AI and remote monitoring are transforming healthcare, but a massive challenge remains. While new technologies are paving the way for personalized, efficient care, a huge roadblock is holding back progress: fragmented patient data. This lack of a unified view is preventing doctors from leveraging these powerful tools to their full potential and keeping patients from receiving the seamless care they deserve. We’re on the cusp of a healthcare revolution, and solving this data dilemma is the key to unlocking its incredible potential.
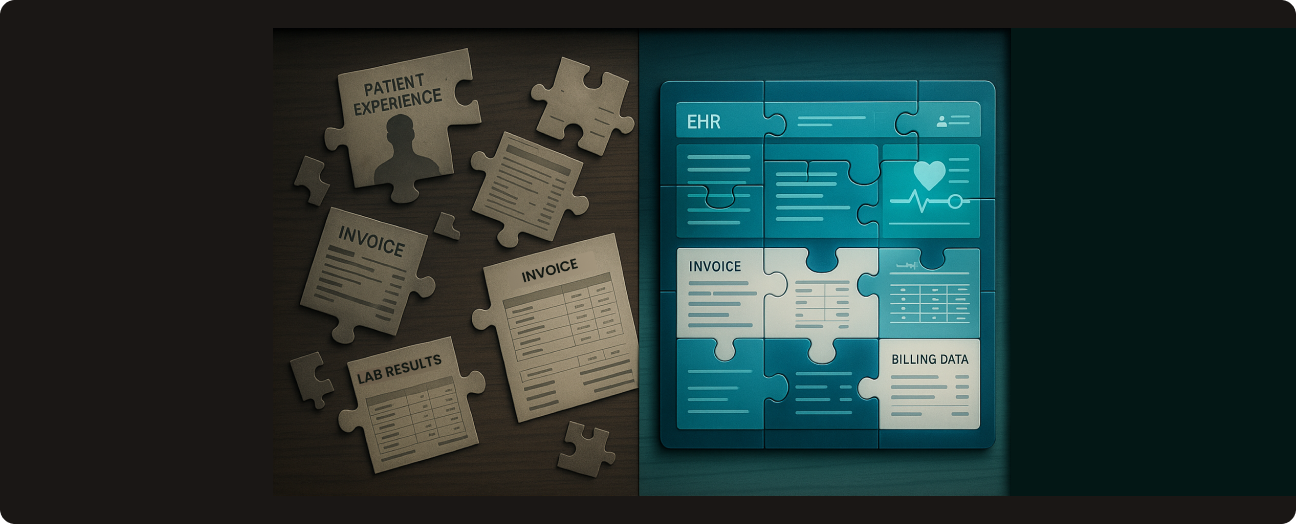
Electronic Health Records were supposed to solve this. And in many ways, they have — clinics and hospitals can now store and manage patient records digitally, making internal processes smoother. But as more and more EHR systems have popped up, especially across large healthcare networks with multiple specialties, a new issue has surfaced: these systems often don’t talk to each other. This creates data silos, where important health information gets stuck in different systems.
This kind of fragmentation is both frustrating and risky. It can affect the safety and quality of care, slow down operations, and increase costs. What healthcare really needs today is not just digital records, but a connected, real-time view of each patient’s full health history.
In this article, we’ll explore the real challenges caused by disconnected EHR systems and show how blueBriX is helping to solve them — creating a more unified, patient-centered healthcare experience.
