“Another Monday. Another pile of denials.” Sound familiar?
If you’re part of the billing or Revenue Cycle Management team, this story probably hits close to home: tight deadlines, payer rejections, long hours — and still, the numbers don’t quite add up.
Mid-sized practices are quietly losing 10–15% of their revenue every year. But it’s not because your team isn’t working hard — it’s because the system is riddled with inefficiencies, under-coding, aging A/R, and never-ending follow-ups.

A simple checklist to assess your current revenue leakage:
Not sure if your practice is bleeding revenue? Here’s a quick frontline reality check:
- Are your denials creeping past 10% — no matter how much you rework?
- Is your A/R log filled with claims aged over 45 days?
- Does denial management feel like a reaction game instead of a real process?
- Is your billing team overwhelmed, short-staffed, or burning out?
- Do you have to dig across systems just to see performance KPIs?
- Are you second-guessing whether your coding reflects the care actually delivered?
- Is follow-up happening late — or not at all — because you’re just trying to stay afloat?
If you’re nodding ‘yes’ to a few of these, you already know you’ve got leakage. Let’s not just patch the holes — let’s prevent them before they form.
The costly consequences of revenue cycle inefficiencies
Several factors contribute to this substantial revenue leakage. Understanding these is the first step towards recovery:
- Denials: Denials feel like déjà vu. You fix them today, and they’re back tomorrow. Whether it’s missing documentation or incorrect codes, denials don’t just slow down cash flow — they wear your team down. A denial rate exceeding 10%, a common challenge for many practices, translates directly into unpaid services and increased administrative burden for rework. Incorrect coding, missing documentation, lack of pre-authorization – the reasons are varied, but the outcome is the same: delayed or lost payments.
- Under-coding: If your coders are flying blind with outdated tools or thin documentation, chances are, you’re leaving money on the table every day. Under-coding, often due to a lack of detailed documentation or outdated coding tools, means you’re not billing for the full scope of services provided. Over time, these seemingly small instances of under-coding can accumulate into significant revenue loss.
- Delayed A/R: If 30%+ of your claims are aging past 45 days, collections drop fast. Old claims need aggressive follow-up — not “someday” status. The longer your Accounts Receivable (A/R) remains outstanding, the lower the probability of collection. Poor follow-up on outstanding claims, inefficient billing processes, and unresolved payer issues contribute to this leakage.
The result? More stress. More backlog. Less revenue. But there’s a smarter way forward.
A real-world wake-up call: $500k+ lost in one quarter
One practice we worked with had over $500,000 stuck in claims older than 90 days — in just one quarter. Their team? Dedicated but drowning. Between chasing denials and trying to appeal on time, their small billing staff was stretched thin. The burnout was real.
We helped them prioritize follow-up, automate denial tracking, and turn A/R into real revenue again — without expecting their team to work miracles.
Targeted RCM improvements: your strategy to stop the bleeding
Let’s make your job smoother — not harder. The good news is that this revenue leakage isn’t inevitable. Targeted improvements in your RCM processes can significantly recover lost cash flow and optimize your financial health.
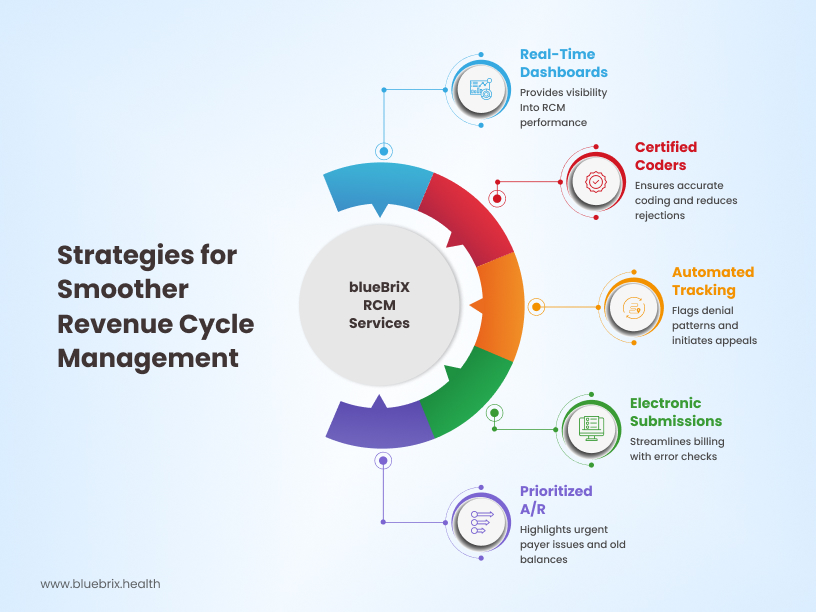
Code right, the first time
Investing in certified coders, implementing regular coding audits, and utilizing up-to-date coding software are crucial steps. Accurate coding from the outset minimizes denials and ensures you’re billing for the complete services rendered.
