The US healthcare ecosystem has been shifting focus from the traditional fee-for-service model to value-based care models which fundamentally aims to ensure better care and outcomes at lower costs. Though value based care is a payment mechanism, shifting the focus from quantity to quality emphasizes the need for quality care. Care Models in VBC are evolving along with technology, changing human perceptions of care, and environmental changes. One of the key advancements with the adoption of VBC is that population health management (PHM) and social determinants of health are being given due importance. Using big data, technologies like data analytics, and predictive analytics are keeping many potentially fatal health issues well under control, changing the trajectory of healthcare across the globe. Covid-19 protocols and how the world tackled it efficiently is proof enough to understand the importance of PHM.
Care models are the blueprints for how healthcare is delivered under VBC. They incentivize providers to deliver high-quality, efficient care that improves patient outcomes. This article explores the evolution of care models in the US, various care models being implemented within the VBC framework, examining their functionalities, potential benefits, challenges, and future.
Evolution of healthcare delivery
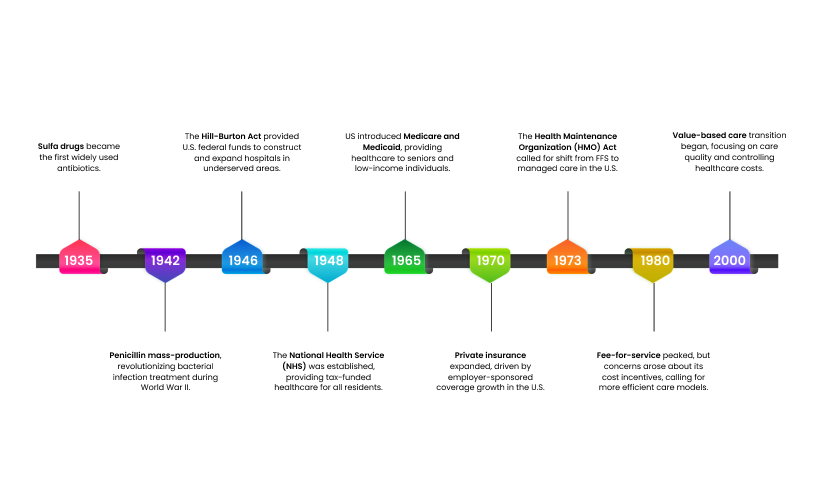
The healthcare delivery landscape has undergone a dramatic transformation since the years following World War II. This journey explores how we’ve arrived at the modern models of care we see today. In the post-war era, healthcare focused largely on episodic, reactive care in hospital settings. Technological advancements and a growing understanding of preventative medicine gradually led to a shift towards more comprehensive and proactive care models. This introduction sets the stage for our deep dive into this evolution. We’ll explore how healthcare delivery moved from physician-centered care to patient-centric models, and how technology and interconnected care systems are shaping the future of how we receive care
Developments after World War II (1945-1960s)
The years following World War II witnessed a surge in healthcare advancements and infrastructure development:
Medical advancements: The war spurred medical research, leading to breakthroughs like penicillin and sulfa drugs that revolutionized infection treatment. Technological innovations in blood transfusions, radiation therapies, and DDT use for malaria control further bolstered treatment options.
Healthcare infrastructure: The Hill-Burton Act in the US and the NHS in the UK exemplified government efforts to expand access to healthcare facilities through funding and construction initiatives. This period also saw the introduction of Medicare and Medicaid in the US, expanding coverage to vulnerable populations.
Government involvement: Governments played a crucial role by establishing funding mechanisms and building public healthcare systems like the NHS. This period highlighted the growing importance of government investment in ensuring equitable access to healthcare.
These developments laid the foundation for the modern healthcare landscape, characterized by ongoing medical research, a focus on accessibility, and a growing role for governments in healthcare infrastructure.
Rise of insurance players (1970s-2000s)
The concept of insurance has a long history, dating back millennia. However, the post-World War II era witnessed a significant surge in the prominence of insurance companies. This period marked a turning point for the industry, with several factors influencing this rise.
Emergence of private insurance and employer-sponsored plans: World War II wage freezes and tax policies led employers to offer health insurance as a benefit to attract and retain workers. This resulted in a significant rise of employer-sponsored health insurance plans.
Impact on access to healthcare services and financial protection for patients: The rise of insurance players notably improved access to healthcare services and provided substantial financial protection for patients by lowering out-of-pocket costs. Health insurance reduced the direct costs of medical care, encouraging more people to seek timely treatment and leading to better health outcomes.