The pain points of disparate EHR systems
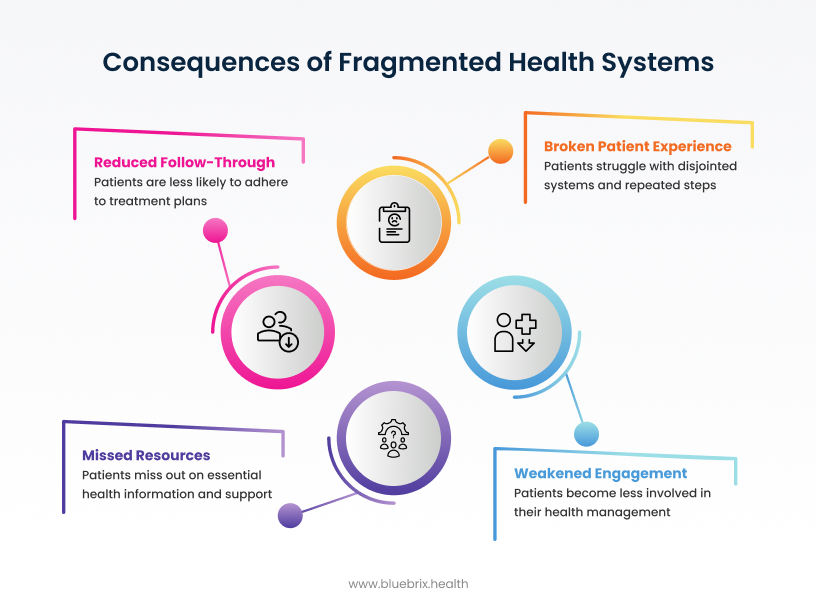
For the Patient: A Disconnected and Frustrating Experience
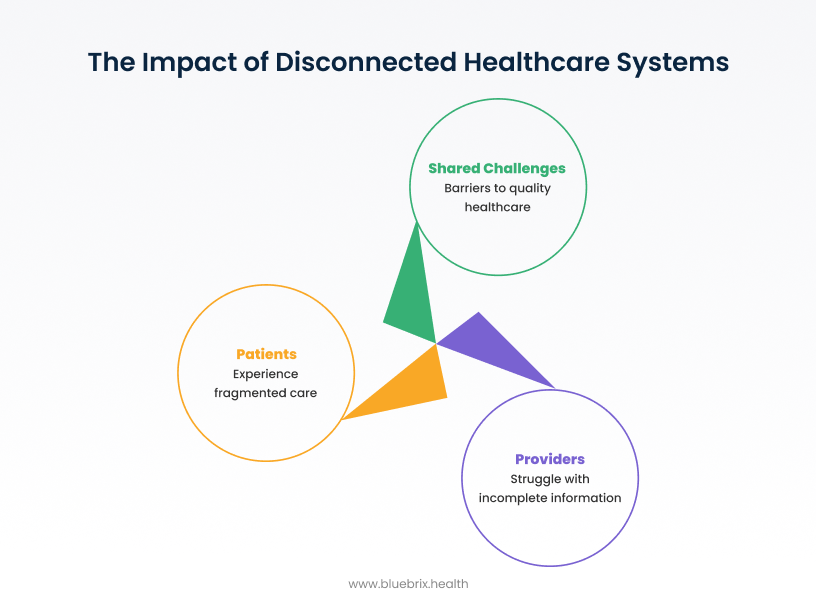
When patients move through a healthcare system that uses different, unconnected platforms, their experience can quickly become frustrating, confusing, and even risky — especially for those dealing with chronic conditions or needing care from multiple specialists.
Let’s take the example of a patient Anthony Edward Stark, to illustrate a common challenge in healthcare today. Anthony is a 50-year-old construction worker who receives care for several health issues. He sees a primary care doctor, a behavioral health specialist, and a cardiologist — all within XYZ Healthcare. The issue? XYZ uses three separate EHR systems across its services. For Anthony, this leads to several challenges:
- Confusing Access to Records: Anthony has to manage different patient portals for each service. Each portal requires its own login and only shows part of his health records. It becomes a guessing game to remember where his heart test results are stored versus his therapy notes. This causes stress and makes it harder for him to stay on top of his care.
- Lack of Communication Between Doctors: When his cardiologist needs to know what medications, he’s been prescribed by his behavioral health provider, the information isn’t available right away. His primary care doctor doesn’t have direct access to test results from other departments. Instead, the staff often rely on phone calls, faxes, or emails — or even ask Anthony to explain or carry paperwork himself. This leads to delays, missing information, and miscommunication.
- Low Involvement in His Own Care: Because Anthony doesn’t have one clear, simple way to see all his health data, he becomes less involved in managing his health. He feels like he’s just going along with what’s being done, instead of actively participating in decisions about his care.
For the Healthcare Provider: Operational Bottlenecks and Compromised Care
Disjointed data isn’t just a patient problem — it directly impacts the ability of doctors, nurses, and healthcare staff to deliver high-quality, efficient care. It causes delays, leads to gaps in treatment, and makes the entire care process harder than it needs to be.
Poor Care Coordination and Clinical Inefficiencies
Think about a provider trying to treat a patient like Anthony, who has multiple conditions and sees different specialists. Without a complete, real-time view of his medical history:
- Key Details Are Missing: The provider might not see key details — like allergy information, previous diagnoses, or medications prescribed by other departments. This can lead to poor treatment decisions, delayed care, or medical errors.
- Referrals Are a Hassle: Sending a patient to another doctor becomes a time-consuming process, requiring multiple steps to manually collect and send the right records. Sometimes, the referred provider doesn’t receive the full information on time — disrupting continuity of care.
