Hospital readmissions, defined as a patient’s return to the hospital within a short period after discharge, pose significant challenges to healthcare systems worldwide. They not only strain hospital resources but also expose patients to increased risks of complications and higher healthcare costs. In the United States, for instance, nearly 20% of Medicare beneficiaries are readmitted within 30 days of discharge, leading to an estimated $17 billion in avoidable costs annually.
Between 2016 and 2020, the 30-day all-cause hospital readmission rate in the United States remained stable at 13.9 per 100 index admissions. Notably, in 2020, patients with Medicare had the highest readmission rate at 17.0 per 100 index admissions, followed by those with Medicaid at 13.6 per 100 index admissions.
Readmission rates can vary significantly by state, ranging from 11.2% to 22.3% across the U.S. Additionally, certain medical conditions exhibit higher readmission rates; for instance, diabetes has a readmission rate of approximately 8.76%, while pneumonia stands at about 1.83%.
Financial burden of readmissions on healthcare systems
Hospital readmissions impose a substantial financial burden on healthcare systems. In 2013 alone, Medicare hospital readmissions cost $29.6 billion. The average cost per readmission is estimated at $15,200. To address this issue, programs like the Hospital Readmissions Reduction Program (HRRP) have been implemented. Since 2012, nearly $2 billion in financial penalties have been imposed on hospitals by the HRRP to incentivize the reduction of readmission rates.
Emotional and physical impact on patients
Frequent hospital readmissions can have profound emotional and physical effects on patients. Emotionally, patients may experience increased feelings of depression and anxiety due to the stress of repeated hospital stays. Physically, the disruption of daily routines and the hospital environment can hinder recovery and diminish overall well-being. Moreover, hospital readmissions often result in out-of-pocket expenses for patients, including co-payments and deductibles, adding a financial strain that can exacerbate emotional distress.
In effect, hospital readmissions present significant challenges, affecting healthcare systems financially and impacting patients’ emotional and physical health. Efforts to reduce readmission rates are crucial for improving patient outcomes and alleviating the financial strain on healthcare systems.
Several factors contribute to the high rates of hospital readmissions:
- Inadequate discharge planning: Patients often leave the hospital without a clear understanding of their care instructions, leading to mismanagement of their conditions at home.
- Medication errors: Miscommunication about medication regimens can result in patients taking incorrect dosages or missing essential medications, exacerbating their conditions.
- Lack of follow-up care: Without timely follow-up appointments, emerging health issues may go unnoticed until they become severe enough to require readmission.
- Socioeconomic factors: Patients from disadvantaged backgrounds may face challenges such as limited access to transportation, inadequate social support, or financial constraints, all of which can hinder effective post-discharge care.
While all of them should be addressed in detail, in this article, we discuss how hospital readmissions due to lack of follow up care can be effectively addressed with remote patient monitoring or RPM. As more healthcare ecosystems are moving to value-based care, keeping readmission rates low becomes one of the daunting tasks and RMP is a proven method that works.
What is remote patient monitoring?
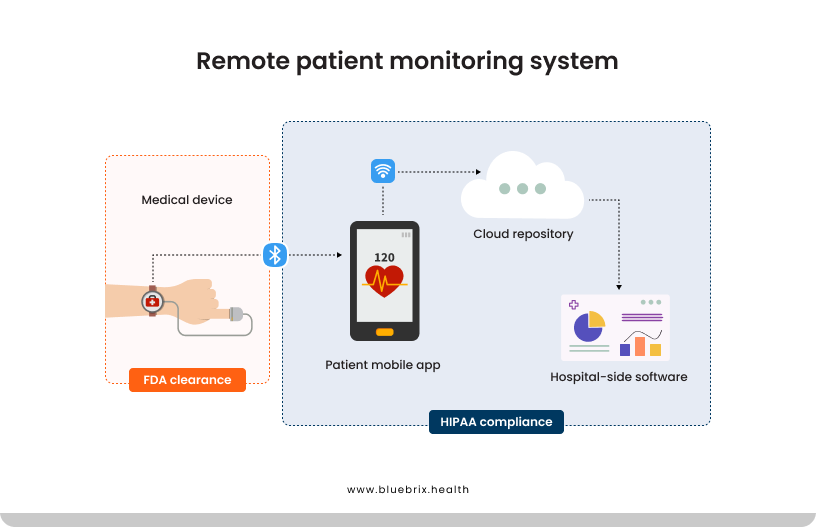
Remote patient monitoring(RPM) is a healthcare approach that utilizes digital technologies to collect health data from patients in one location and electronically transmit it to healthcare providers in a different location for assessment and recommendations. This method enables continuous monitoring of patients outside traditional clinical settings, enhancing the management of chronic diseases and post-operative care.