Advent of fee-for-service (FFS) models: FFS became the dominant payment model after WWII due to its simplicity and clear compensation for providers. Transparency and provider control over earnings were factors driving its adoption by patients and providers.
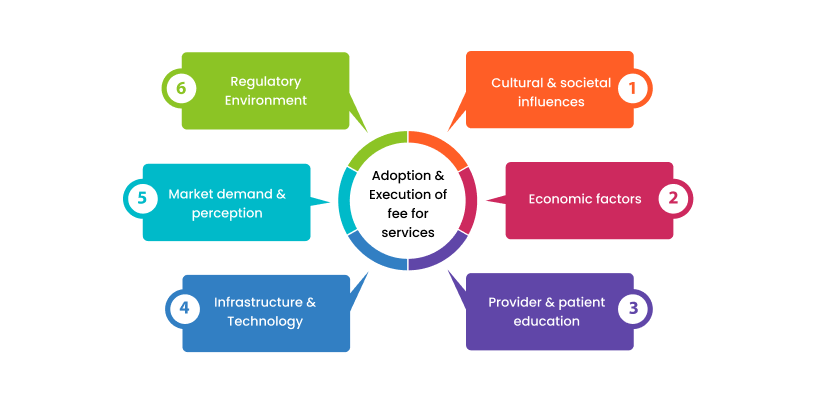
Factors Shaping FFS Adoption:
- Patient preference for transparency in costs
- Provider preference for control over practice and earnings
- Government policies and insurance frameworks
- Effective billing systems, electronic health records, and digital platforms
- Education for providers and patients on FFS benefits and drawbacks
- Economic considerations like cost-effectiveness and income disparities
- Cultural attitudes towards direct healthcare payments
Table: Advantages and Limitations of Fee-for-Service (FFS) Models
| Aspect | Advantages | Limitations |
| Administrative simplicity | Straightforward billing and reimbursement processes | Complexity in managing multiple services and claims |
| Service flexibility | Providers are equipped to deliver a wide variety of services. | Lack of standardized care pathways |
| Incentives for treatment | Encourages providers to offer more treatments | Potential for overutilization and unnecessary services |
| Patient choice | Patients have access to numerous healthcare providers. | Focus on quantity over quality of care |
| Revenue generation | Increased potential for revenue with more services | Can lead to high healthcare costs |
| Lack of preventive focus | Not incentivized to prevent illness | Limited emphasis on preventive care and wellness |
| Provider autonomy | Providers have control over treatment decisions | Variability in care quality and outcomes |
| Transparency in costs | Clear costs associated with specific services | Can be costly for patients without insurance coverage |
This period laid the foundation for the dominance of private insurance and fee-for-service models in healthcare, which continue to be influential today.
Shifting towards Value-based Care (2006-present)
The traditional fee-for-service (FFS) model, where providers are reimbursed per service rendered, is undergoing a significant transformation towards Value-Based Care (VBC). The two most relevant factors that are propelling the healthcare industry towards VBC are:
Rising healthcare costs: The ever-increasing cost of healthcare is unsustainable, prompting a search for more cost-effective models that deliver better value for the money spent.
Increased focus on population health and patient-centered care: The emphasis is shifting towards preventative measures, managing the health of entire populations, alongside prioritizing patient needs and preferences.
Furthermore, the FFS model has limitations that VBC aims to overcome:
FFS incentivizes volume over value: Providers might prioritize procedures that generate higher fees, potentially neglecting preventive care or coordination with other specialists.
Limited focus on patient outcomes: FFS doesn’t directly reward positive health outcomes, potentially leading to a disconnect between services offered and patient well-being.