- Staff Workload Increases: Nurses, care coordinators, and admin teams spend hours tracking down data, copying it between systems, or trying to correct mismatched records. This takes away from time that could be used for patient care and increases burnout.
- Training Everyone Takes Time: A new system means training doctors, nurses, support staff, and administrators. This can interrupt daily operations and slow things down while everyone adjusts.
- Complex Integration Work: Merging older systems and cleaning up existing data takes time, technical skill, and careful planning. Doing it wrong can disrupt care or result in lost or inaccurate information.
Financial Strain: Hidden Costs of Fragmentation
All of these inefficiencies come with a cost. According to a McKinsey study, about 20-25% of healthcare spending in the U.S. — roughly $1 trillion — is wasted. The good news? It’s estimated that over half of that waste could be reduced with better data sharing and smarter use of information. Here’s how fragmented data leads to waste:
- Repeat Testing: Duplicate labs, imaging, and other procedures drive up costs, create more work for staff, and expose patients to unnecessary risks.
- Extra Administrative Work: When teams spend too much time on manual data entry, chasing down records, or fixing errors, it drives up operational costs without improving care.
- Problems with Billing and Payments: When billing teams don’t have accurate, timely patient data, it can result in denied claims, longer payment cycles, and a loss of revenue for the organization.
- Patient Safety Risks: Missing or incomplete health information can cause serious safety issues. For example, if a provider doesn’t know about a patient’s allergy or medication history, they may prescribe something harmful — leading to bad outcomes that could have been avoided.
- Vendors Making It Harder: Some EHR companies have built their systems in a way that blocks easy sharing of data — a practice known as “information blocking.” New rules like the 21st Century Cures Act are helping to fight this, but there’s still resistance in many places, both technically and culturally.
For the Health System: System-Wide Risks and National-Level Consequences
When EHR systems are fragmented across regions, organizations, and platforms, the consequences extend far beyond individual providers or facilities. Entire health systems—regional and national—face critical breakdowns in coordination, public health response, and long-term innovation. The lack of interoperability doesn’t just slow down care—it undermines a nation’s ability to deliver safe, equitable, and data-driven healthcare at scale.
Fragmentation of National Health Data Infrastructure
Health leaders, policymakers, and agencies can’t access a unified, real-time view of population health data.
- Public Health Surveillance Breaks Down: Without integrated data, tracking disease outbreaks or managing pandemics becomes reactive and inefficient. This slows down containment efforts and weakens emergency response.
- No Learning Health System: Fragmented data blocks efforts to develop continuous learning systems and limits cross-border research collaboration. As a result, the system can’t adapt quickly to emerging threats or leverage collective intelligence.
Barriers to Integration and Value-Based Models
Disconnected systems make it nearly impossible to scale modern, outcome-based care models across regions.
- Population Health Initiatives Stall: Payers and health networks can’t track outcomes across care settings, limiting the success of value-based programs.
- ACOs and Registries Face Technical Hurdles: Coordinated efforts like Accountable Care Organizations (ACOs), Health Information Exchanges (HIEs), and national registries hit roadblocks due to incompatible data formats and incomplete patient records.
Innovation and Research Are Stifled
Modern healthcare depends on data to drive breakthroughs. Fragmentation holds progress back.
- No National-Scale Evidence: AI, precision medicine, and drug development all require massive, clean, standardized datasets. Incomplete or incompatible data sets slow down clinical trials and limit research potential.
- Data Quality Suffers: Researchers and analysts spend more time cleaning and matching data than generating insights—limiting innovation across the board.
Unified patient data: the key to smarter, safer, and more efficient healthcare
One of the biggest takeaways from the challenges of fragmented data is clear: to deliver better, safer, and more personalized care, healthcare organizations must be able to see a complete picture of each patient.