Key technologies used in RPM
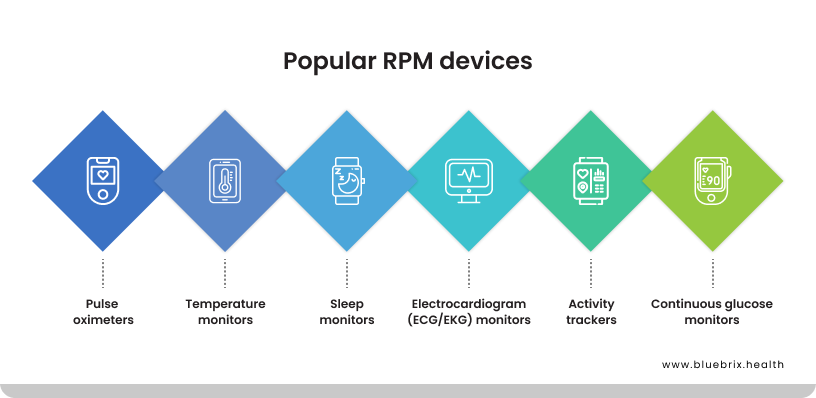
RPM employs a variety of digital devices and communication technologies to monitor and transmit patient data. Some of the most commonly used devices include:
- Blood pressure monitors: These devices measure a patient’s blood pressure and transmit the readings to healthcare providers, aiding in the management of hypertension and related conditions.
- Glucometers: Used by diabetic patients, glucometers measure blood glucose levels, allowing for real-time monitoring and management of diabetes.
- Pulse oximeters: These devices monitor oxygen saturation levels in the blood, which is crucial for patients with respiratory conditions.
- Wearable devices: Activity trackers and smartwatches can monitor various health metrics such as heart rate, physical activity, and sleep patterns, providing a comprehensive view of a patient’s health status.
- Health patches: Health patches are wearable devices designed for continuous monitoring of various physiological parameters. These soft, adhesive patches are applied directly to the skin, allowing for unobtrusive data collection. They can monitor metrics such as heart rate, blood pressure, glucose levels, and stress indicators. For instance, some wearables enable continuous monitoring through a sticker or patch applied onto the patient’s body, facilitating ongoing symptom and biometric tracking.
- Smart implants: Smart implants represent a significant advancement in RPM by integrating sensors directly into medical implants. These devices can monitor various health metrics and transmit data to healthcare providers for analysis. A notable example is the development of smart knee implants that allow for remote monitoring of a patient’s recovery after total knee replacement surgery. These implants can measure steps taken, walking speed, range of motion, and other indicators of knee function, providing valuable insights into the patient’s rehabilitation progress.
These devices typically use Bluetooth, Wi-Fi, or cellular technologies to transmit data in real-time to healthcare providers, ensuring timely interventions when necessary.
Did you know that RPM can lead to a reduction in hospital readmissions by up to 25%?
How RPM reduces hospital readmissions
Remote patient monitoring enables continuous observation of patients’ health outside traditional clinical settings. This proactive approach is instrumental in reducing hospital readmissions through early detection of health deterioration, timely interventions, personalized care plans, and continuous data collection.
Early detection of health deterioration
RPM employs devices like wearable gadgets, smart implants, and home monitoring tools to track vital signs such as heart rate, blood pressure, and glucose levels in real-time. This continuous monitoring allows healthcare providers to identify subtle changes in a patient’s condition promptly. For instance, smart implants are increasingly used to treat various diseases, track patient status, and restore tissue and organ function. These devices support internal organs, actively stimulate nerves, and monitor essential functions, thereby improving patient observation quality and subsequent treatment.
Timely interventions and personalized care plans
The real-time data from RPM devices enable healthcare providers to intervene swiftly when a patient’s condition worsens. For example, smart knee technology allows care teams to remotely monitor a patient’s recovery after total knee replacement surgery, ensuring timely interventions if complications arise. This immediate response capability reduces the likelihood of hospital readmissions.
Moreover, RPM facilitates the development of personalized care plans tailored to individual patient needs. By analyzing data trends, healthcare providers can adjust treatments and recommend lifestyle changes that enhance patient outcomes. This personalized approach ensures that care plans are responsive to the unique health patterns of each patient, thereby reducing the risk of readmission.