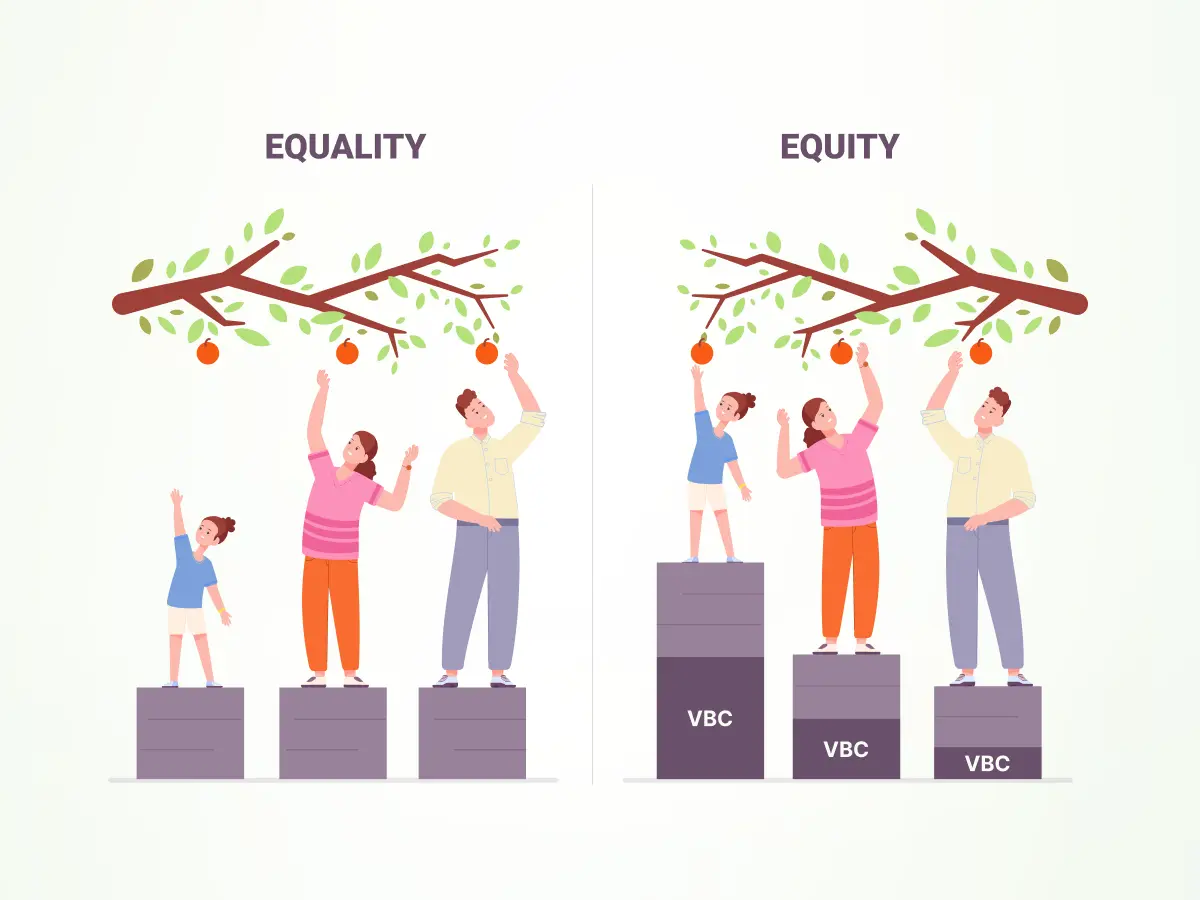
The value-based care model prioritizes quality and efficiency in healthcare delivery, focusing on measurable patient improvements at optimal costs. VBC tackles the shortcomings of FFS model by aligning financial incentives with patient well-being and encouraging preventative care and care coordination. This shift aims to create a healthcare system that delivers high-quality care at a sustainable cost, with the goal of better patient outcomes.
Let’s understand the fundamental principle of value-based care:
Principles of value-based care
VBC rests on three core, interconnected principles:
Patient outcomes: The primary focus shifts to improving a patient’s health and well-being through preventive care, chronic disease management, and improved care coordination. This is measured by tracking specific metrics such as patient readmission rates, A1C levels for diabetics, and blood pressure control.
Cost-effectiveness: VBC aims to deliver the best possible care while considering the economic constraints of the healthcare system. Cost-effectiveness analysis is a tool used to assess the relative cost and benefits of different treatment options, ensuring value for the money spent.
Accountability: Providers are held accountable for the quality and efficiency of the care they deliver. Financial rewards are tied to meeting predetermined performance metrics that reflect positive patient outcomes and cost-effectiveness.
For example, a VBC program might incentivize a group of cardiologists by providing a bonus if they can keep their patients’ cholesterol under control and reduce hospital readmission rates for heart attacks. This focus on population health management and preventative measures encourages a more holistic approach to patient care.
CMS predicts that national health expenditure will rise to 20% of GDP by 2025, while health care costs as a percentage of total family income will rise to unsustainable levels. Fortunately, value-based contracts can help improve the quality of care while slowing the cost curve.
Understanding care models
Care models detail how care is coordinated and delivered holistically within a value-based environment. The core focus is on quality of care, aiming at better outcomes and reduced costs. Care models define the service structure, administration, and strategies for improving health. While discussing the care models in VBC, we also need to discuss the payment models.