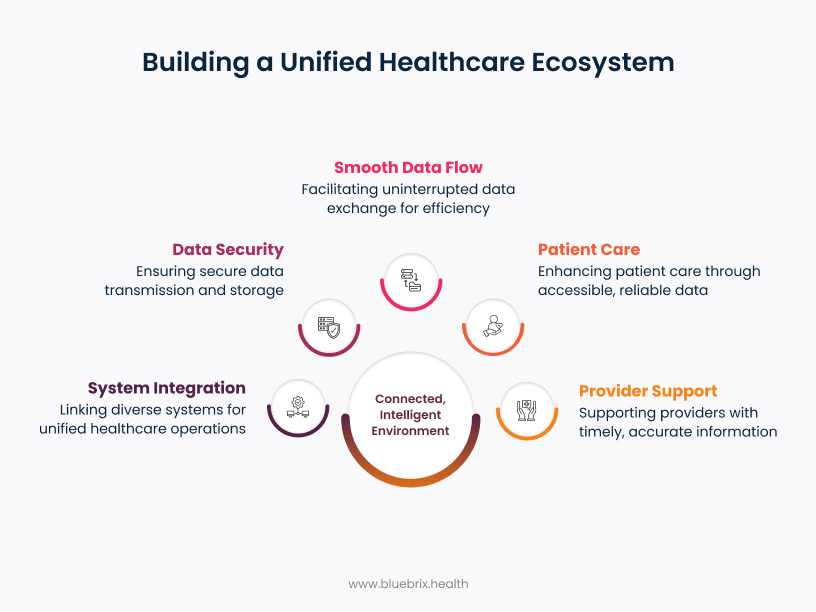
What “Unified Patient Information” Really Means
For physicians and clinical teams, unified patient information is more than just centralized data — it’s about having fast, reliable access to the right information at the right time. It means bringing together all of a patient’s records — across specialties, care settings, and systems — into a single, longitudinal digital view that’s accurate, actionable, and context-rich.
Here’s what that looks like in practice:
- Clinical Completeness: The record captures the full patient story — current medications, allergies, problem lists, diagnoses, vitals, lab results, imaging reports, immunizations, referrals, prior authorizations, and unstructured data like physician notes — whether it’s from primary care, behavioral health, acute care, or specialty services.
- Real-Time Accessibility: Data is immediately available to authorized providers across departments, care teams, and locations, regardless of where it was originally documented. This eliminates the lag of waiting on faxes or chasing information through fragmented portals.
- Data Accuracy & Reconciliation: Duplicate entries are removed, conflicting records are resolved, and outdated data is flagged. Providers can trust that what they’re seeing reflects the current clinical reality — not a patchwork of disconnected snapshots.
- Contextual Clarity: Information is presented in a clinically meaningful format — organized by relevance, not just chronology. For example, active care plans, recent medication changes, and recent labs are surfaced upfront, minimizing time spent digging through pages of PDFs or disparate systems.
- Patient Permission & Data Governance: The system supports consent-based data sharing, aligning with HIPAA and 21st Century Cures Act provisions. Patients maintain control over access rights, while providers gain confidence in the integrity and legality of shared data.
The result? Less time spent gathering background and more time focused on care. Unified data turns your EHR from a documentation tool into a real-time clinical intelligence platform — reducing guesswork, avoiding redundancy, and enabling a higher standard of care across the patient journey.
The Power of a Unified Patient Portal
For patients, the most practical and visible benefit of unified data is having one single portal to access all their health information. Right now, many patients have to deal with multiple portals, each tied to a different provider. A unified portal brings everything together in one place and comes with several key benefits:
- Patients Feel More in Control: A single portal gives patients like Anthony quick, clear access to all their health records, lab results, appointments, and care plans. This builds trust and helps them stay more involved in their health. When they can track progress, read about their conditions, and access personalized health tips, they’re more likely to follow through with care.
- Better Coordination Between Providers: With a shared view of the patient’s history, doctors across departments can quickly understand the full story. A cardiologist can see notes from a mental health visit, or a primary care doctor can check on test results ordered by a specialist. This kind of teamwork helps avoid mistakes, improves referrals, and ensures everyone is on the same page.
- More Efficient Operations: When systems are connected and data is clean, staff spend less time on paperwork and chasing down records. This means they can focus more on patients, not administrative tasks.
- A Strong Base for Using AI and Analytics: When all data is in one place and well-organized, healthcare systems can use it to spot trends, predict problems, and plan better treatments. For example, they can identify which patients are at higher risk, or which treatments are working best for certain groups. This kind of insight supports smarter, value-based care.