Continuous monitoring and data collection
Continuous data collection is a cornerstone of RPM, providing a comprehensive view of a patient’s health over time. Devices such as wearable gadgets, smart implants, hospital equipment, and medical devices, powered by the Internet of Things (IoT), improve patient care and clinical outcomes by enabling real-time health monitoring. This wealth of data allows for more accurate assessments and informed decision-making, contributing to better management of chronic conditions and early detection of potential health issues.
Several studies have highlighted the effectiveness of RPM in reducing hospital readmissions. For instance, remote patient monitoring led to a 50% reduction in 30-day hospital readmissions for patients with heart conditions, according to a study published in Medical Economics. Additionally, the integration of smart implants in healthcare is reshaping service delivery by enhancing health monitoring for early disease detection, tracking physiological conditions, and preventing complications.
In short, RPM’s ability to provide continuous, real-time health monitoring enables early detection of health deterioration, facilitates timely interventions, supports personalized care plans, and offers compelling evidence of its effectiveness in reducing hospital readmissions.
How to implement RPM effectively to reduce hospital readmissions?
Implementing Remote Patient Monitoring in healthcare organizations is a strategic move that can significantly reduce hospital readmissions, particularly in the context of value-based care. As healthcare systems shift their focus from volume to value, RPM emerges as a vital tool for enhancing patient outcomes while controlling costs. Here’s a detailed look at effective strategies for implementing RPM, supported by relevant statistics and examples.
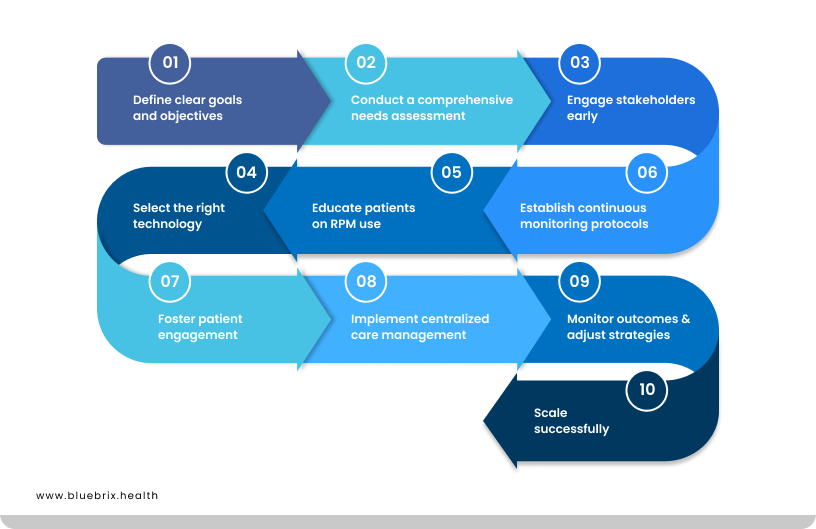
Define clear goals and objectives
Before diving into the implementation of RPM, it’s essential to establish clear goals. Are you aiming to reduce hospital readmissions, improve chronic disease management, or enhance medication adherence? Having specific, measurable objectives will guide your program and provide benchmarks for success. For instance, a healthcare organization might set a goal to decrease 30-day readmission rates by 20% within the first year of implementing RPM.
Conduct a comprehensive needs assessment
Understanding your patient population is crucial. Identify which groups would benefit most from RPM—typically those with chronic conditions like diabetes or heart disease that require ongoing monitoring. For example, a study found that implementing RPM for patients with heart failure led to a 76% reduction in readmissions within 30 days post-discharge. This data-driven approach ensures that resources are allocated effectively.
Engage stakeholders early
Creating a multidisciplinary team that includes physicians, nurses, IT staff, and even patients is vital for successful RPM implementation. This team can identify pain points, streamline workflows, and ensure that the technology meets clinical needs. Regular meetings and open communication foster collaboration and buy-in from all parties involved.
Select the right technology
Choosing the appropriate RPM technology is critical. Evaluate vendors based on their ability to meet your specific goals and integrate seamlessly with existing electronic health record (EHR) systems. Look for solutions that offer user-friendly interfaces and robust data analytics capabilities to track patient progress effectively.
Educate patients on RPM use
Patient education is key to ensuring the success of an RPM program. Provide comprehensive training on how to use monitoring devices and platforms effectively. For instance, a Midwest health system implemented automated communication tools that engaged patients through text messages and phone calls, ensuring they understood how to use their devices and the importance of regular monitoring.