Integrating care and payment models for optimal healthcare delivery
Care models and payment models are two independent, yet closely connected, aspects of the US healthcare system. Care models detail how care is coordinated and delivered with an emphasis on prevention while payment models define how the providers are compensated. So, care models dictate what kind of care you provide (patient-centered, preventive, and so forth) whereas payment models decide how you are going to get paid (fee-for-service or value-based). Understanding both is critical to optimizing resources, improving patient care, and ensuring financial sustainability.
Payment mechanisms
The healthcare sector is going through a major change, as payment methods are evolving to tackle issues like controlling costs, enhancing quality, and satisfying patients. Here’s a quick look at the payment models currently being used in the US healthcare ecosystem.
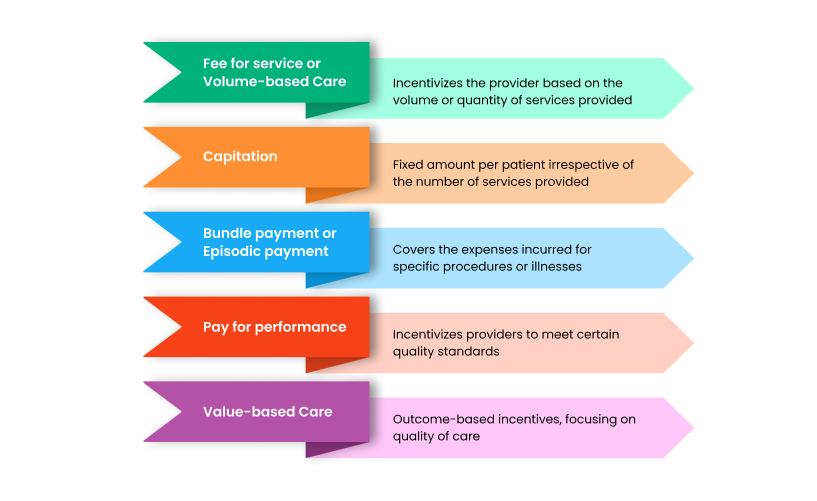
The best payment model probably involves a combination of various models to tackle specific healthcare issues. For instance, using capitation for primary care with bundled payments for complex procedures could be successful.
Traditional payment models and their limitations
1.Fee-for-service (FFS)
Until very recently (within the last three-four years) this model of care provision was the standard, evidenced by data from 2020, showing that nearly 2/3rds (64%) of care providers were compensated based on this methodology.
The reasoning behind the use of this model of care provision was sound:
- There was a lack of resources and technological advancements necessary to provide holistic care for patients
- It was the model of care that had been primarily used for a long time
- It allowed providers and their administrative staff to establish workflows that best fit their needs
But, it was not without its flaws. The lack of an all-encompassing method of care provision often meant that patients would only receive acute care; which subsequently meant that over time, patients would be handicapped from achieving absolute health and would have to financially suffer if further health problems were to arise.
2. Episodic care
Episodic care is best defined as, “a single encounter with a patient focused on a presenting concern(s), identified medical condition(s) or referred consultation, where neither the regulated member nor patient have the expectation of an ongoing care relationship.” An example of this would be a visit to urgent care.
Episodic care does provide acute/emergency care, however, it does also come with its own drawbacks. In many countries, such as the United States, a visit to the urgent care could result in the patient being burdened with heavy fees that financially hampers them long-term. It does also leave patients in the helpless situation of needing to find their own way if they require/want additional care.
3.Volume-based care
Often interchangeably used with fee-for-service model of care, volume-based care faces many of the same challenges. Since the provider is reimbursed per the quantity of services or procedures they render to the patient, this leads to issues such as:
- Providers taking a reactive approach to care provision
- Patients only receiving a solution to their present ailment, rather than understanding and addressing the underlying issues and taking preventive steps to address them.
- Providers possibly feeling pressured to administer unnecessary services or procedures
The traditional fee-for-service model rewarded healthcare providers based on the volume of services delivered, not necessarily the quality. To address this, the Centers for Medicare & Medicaid Services (CMS) has implemented various value-based care programs. These programs, like the Medicare Shared Savings Program and Accountable Care Organizations (ACOs), incentivize providers to deliver high-quality care that improves patient outcomes while controlling costs. This shift towards value-based care aims to achieve the “triple aim” of better individual care, improved population health, and reduced healthcare spending.
Key care models driving value-based care transformation
1. Accountable care organizations (ACOs)
The American Hospital Association describes accountable care organizations as “groups of clinicians, hospitals and other health care providers who come together voluntarily to give coordinated high-quality care to a designated group of patients.” This model of care has a preventative mindset, rather than a reactive one. While ensuring optimal patient health, the ACO model is dependent upon the savings that the organization (in many cases, Medicare) partnered with the ACO receives. This care model is effective in promoting care coordination between providers; ensuring that patients receive holistic care, reducing costs for both patients and the organization.
