial performance for providers. Practices can benefit from:
- Higher reimbursement rates through Behavioral Health Integration-specific billing codes (CPT 99484, 99492, 99493, and 99494), allowing primary care providers to bill for behavioral health management.
- Reduced claim denials—practices using automated Medicaid billing solutions see a 30% reduction in rejected claims.
- Lower overall healthcare costs—a Salt Lake City study found that BHI implementation resulted in $115 per patient per year in cost savings and a 76% decrease in unnecessary primary care visits.
By leveraging value-based care models, providers can receive performance-based incentives for improved behavioral health outcomes, such as:
- Depression remission rates tied to reimbursement bonuses under CMS’s Making Care Primary (MCP) model.
- Additional funding opportunities for practices that enhance care coordination and adopt behavioral health screening as part of primary care.
Optimizing integrated behavioral health through technology: Three things to consider
Successfully implementing integrated behavioral health requires comprehensive technological solutions that enable practices to identify patients in need, coordinate care, track outcomes, and document encounters for accurate reimbursement. Also ensuring compliance with CCBHC, HIPAA, and Medicaid reporting is a major challenge for providers. blueBriX automates compliance tracking, simplifying audits and reimbursement submissions.
How does technology improve behavioral health integration?
If you’re thinking about integrating behavioral health, your Electronic Health Record is a great place to start, providing tools for tracking patients’ behavioral health journeys, managing referrals, facilitating communication across care teams, supporting patient education, and automating follow-up reminders.
Beyond EHRs, specialized healthcare software can enhance integrated care by offering:
- Clinical decision support to assist primary care providers.
- Self-management tools that empower patients.
- Secure information exchanges that enhance provider collaboration.
- Support for medication-assisted treatment (MAT) tailored to behavioral health needs.
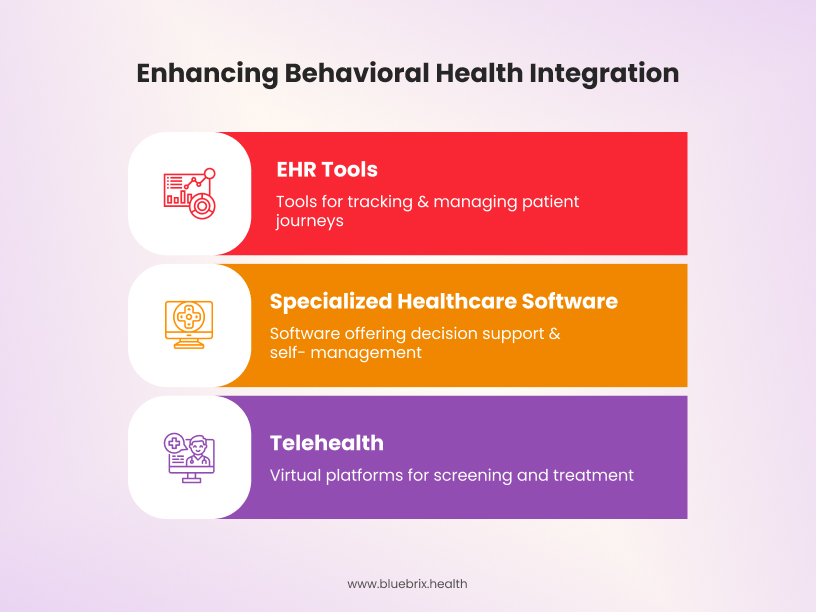
Additionally, the AMA emphasizes telehealth’s role in making BHI more accessible. Virtual platforms enable screening, education, treatment, and care coordination, ensuring wider patient reach and improved engagement.
When evaluating clinical workflow software to support behavioral health integration, consider these key factors:
Enhancing impact: Early identification and improved care coordination
Traditional electronic health record systems often present challenges in behavioral health integration. Many have fragmented screening tools, making it difficult to efficiently assess and track patients. Additionally, most Electronic Health Records are not built to document behavioral health treatments and outcomes effectively.
Expanding preventive behavioral health screenings
Preventive screenings for chronic diseases like diabetes and hypertension are standard practice in primary care—yet behavioral health screenings remain underutilized. This reactive approach results in delayed treatment, allowing mental health conditions to worsen before intervention.
With an integrated behavioral health model, PCPs have access to tools and support to routinely screen for behavioral health concerns, leading to earlier detection and improved patient outcomes.
Reducing delays in behavioral health treatment
Accessing a behavioral health specialist can take weeks or even months due to provider shortages, scheduling barriers, and insurance challenges. Integrated behavioral health eliminates these roadblocks by allowing patients to begin treatment within their PCP’s office. This faster access to care ensures that patients receive immediate support, improving treatment adherence and long-term recovery rates.