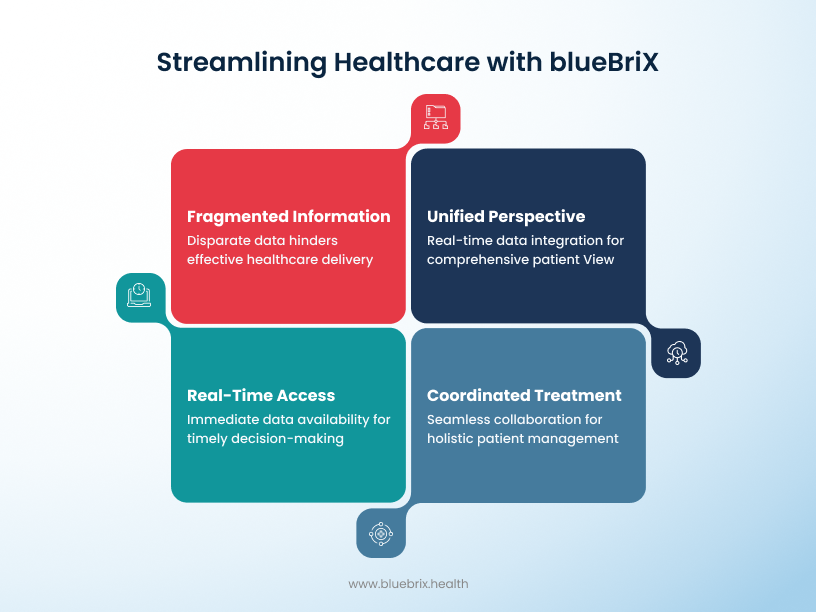
Why blueBriX is a strategic choice for healthcare organizations
Now that we’ve outlined the need for a unified patient platform, let’s look at how blueBriX delivers on that promise. Designed to fix the challenges of disconnected EHR systems, blueBriX goes beyond basic system connection.
Built with an API-First Mindset
At the core of blueBriX’s success is its API-first architecture. If you’re not familiar, an API (Application Programming Interface) is what lets different software systems talk to each other. In healthcare, that means your EHR, imaging system, billing system, and even mobile apps can all exchange information securely and efficiently.
Building blueBriX around APIs from the start allows for better flexibility, speed, and scale. Here’s how that plays out in the real world:
- Smooth Data Sharing Between Systems: Unlike older systems that use rigid, one-off connections, blueBriX makes it easy for different platforms to work together. Whether it’s Epic, Cerner, Athena, or other tools, blueBriX acts like a translator — making sure they all understand each other and share data properly.
- Built on Healthcare Standards: blueBriX is fully aligned with modern standards like FHIR (Fast Healthcare Interoperability Resources), developed by HL7. That’s important because FHIR is the new standard most U.S. systems are moving toward. It organizes health data into clear, consistent formats so systems can easily pull, push, and interpret information — without needing complex custom coding.
- Modular and Flexible by Design: Because blueBriX is built with reusable pieces (or “modules”), it can grow and adapt without needing to overhaul everything. Whether you’re adding a new specialty, rolling out a wearable device integration, or linking a third-party app like Redox, it’s quick to plug in. This modular approach saves time and keeps integration costs low.
Exceptional Integration Capabilities
One of blueBriX’s biggest strengths is how well it integrates with different systems. blueBriX is designed to make data sharing between different systems simple and fast. Built with an API-first approach, it connects easily with popular EHRs like Epic, Cerner, and Athena Health—so you don’t have to worry about delays or messy integrations. It also supports tools like Redox to standardize data from different sources, and can even connect to your custom or in-house systems using flexible APIs.
Whether you’re pulling lab results, medical history, or device data, blueBriX keeps everything up to date in real time. That means clinicians get the full picture without delays—making it easier to act fast, stay informed, and deliver better care.
Scalable and Cloud-Native by Design
For larger healthcare organizations, scalability isn’t optional—it’s critical. blueBriX was designed from the ground up to handle growing volumes of data, users, and demands for digital services.
- Flexible Performance During High Demand: Whether it’s flu season or a public health emergency, blueBriX automatically adjusts to handle more traffic and data without slowing down. When demand is lower, it can scale back to reduce unnecessary costs.
- Lower Infrastructure and IT Costs: Because blueBriX is cloud-native, there’s no need for bulky hardware or constant maintenance from on-site IT teams.
- Accessible and Disaster-Ready: Since blueBriX is cloud-based, it can be accessed from anywhere with internet—ideal for remote work, distributed care teams, and telehealth models. It also has built-in backup and recovery features to ensure uptime and protect against disruptions.
Faster Rollout with Pre-Built Templates
A common challenge in healthcare IT is how long it takes to roll out new technology. blueBriX helps organizations get started quickly and efficiently by offering ready-to-use components.
- Pre-Configured for Healthcare Workflows: blueBriX comes with built-in templates for everyday workflows like patient intake, test results delivery, appointment scheduling, and more. These templates help organizations get started faster without having to build everything from scratch.