Establish continuous monitoring protocols
Set up protocols for continuous data collection and monitoring. This includes regular check-ins and data uploads to track vital signs and other health metrics effectively. Utilizing data analytics can help identify trends early on, allowing healthcare providers to intervene before conditions worsen.
Foster patient engagement
Engaging patients in their care journey enhances adherence to treatment plans. Involve them in decision-making regarding their monitoring plans and adjust data collection frequency based on individual needs. Research indicates that when patients feel involved in their care, they are more likely to comply with monitoring protocols.
Implement centralized care management
Building centralized care management pods can help address the unique needs of different patient populations. These pods should include nurses, physicians, and care coordinators who work together to engage with patients proactively. This team-based approach ensures that care is tailored to individual needs while optimizing resource utilization.
Monitor outcomes and adjust strategies
Once your RPM program is up and running, continuously evaluate its effectiveness against the established goals. Collect feedback from both patients and healthcare providers to identify areas for improvement. For example, if readmission rates are not decreasing as expected, reassess patient engagement strategies or technology usability.
Scale successfully
As your RPM program matures, consider how it can be expanded or enhanced. Look for opportunities to incorporate additional technologies or services that could further improve patient outcomes or streamline operations.
Implementing Remote Patient Monitoring is not just about adopting new technology; it’s about transforming how healthcare organizations engage with patients in a value-based care model. By following these strategies—defining clear goals, engaging stakeholders, educating patients, and continuously monitoring outcomes—healthcare providers can significantly reduce hospital readmissions while improving overall patient care quality.
Challenges in implementing RPM
Implementing RPM has the potential to revolutionize healthcare by enabling continuous patient observation outside traditional clinical settings. However, several challenges can impede its effective adoption. Let’s explore these obstacles, supported by relevant statistics and examples.
Data management and workflow integration
Healthcare providers often face difficulties handling the influx of data generated by RPM devices. Establishing a manageable workflow to process and respond to this data is crucial. A study highlighted that primary care physicians identified barriers such as difficulties in managing data and integrating it into existing workflows.
Patient engagement and compliance
The success of RPM heavily relies on patient participation. Challenges arise when patients forget to use devices, fail to charge them, or lack the necessary skills to operate them properly. This non-compliance can lead to data gaps, compromising the effectiveness of RPM programs.
Technological barriers
Patients may encounter difficulties with the technology used in RPM, especially if they are not tech-savvy. Issues such as disorienting technology and digital literacy barriers can hinder effective use. A study noted that challenges included digital and health literacy barriers among patients.
Data accuracy and reliability
Ensuring the accuracy of data collected through RPM devices is vital. Inaccurate data can lead to misdiagnoses or inappropriate treatment plans. Factors contributing to data inaccuracy include device malfunctions and improper usage by patients.
Financial considerations
The cost of implementing RPM can be a significant barrier for healthcare organizations. Expenses related to purchasing devices, training staff, and maintaining the technology can add up. A study found that many primary care physicians did not believe RPM was profitable, highlighting financial concerns as a barrier to adoption.
Privacy and security concerns
Protecting patient data from cybersecurity threats is paramount. RPM systems are vulnerable to hacking, data breaches, and malware attacks. Ensuring robust security measures are in place is essential to maintain patient trust.
Increased workload for healthcare providers
The continuous stream of data from RPM devices can lead to an increased workload for healthcare providers. Managing and responding to this data requires additional time and resources, which can be challenging for already overburdened healthcare systems.
Patient anxiety and over-reliance
Some patients may experience increased anxiety due to constant monitoring, feeling overwhelmed by the continuous observation of their health metrics. Additionally, there is a risk of patients becoming overly reliant on RPM, potentially neglecting traditional in-person consultations.
Addressing the digital divide
The digital divide, particularly in rural or underserved areas, can limit the effectiveness of RPM. Limited internet connectivity and lack of access to modern technology can hinder the deployment and utilization of RPM systems. Innovative solutions, such as utilizing opportunistic networks, are being explored to overcome these challenges.
While RPM offers significant benefits in enhancing patient care, addressing these challenges is crucial for its successful implementation. Healthcare providers must develop strategies to manage data effectively, engage patients, ensure data accuracy, address financial concerns, and protect patient privacy to fully realize the potential of RPM.
How can digital health improve the outcomes of RPM?