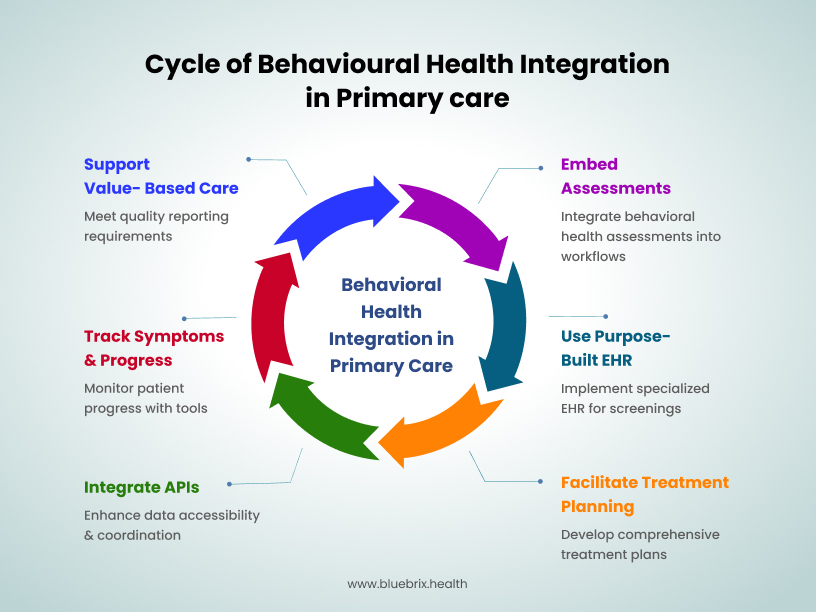
Supporting primary care: Behavioral health measurement and follow-up
Embedding behavioral health assessments directly within clinical workflows eliminates the need for providers to navigate multiple applications, allowing for seamless integration into routine care. A Behavioral Health EHR solution can streamline early screening for behavioral health conditions, providing a comprehensive view of how mental and physical health intersect. This facilitates more effective treatment planning and enables clinicians to deliver whole person care. blueBriX utilizes application programming interfaces (APIs) to integrate seamlessly with existing Electronic Health Records can improve data accessibility and care coordination across providers.
Key features such as symptom tracking tools, severity measurement scales, and functional impairment assessments help clinicians gain a comprehensive view of a patient’s progress over time. This not only enables data-driven decision-making but also supports quality reporting requirements tied to value-based care models.
Measurement frameworks for behavioral health
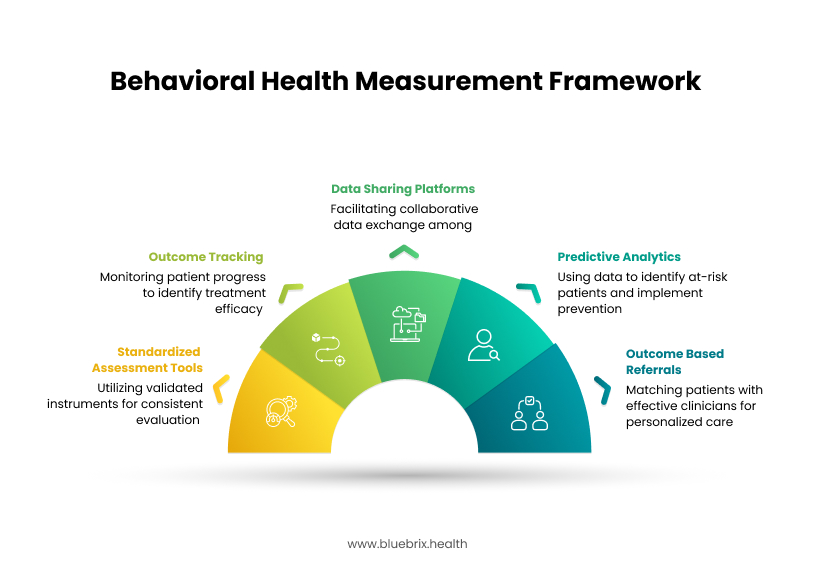
Regardless of whether a value-based care model is administered through Medicare, Medicaid, or private insurers, robust measurement frameworks are critical to success. These frameworks enable healthcare providers to assess, monitor, and enhance the quality of care, ensuring comprehensive attention to both mental and physical health aspects. By tracking clinical and financial metrics, providers maintain accountability in delivering high-quality care, patients experience measurable improvements in behavioral health outcomes, and payers and providers align on shared incentives, fostering a more effective and sustainable healthcare system.