ACOs share these core features:
- Networks of providers: ACOs are groups of doctors, hospitals, and other healthcare professionals who work together.
- Defined patient population: They care for a specific group of patients, often determined by their relationship with ACO physicians.
- Financial accountability: ACOs are given a budget based on past spending for their attributed patients. They share any savings achieved under this target.
There are several ACO models catering to different needs:
- Medicare ACOs: Focus on improving care quality and reducing costs for Medicare beneficiaries (e.g., Shared Savings Program).
- Medicaid ACOs: Address the needs of low-income populations while focusing on value-based care.
- Commercial ACOs: Partner with private insurers to deliver high-quality care for a broader patient population.
- Integrated delivery systems (IDS): These tightly knit organizations have shared ownership of hospitals, physician practices, and sometimes insurance. They emphasize financial alignment, electronic health records, and coordinated care.
- Multispecialty group practices: Offer comprehensive care through a network of specialists, often affiliated with hospitals.
Cleveland Clinic’s Medicare ACO, serving over 148,000 patients in northeast Ohio, focuses on chronic disease management through multidisciplinary care teams. These teams include doctors, nurses, pharmacists, and social workers who collaborate to reduce unnecessary medical use, especially during care transitions. CCMACO operates under the Medicare Shared Savings Program, a value-based payment model that rewards quality care and cost savings. Their experience highlights the importance of teamwork, clear goals, and well-defined structures for successful implementation of such programs.
2.Patient-centered medical homes (PCMHs)
Patient-centered medical homes are “a model of care that puts patients at the forefront of care.” Much like ACOs, PCMHs are also focused on preventative care, and easing care management for those with on-going health problems through collaborative care co-ordination. Due to this approach, PCMHs are able to provide comprehensive care to their patients, allowing for increased overall wellness and reducing potential future healthcare costs.
Key characteristics of patient-centered medical homes (PCMHs):
PCMHs focus on building strong relationships between patients and their healthcare providers. They achieve this through several key features:
- Personal physician: You have a designated doctor for your initial care and ongoing needs.
- Team-based care: A team of healthcare professionals collaborates to manage your health.
- Whole-person care: They consider all aspects of your health, including preventive, chronic, and end-of-life care.
- Coordinated care: Care is coordinated across different healthcare providers and settings.
- Quality and safety: Evidence-based practices and tools ensure high-quality care.
- Enhanced access: Easier access to care through flexible scheduling and communication options.
- Payment reform: Reimbursement models that reward PCMHs for providing better value-based care.
Through this value-based care model, a Colorado-based PCMH reported a 15 percent decrease in emergency department visits, an 18 percent reduction in inpatient admissions, and a return on investment of $4.50 for every dollar spent. Another Maryland-based PCMH stated that it saved $98 million and increased its quality scores by 10 percent in one year.
3.Pay-for-performance programs
In this model of care provision, providers are reimbursed based on whether they were able to meet specific quality metrics.
4.Virtual care models
Utilizing digital technologies, such as telehealth and wearable technology, this care model aims to make access to care more easily accessible.
5.Chronic disease management models
This model focuses on the long-term management of chronic conditions to prevent complications and to improve patient well-being and quality of life.
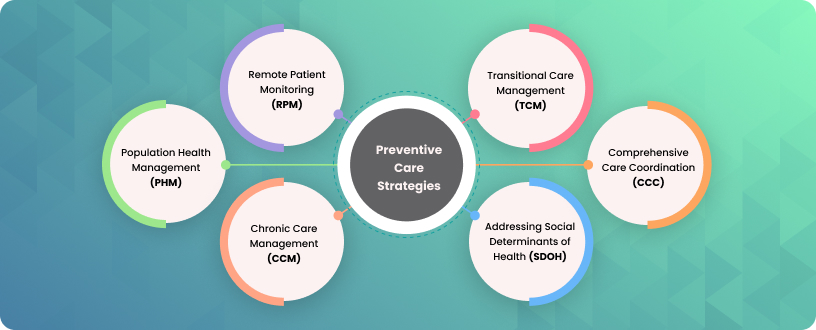
6.Population health management
Using technology such as data analytics, this model aims to service entire patient populations for preventive care and addresses social determinants of health that might be a factor in population health.
Key characteristics and components of population health management:
Long-term focus: Aims to achieve lasting improvements in health outcomes, not just quick fixes.