Digital health play a pivotal role in enhancing the outcomes of Remote Patient Monitoring, fundamentally transforming how healthcare is delivered. By leveraging advanced tools and systems, healthcare providers can improve patient engagement, streamline data collection, and ultimately reduce hospital readmissions. Here’s a closer look at how these technologies make a difference.
Integrating Remote Patient Monitoring with digital health tools is becoming increasingly essential in modern healthcare. As we navigate a landscape marked by an aging population, rising chronic diseases, and workforce shortages, the need for effective solutions that enhance patient care and reduce hospital readmissions has never been more pressing. Let’s explore why this integration is crucial and how it can transform healthcare delivery.
The need for integration
- Rising healthcare demands: The global healthcare system is under immense pressure due to an aging population and a surge in chronic diseases. For instance, the World Health Organization estimates that by 2030, the number of people aged 60 years and older will reach 1.4 billion, leading to increased demands for healthcare services. RPM can help manage these demands by enabling continuous monitoring of patients from the comfort of their homes.
- Hospital readmissions: Hospital readmissions are a significant concern, costing the U.S. healthcare system approximately $17 billion annually. RPM can play a pivotal role in reducing these costs by allowing healthcare providers to monitor patients remotely and intervene before conditions worsen.
- Workforce shortages: With healthcare professionals facing burnout and shortages, integrating RPM with digital health tools can alleviate some of the burdens on providers. By automating data collection and facilitating remote consultations, RPM helps ensure that healthcare teams can focus on delivering quality care rather than being overwhelmed by administrative tasks.
Enhanced data collection and analysis
One of the most significant advantages of digital technologies in RPM is the ability to collect vast amounts of health data in real-time. Wearable devices, such as smartwatches and continuous glucose monitors, allow patients to track vital signs like heart rate, blood pressure, and glucose levels from the comfort of their homes. This continuous data flow enables healthcare providers to monitor patient health proactively.
For instance, a study highlighted that RPM technologies can lead to a 9.6% reduction in hospitalizations due to better monitoring and timely interventions. By analyzing this data using machine learning algorithms, healthcare professionals can identify trends that may indicate deteriorating health conditions, allowing for quicker diagnoses and treatment adjustments.
Improved patient engagement
Digital technologies foster greater patient engagement in their healthcare journey. Through user-friendly applications and platforms, patients can easily access their health data, receive reminders for medication adherence, and communicate with their healthcare providers. This level of engagement is crucial; research shows that increased patient involvement is linked to better compliance with treatment plans.
For example, RPM systems often include features that allow patients to log symptoms or report changes in their condition directly to their care team. This immediate communication helps ensure that any potential issues are addressed promptly, reducing the likelihood of readmissions.
Real-time alerts and notifications
Digital alerting systems integrated into RPM platforms provide real-time notifications for both patients and healthcare providers. When a patient’s monitored data indicates a potential health risk—such as an abnormal heart rate or significant weight gain—alerts can be triggered automatically. This immediate feedback allows for swift action, whether it’s adjusting medication or scheduling an urgent appointment.
A systematic review found that digital alerting systems could significantly reduce hospital length of stay by an average of 1.043 days, showcasing the effectiveness of timely interventions made possible through technology.
Telehealth integration
The integration of RPM with telehealth services creates a comprehensive care model that enhances patient outcomes. Patients can have virtual consultations with their healthcare providers while simultaneously sharing real-time health data collected through RPM devices. This synergy allows for more informed decision-making during appointments.
Studies indicate that combining telehealth with RPM leads to significant improvements in managing chronic conditions like heart failure and COPD. For instance, 17 systematic reviews concluded that remote monitoring improves mortality rates and quality of life while reducing hospitalizations.
Personalized care plans
Digital technologies enable the creation of personalized care plans based on real-time data analysis. By understanding each patient’s unique health patterns and needs, healthcare providers can tailor interventions more effectively.
For instance, continuous glucose monitoring devices provide insights into how a patient’s blood sugar levels fluctuate throughout the day. This information allows healthcare teams to adjust insulin dosages or dietary recommendations in real time, leading to better diabetes management and fewer complications that could result in hospitalization.
Cost-effectiveness
Implementing RPM through digital technologies not only improves clinical outcomes but also offers significant cost savings for healthcare systems. A study at Dartmouth-Hitchcock Medical Center demonstrated that using an RPM system resulted in a 65% reduction in distress codes and rescue activations, along with a 48% decrease in patient transfers to intensive care units, yielding substantial cost savings. By reducing hospital readmissions—often one of the most expensive components of patient care—RPM can help organizations allocate resources more efficiently.