- Shorter Implementation Time and Lower Costs: Because much of the setup work is already done, healthcare organizations can launch faster—cutting down on both development time and cost. At the same time, blueBriX allows for customizations when needed, offering both speed and flexibility.
- Compatible from Day One: Using these pre-built elements also helps ensure your system is compatible with other tools right from the start. It gives your team more time to tailor the platform to your specific needs instead of wasting effort building basic functions.
Strong Data Security and Compliance
In healthcare, protecting patient data is non-negotiable. blueBriX takes data security seriously and builds it into every part of the platform.
- Multiple Layers of Protection: Data is encrypted both when it’s stored and when it’s being shared across systems. This means sensitive health information stays secure at all times.
- Strict Access Controls: Not everyone needs to see everything. With blueBriX’s role-based access system, each user only sees the data they need for their role—nothing more. This minimizes internal risks and protects patient privacy.
- Meets U.S. and Global Standards: blueBriX is built to meet HIPAA requirements in the U.S. and GDPR standards in Europe. It also includes features like audit trails and system monitoring to help organizations stay compliant with ever-evolving regulations.
- Ongoing Security Monitoring: The platform is regularly tested for vulnerabilities. Security patches and system updates are applied as needed to stay ahead of potential threats and ensure system integrity.
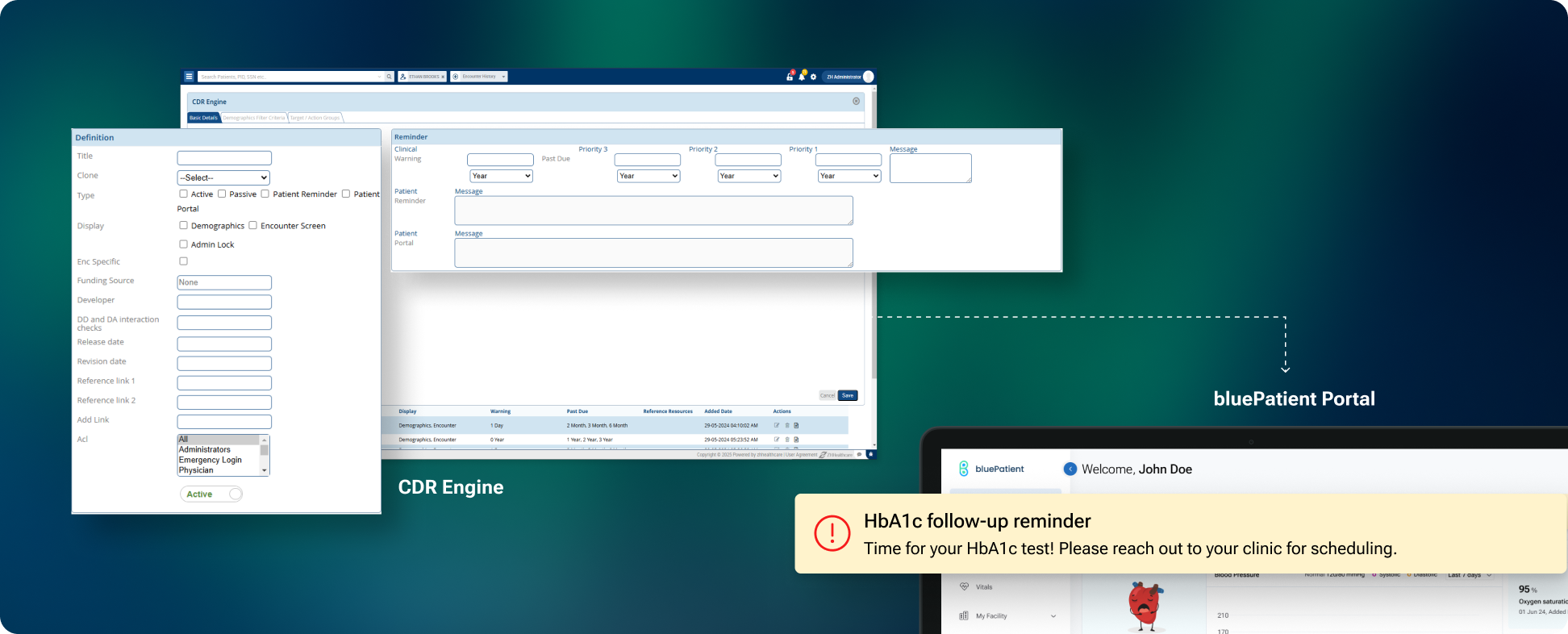
How blueBriX Brings All Patient Data Together
The real value of blueBriX is how it pulls everything into a single, secure, up-to-date patient record — no matter where the data comes from.