Equity-focused: Works to reduce health disparities between different groups.
Targeted interventions: Identifies subgroups within the population with specific needs and tailors interventions accordingly.
The above care models have the following advantages:
- Utilizing preventive care strategies can lower hospitalization rates and decrease costs, resulting in improved outcomes.
- Patient lifestyle data is also considered while prescribing medications which results in better adherence, further improving outcomes.
- Patients are more aware and involved in their treatment decisions, which helps improve adherence and outcomes.
- Artificial Intelligence simplifies processes, enabling providers to receive alerts from decision support systems that recommend personalized treatment plans based on the patient information provided.
- Cloud technology provides a centralized data repository for diagnostic purposes in different fields.
That brings us to how technology enables and empowers both providers and patients in their care journey. On one hand EHRs and hospital networks enable smoother operations and care coordination while patients get ample information and support on their fingertips with patient portals. Let’s explore the role of technology in effective implementation of VBC care models.
The role of technology in implementing care
The top barriers to adoption of VBC models can be tackled using robust technology solutions which makes technology a key element enabling VBC adoption. Technology has emerged as a critical enabler of value-based care (VBC) models, facilitating data-driven decision-making, improving care coordination, and enhancing patient engagement. Technology helps reduce cost, time and errors in healthcare. It also helps improve the quality of care by providing more accurate information and easing secure information transfer. Be it appointment scheduling, diagnosis, care coordination, patient engagement or reporting, technology plays a vital role in today’s healthcare ecosystem.
Electronic health records (EHR) and data analytics
Electronic Health Records (EHRs) have become the cornerstone of modern healthcare, serving as a repository for patient information and enabling data-driven decision-making. When coupled with robust analytics, EHRs can significantly contribute to improving care quality, ensuring patient safety, informing decision-making, and monitoring performance.
Improve care quality
- Comprehensive patient record: EHRs provide a comprehensive view of a patient’s medical history, including diagnoses, medications, allergies, treatment plans, and demographics. This enables healthcare providers to make informed decisions and deliver more effective care.
- Care coordination: EHRs facilitate communication and collaboration among healthcare providers, ensuring continuity of care and reducing medical errors.
- Evidence-based medicine: EHRs can be used to identify best practices and implement evidence-based guidelines, leading to improved patient outcomes.
- Reducing readmissions: By identifying patients at risk for readmission, hospitals can implement targeted interventions to prevent unplanned returns.
- Outbreak prediction: Analyzing data on infectious disease trends can help predict potential outbreaks, enabling proactive measures to be taken.
Ensure patient safety
- Medication reconciliation: EHRs help prevent medication errors by providing a complete list of medications and identifying potential interactions.
- Allergy alerts: EHRs can alert providers to patient allergies, reducing the risk of adverse drug reactions.
- Clinical decision support: EHRs can offer reminders, alerts, and suggestions to support clinical decision-making and prevent errors.
- Identifying high-risk patients: By analyzing patient data, predictive models can identify individuals at risk for developing specific conditions or experiencing adverse events. This allows for early intervention and preventive measures.
- Precision medicine: Identifying patient subgroups that may respond differently to treatments, leading to more personalized care.
Informed Decision-making - Population health management: EHR and data analytics can be used to identify high-risk patient populations and target preventive interventions.
- Resource allocation: Analyzing EHR data can help optimize resource allocation by identifying areas of high utilization and potential inefficiencies.
- Outcome measurement: Data analytics can extract EHR data to track patient outcomes and provide insights into the effectiveness of care interventions.
Performance monitoring
- Quality improvement: EHR data can be used to identify areas for quality improvement and track progress over time.
- Financial performance: EHRs can provide data on costs, revenue, and utilization, enabling organizations to monitor financial performance and identify opportunities for cost reduction.
- Regulatory compliance: EHRs can help healthcare organizations meet regulatory requirements by providing necessary data for reporting and auditing.
- Optimizing resource allocation: Predicting patient volumes, resource utilization, and staffing needs can help healthcare organizations allocate resources effectively.
Intermountain Healthcare is a notable example of an organization that has successfully leveraged EHRs and data analytics to improve care quality and patient safety. By implementing a comprehensive EHR system and utilizing advanced analytics, Intermountain has achieved significant reductions in mortality rates, hospital readmissions, and healthcare costs.
By harnessing the power of EHRs and data analytics, healthcare organizations can drive improvements in care quality, patient safety, and operational efficiency, ultimately contributing to the success of value-based care models. By leveraging predictive analytics, healthcare organizations can proactively address potential health issues, improve patient outcomes, and optimize resource utilization.