Key components of measurement frameworks:
- Standardized assessment tools: Utilizing validated instruments, such as the Patient Health Questionnaire-9 (PHQ-9) for depression, allows for consistent evaluation of behavioral health conditions. These tools facilitate accurate clinical assessments and inform treatment planning.
- Outcome tracking: Regular monitoring of patient progress through systematic data collection helps in identifying treatment efficacy and areas needing adjustment. This continuous tracking supports proactive interventions and enhances overall care quality.
- Data sharing platforms: Collaborative platforms like Grid-Enabled Measures (GEM) promote the use of standardized measures and facilitate data sharing among researchers and clinicians. GEM’s web-based system allows for the exchange of harmonized data on behavioral constructs and measures, contributing to improved care strategies.
- Predictive analytics: Advanced measurement frameworks incorporate predictive modeling to identify patients at risk for adverse outcomes, such as hospitalization. By analyzing collected data, healthcare providers can implement preventive measures, thereby improving patient safety and reducing costs.
- Outcome-based referrals: Leveraging outcome data to match patients with clinicians who have demonstrated effectiveness in treating specific conditions ensures personalized and effective care. This approach enhances treatment success rates and patient satisfaction.
Driving value: Documentation for reimbursement and quality reporting
The shift from fee-for-service to value-based care
According to the Health Care Payment Learning & Action Network, approximately 41% of healthcare payments in the U.S. are tied to value-based care arrangements, while 59% remain fee-for-service. However, primary care physicians are lagging behind, with 71% still relying on FFS revenue, as reported by the Commonwealth Fund.
Integrating behavioral health into primary care has been shown to drive better clinical outcomes and cost savings. CMS’s Making Care Primary (MCP) model, introduced in 2023, provides several key benefits to help practices generate revenue while transitioning to value-based care.