Safe and Accurate Patient Matching
One of the biggest risks in healthcare is misidentifying patients. Duplicate records and mismatches can lead to dangerous errors. blueBriX has built-in tools to prevent this:
- Advanced Matching Algorithms: When someone checks in, blueBriX confirms their identity by matching multiple fields — like name, DOB, gender, and even Social Security number (where used).
- Flags Conflicts for Review: If there’s ever a discrepancy — like two patients with similar names — the system immediately alerts staff to review and resolve the issue. That human oversight ensures data stays clean and reliable.
- Built-In Privacy and Security: Data is encrypted in transit and at rest, and all access is tightly controlled. Patients must authorize any sharing of their data, and the system complies fully with HIPAA and GDPR guidelines.
Here’s how blueBriX does it step-by-step:
- Pulls Data from Multiple Sources: This includes your EHRs, lab systems, imaging, billing platforms, wearable tech, and even patient apps. The data comes in many formats — and blueBriX is built to handle them all.
- Cleans and Standardizes the Data: Different systems use different terms and structures. blueBriX transforms all that messy input into clean, consistent formats. For example, it might convert an HL7 message into a FHIR resource to make it usable in other systems. That standardization is key for accurate care.
- Centralizes the Information: Once standardized, the data is brought into a central, secure repository. That means no matter which part of your organization a patient visits — primary care, specialty, hospital — their complete history is automatically available to any clinician with the right permissions.
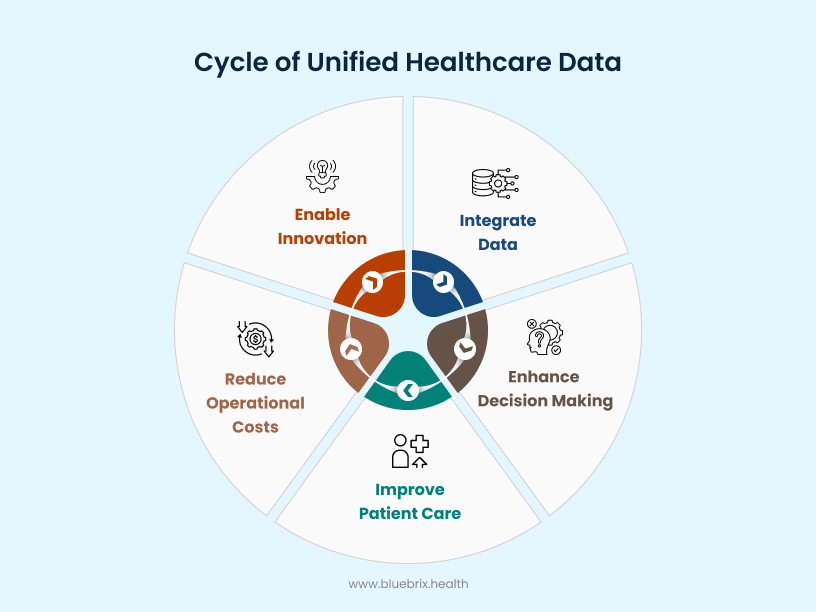
The broader impact of unified patient data
The deployment of a unified patient information platform powered by blueBriX creates a virtuous cycle of benefits that extend far beyond simply alleviating immediate pain points. It fosters a fundamental transformation, enhancing the experience for patients, empowering healthcare providers, and ultimately contributing to a more efficient, effective, and sustainable healthcare system.
- One Longitudinal Record: Instead of piecing together records from multiple systems or waiting on faxes from other providers, clinicians can see a full picture—labs, imaging, notes, diagnoses—all in one place. This helps reduce guesswork, avoid repeated tests, and support more confident, accurate decisions.
- Less Admin Work, More Time for Care: Doctors and clinical staff no longer need to log into multiple systems, dig through scattered notes, or spend hours on documentation. With clean, organized data in one system, providers can spend more time with patients and less time switching through screens.
- Team-Based Care Made Easier: When every provider involved in a patient’s care has access to the same information, coordination improves. Primary care doctors, specialists, therapists, and case managers can all stay on the same page. This leads to fewer errors, clearer care plans, and smoother transitions between visits.