IoT and remote patient monitoring
The Internet of Things (IoT) has revolutionized healthcare by enabling continuous monitoring of patients outside of clinical settings. Through wearable devices and sensors, IoT devices collect and transmit patient health data to healthcare providers, enabling remote patient monitoring and improved care management.
Elements of internet of things (IoT) devices in enhancing patient monitoring and engagement
IoT devices play a pivotal role in empowering patients and enhancing their engagement in healthcare.
- Wearable devices: These include smartwatches, fitness trackers, and specialized medical devices that collect data on vital signs, physical activity, sleep patterns, and other health metrics.
- Remote monitoring equipment: Devices like blood pressure monitors, glucose meters, and oxygen sensors can be used to track chronic conditions and detect early signs of deterioration.
- Home sensors: These devices can monitor environmental factors such as temperature, humidity, and air quality, which can impact patient health.
- Patient portals: Online platforms that allow patients to access their health data, communicate with providers, and manage appointments.
- Ambient monitoring: By continuously tracking patient movements and behaviors, these systems can predict potential risks, such as falls, and alert care teams proactively. This allows healthcare providers to allocate their time and resources effectively, improving overall patient care.
By providing real-time data on patient health, IoT devices enable healthcare providers to identify potential issues early and intervene proactively. Furthermore, these devices empower patients to take an active role in managing their health by providing them with insights into their condition and progress.
Benefits in managing chronic conditions and reducing hospital readmissions
IoT-enabled remote patient monitoring offers significant benefits in managing chronic conditions and reducing hospital readmissions.
- Early detection of exacerbations: By continuously monitoring vital signs and other health metrics, IoT devices can detect early signs of deterioration in patients with chronic conditions, allowing for timely interventions to prevent hospitalizations.
- Improved medication adherence: Remote monitoring can help ensure patients are taking their medications as prescribed, reducing the risk of adverse events and hospitalizations.
- Enhanced patient engagement: By providing patients with real-time data on their health, IoT devices can motivate them to take an active role in managing their condition.
- Reduced healthcare costs: By preventing hospitalizations and reducing the length of stay, IoT-based remote patient monitoring can lead to significant cost savings.
For example, patients with chronic heart failure can use wearable devices to monitor their heart rate, blood pressure, and oxygen levels. If any abnormalities are detected, alerts can be sent to healthcare providers, enabling early intervention and preventing decompensated heart failure, which often leads to hospitalization.
By effectively leveraging IoT technology, healthcare providers can improve patient outcomes, reduce healthcare costs, and enhance the overall patient experience.
Digital tools and patient engagement
Digital tools play a pivotal role in empowering patients to take an active role in their healthcare journey. By providing patients with access to information, communication channels, and self-management tools, these technologies can significantly enhance patient engagement and improve health outcomes.
Mobile health applications and patient portals for empowering patients
Mobile health applications and patient portals offer a range of functionalities that empower patients to manage their health effectively.
Access to health information: Patients can view their medical records, test results, and medication history through patient portals.
Appointment scheduling: Patients can conveniently book, reschedule, or cancel appointments online.
Secure messaging: Patients can communicate with healthcare providers through secure messaging platforms.
Health education resources: Patients can access educational materials on various health conditions and preventive measures.
Remote monitoring: Certain applications allow patients to monitor their health conditions using wearable devices and share data with healthcare providers.
A recent study published in International Journal of Science and Research Archive highlights the effectiveness of mobile health apps in managing chronic conditions, promoting healthy behaviors, and improving overall health outcomes.
Strategies for enhancing patient participation in their own care
To maximize the impact of digital tools, healthcare organizations should employ strategies to foster patient participation in their own care.
- Personalized content: Tailoring health information and recommendations to individual patients based on their health conditions, preferences, and demographics.
- Human touchpoints: Combining digital tools with human interaction to provide personalized support and address patient concerns.
- Gamification: Incorporating game-like elements to motivate patients to engage with health-related activities.
- Patient education and support: Offering educational resources and support programs to help patients understand their health conditions and manage their care.
- Incentives: Providing incentives for patients to engage with digital tools and participate in their care.
Kaiser Permanente’s use of personalized health coaching and patient education programs has demonstrated success in improving patient engagement and health outcomes. By combining digital tools with human support, Kaiser Permanente has empowered patients to take an active role in managing their chronic conditions.
By implementing these strategies and leveraging the power of digital tools, healthcare organizations can foster a culture of patient engagement, leading to improved health outcomes and increased patient satisfaction.