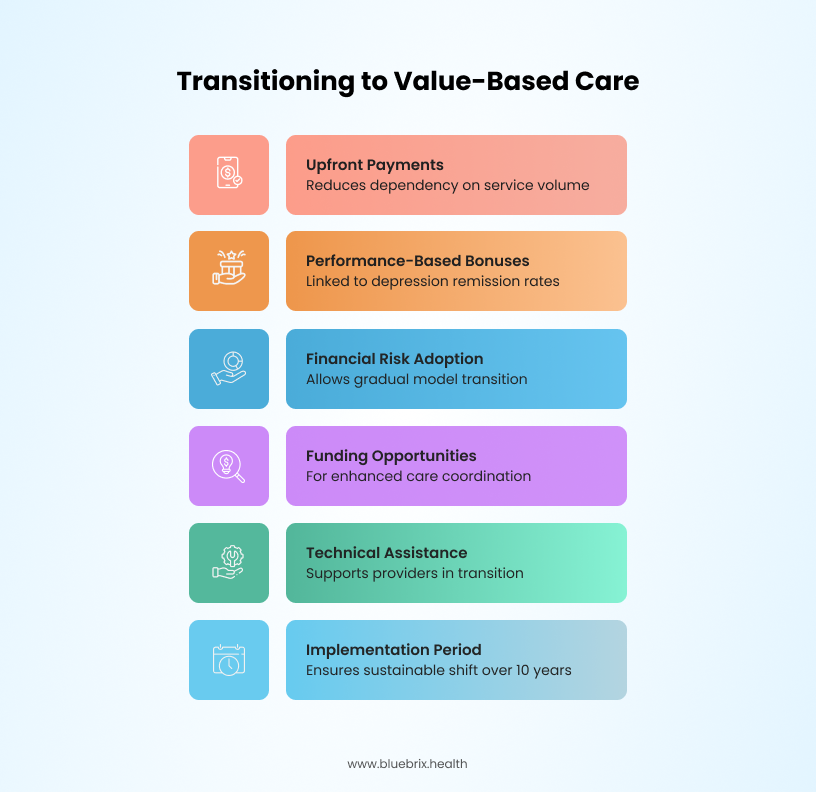
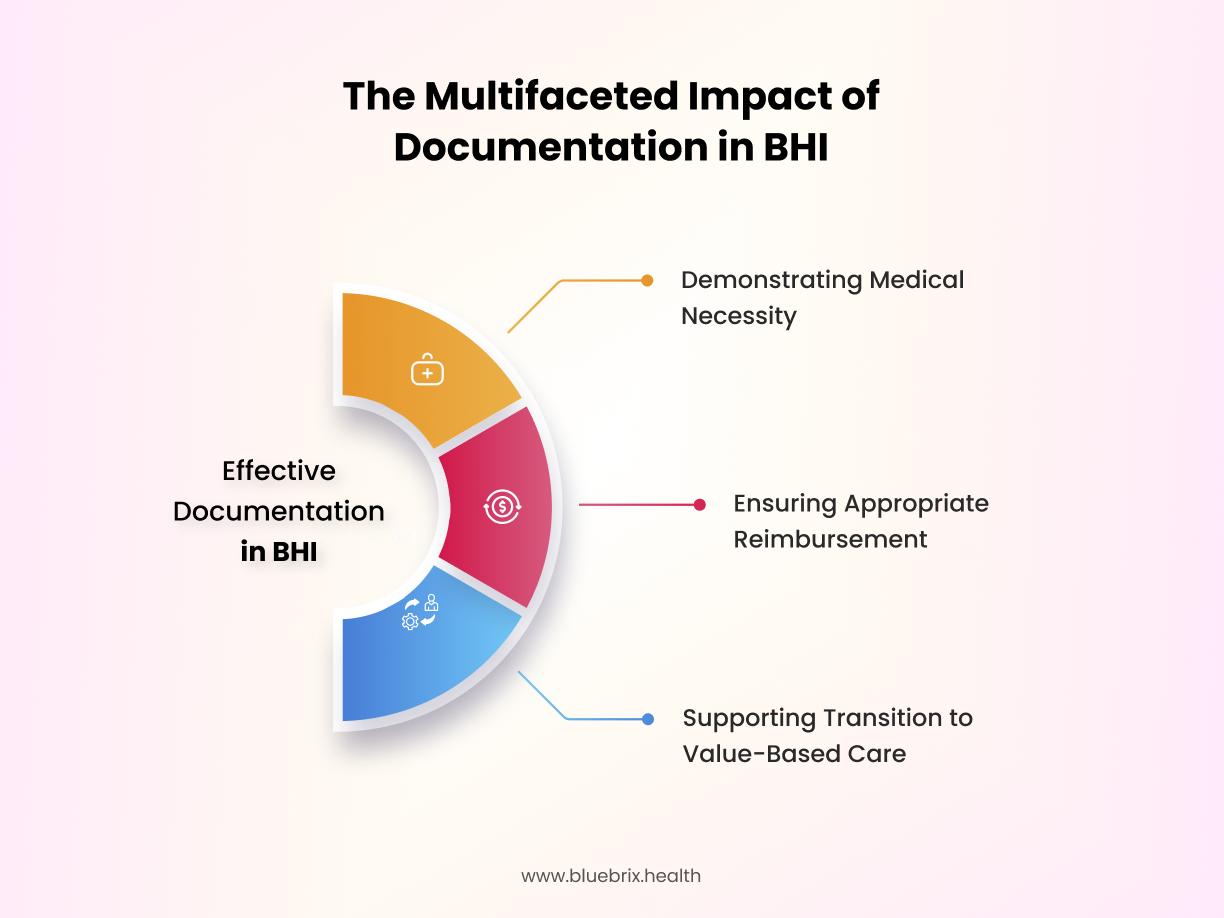
Comprehensive documentation
Effective documentation is the foundation of measurement-based care and plays a crucial role in securing reimbursement for Behavioral Health Integration services. Documentation helps Behavioral Health Integration in the following ways:
- Medical necessity is clearly demonstrated, streamlining the prior authorization process with payers.
- Providers receive appropriate reimbursement for Behavioral Health Integration services, leveraging available billing codes.
- Transitioning to value-based care models is supported, as thorough records of diagnoses, symptoms, and outcomes illustrate the effectiveness of integrated care.
Behavioral health integration as a care management service
Behavioral health has historically been excluded from the broader shift to value-based care due to barriers such as low reimbursement rates, insurance carve-outs, and a lack of parity with other specialties. As a result, a significant portion of behavioral health services are paid out-of-pocket, limiting access for many patients.
Recognizing this gap, CMS introduced new billing codes in 2017 that allow PCPs to bill for Behavioral Health Integration services. These codes cover two primary categories:
- General BHI services
- Collaborative Care Management services
By leveraging these reimbursement opportunities, PCPs can transition toward value-based payment models while expanding access to integrated behavioral healthcare for their patients.
Service type
General BHI services
Billing code: CPT 99484
Monthly care management for patients with behavioral
health conditions
Who Can Bill?
Service type
Collaborative care management (CoCM)
Billing code: CPT 99492
Initial psychiatric collaborative care (first 70 minutes
in a month)
Who Can Bill?
Service type
Collaborative care management (CoCM)
Billing code: CPT 99493
Subsequent psychiatric collaborative care (minimum 60
minutes per month)
Who Can Bill?
Service type
Additional CoCM time
Billing code: CPT 99494
Each additional 30 minutes of psychiatric collaborative
care
Who Can Bill?