Track denials automatically
Implement a system to track denial codes meticulously, identify recurring issues, and establish a proactive process for appealing denied claims within payer timelines.
Submit clean claims fast
Streamline your charge entry and claims submission processes. Electronic claims submission, coupled with robust error checking, reduces delays and ensures clean claims are submitted promptly.
Prioritize smart A/R
Implement a systematic approach to A/R follow-up, prioritizing older balances and proactively addressing payer issues. This includes regular review of aging reports and timely communication with payers.
Visibility that makes sense
Gain real-time visibility into your key RCM metrics. Get actionable insights from comprehensive reports that allow you to identify bottlenecks, track performance, and make data-driven decisions to improve revenue integrity.
The outsourcing advantage: is it right for you?
We get it. Sometimes your internal team is doing everything humanly possible — and still falling behind. For many mid-sized practices with lean internal billing teams, outsourcing RCM can be a strategic move to plug revenue leaks and improve efficiency. Here’s how outsourcing RCM to blueBriX gives your team the backup they deserve:
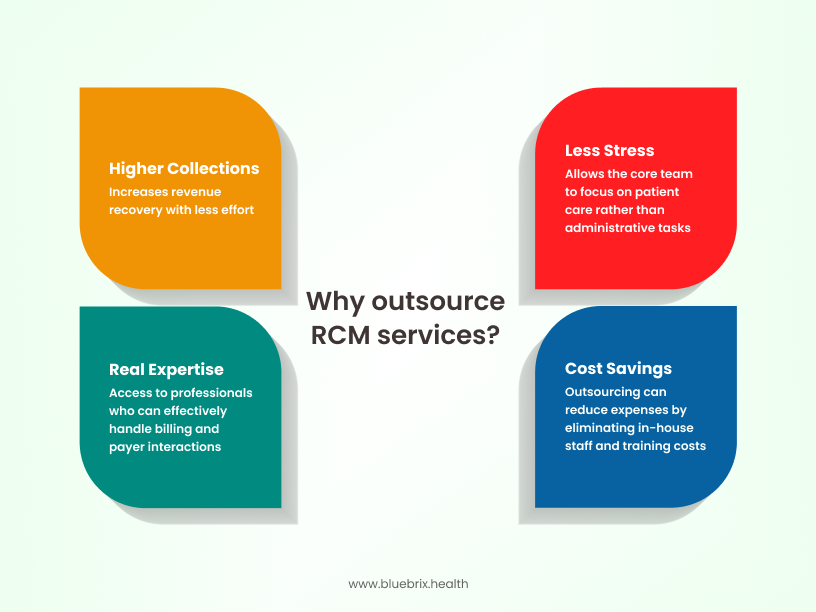
- Cost savings: While there’s an upfront cost to outsourcing, it can often be more cost-effective than hiring and training additional billing staff, investing in technology, and managing employee turnover.
- Expertise and experience: blueBriX brings 2 decades of specialized knowledge, experienced professionals, and proven processes to optimize your revenue cycle.
- Focus on core competencies: Outsourcing allows your internal team to focus on patient care, the core of your practice.
- Improved collection rates: RCM experts are often more effective at navigating complex payer rules and maximizing collections, directly impacting your bottom line.