- Better Patient Engagement and Outcomes: By consolidating lab results, appointments, and prescriptions into one centralized platform, patients gain a clear, real-time view of their entire care journey. This not only reduces confusion and delays but also drives stronger engagement, encourages self-management, and leads to better outcomes. When patients can easily track their progress, understand their next steps, and communicate proactively, they’re more likely to follow through—preventing complications and unnecessary ER visits.
- Using Data to Guide Care: With all the data in one place, it’s easier to identify high-risk patients and act early. For example, if Anthony’s behavioral health notes show increased anxiety while his cardiac readings trend poorly, his care team can step in before it becomes a crisis.
Building a future-ready healthcare system
The future of healthcare will be built on the ability to connect systems, share data, and generate actionable insights. Whether it’s real-time interoperability through standards like FHIR, the shift to value-based and personalized care, or the growing role of AI—none of it can succeed without a unified, trustworthy data platform.
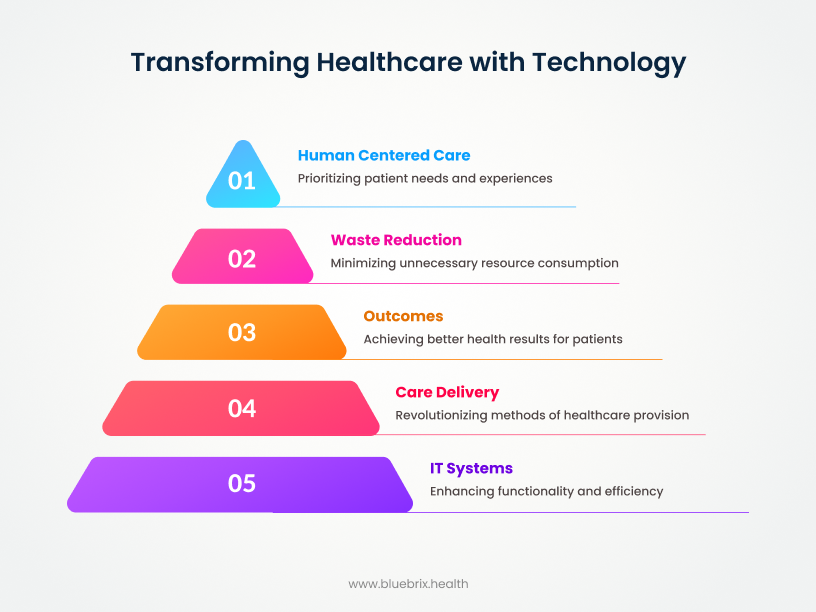
Moving toward value-based and personalized care
Another big change shaping healthcare is the shift from fee-for-service (FFS) to value-based care (VBC).
Data is essential for value-based care: VBC only works if healthcare providers can track outcomes, manage risk, and coordinate care across different settings. That requires access to a complete, real-time view of each patient’s history. Without unified data, providers are flying blind—unable to measure success, identify gaps, or deliver efficient care.
Making care more proactive: With connected, up-to-date patient data, organizations can use predictive tools to spot patients at risk of developing chronic conditions or needing emergency care. This enables earlier interventions, preventive strategies, and outreach that improve outcomes and lower overall costs.
Enabling personalized medicine: Unified data also makes it possible to move beyond “one-size-fits-all” treatments. By combining clinical data with genomics, lifestyle information, and data from patient devices, healthcare providers can tailor care plans to each person’s unique profile. Personalized care improves effectiveness and helps avoid adverse reactions or unnecessary interventions.
Unlocking the power of AI and advanced analytics
A truly unified data platform also makes it possible to take full advantage of artificial intelligence (AI) and advanced analytics in healthcare. Without clean, connected data, AI is just a theory. But with the right data infrastructure, AI can deliver real value.
Smarter diagnoses with AI: AI tools can analyze large amounts of medical images, lab values, and clinical notes to identify subtle warning signs that humans might miss. This can lead to earlier and more accurate diagnosis for diseases like cancer, heart conditions, or diabetic eye disease.
Predictive insights and risk identification: AI-powered analytics can identify patients who are likely to be readmitted, who might develop complications, or who are at risk of falling through the cracks. These insights allow healthcare providers to act early, reduce preventable events, and manage costs more effectively.
Improving operations, not just clinical outcomes: AI can also help behind the scenes—automating scheduling, forecasting demand for staffing or beds, and speeding up billing and administrative processes.
Making use of unstructured data: Healthcare generates a lot of unstructured data—like doctor’s notes, audio dictations, and patient feedback. With tools like Natural Language Processing (NLP), AI can turn that messy text into usable insights, giving providers a more complete picture of the patient.