Technology serves as a cornerstone in the successful implementation of value-based care (VBC) models. By leveraging electronic health records, IoT devices, and digital tools, healthcare organizations can enhance patient engagement, improve care coordination, and optimize resource allocation. Digitally enabled care models, such as telehealth and remote patient monitoring, are reshaping healthcare delivery by providing accessible, convenient, and personalized care. As technology continues to advance, its integration into VBC will be essential for achieving optimal patient outcomes and driving long-term sustainability.
Barriers to the adoption of value based care model
While technology offers a powerful foundation for implementing VBC models, achieving widespread adoption requires overcoming significant hurdles. Let’s delve into the key challenges that healthcare organizations currently face in transitioning towards value-based care.
Reluctance:
The majority of healthcare practices already have existing workflows and practices that service their needs adequately. The prospect of possibly reworking them or starting anew could be seen as unnecessary or not worth the effort. For some, it might even be seen as possibly detrimental.
One way to address resistance to VBC is to educate providers on the value it offers. Explain the rationale behind the shift and showcase real-world examples demonstrating the benefits for both patients and providers in achieving their goals. Staff buy-in is crucial for successful implementation. Involving them in workflow design ensures everyone understands the changes. Regular feedback sessions such as meetings or surveys help understand the gaps, realign and improve.
Financial viability:
Shifting from a fee-for-service model (which promises more financial stability) to a value-based care model might place some providers in a difficult position as they would now need to fulfill the objectives by their regulatory bodies (such as Medicaid) to receive reimbursement for care rendered. But the providers cannot guarantee that a medical interaction will always lead to the desired positive outcome for the patient. However, the benefit of a value-based care model of treatment from a financial point of view is that while it gives the patients the benefit of saving on costs, it also benefits the provider by reducing their risk of not receiving reimbursement by evaluating their results by accounting for the health outcomes for the group as a whole, rather than on an individual basis.
Technological challenges:
Presently, in the United States, the Health Insurance Portability and Accountability Act of 1996 (HIPAA) law is enacted and uniformly adopted by all involved in the healthcare ecosystem. It ensures that patient health data stays secure and private.
In a VBC model, it requires two or more care providers to work together and communicate sensitive patient health data, potentially risking the patient information privacy. Moreover, they should also be able to communicate the data through an encrypted pathway which cannot be interrupted or influenced by any third parties. This presents a challenge to a significant portion of the healthcare providers currently using a standard Electronic Health Records (EHR) system, as most of these legacy software providers do not equip their system with API capabilities or 3rd party integration.
While it might seem like another tiresome task, the most financially prudent option here is to adopt a competent and secure EHR system that can seamlessly integrate with other EHR systems to communicate data without corrupting its integrity. This would make administrative tasks, such as collecting and communicating patient health data, more streamlined and less vulnerable to potential inaccuracies, thus reducing the need for manual processes, which would result in the reduction of possible staff burnout.
Considering that the VBC models aim to achieve quality care and reduce healthcare costs, such barriers can be overcome tactically using the right technology and resources. CMS has already established a goal to have 100% of Original Medicare and the majority of Medicaid be on value-based contracts by 2030.
Integrating social determinants of health (SDOH)
The US spends the most on healthcare among developed nations, yet has high poverty rates, income inequality, and poor health outcomes. Access to medical care is important, but factors like socioeconomic status, education, and environment significantly impact health. The healthcare ecosystem must consider social determinants of health to address health inequities and improve population health outcomes.
Understanding SDOH
Social determinants of health (SDOH) are the social and economic factors that influence your health outcomes. These are matters like your education level, income, access to safe housing and healthy food, and the quality of your environment. For example, someone living in a community with limited access to fresh fruits and vegetables may be more likely to experience diet-related health problems.
The role of social determinants in influencing health outcomes
Social Determinants of Health can have a greater impact on a person’s health than medical care or lifestyle choices. Understanding and addressing SDOH is crucial for Value-Based Care initiatives because they directly impact patients’ health needs and resource utilization.
Here are some key aspects to consider:
Limited access to quality healthcare: Low income, lack of transportation, or inadequate health insurance can limit access to preventative care, screenings, and treatment. This can lead to delayed diagnoses, poorer management of chronic conditions, and higher healthcare costs down the line.
Health behaviors: SDOH can influence health behaviors. For example, residents of communities with limited access to fresh fruits and vegetables or safe places to exercise may be more likely to have unhealthy diets or be physically inactive.
Environmental factors: Exposure to environmental hazards like air or water pollution can increase the risk of respiratory problems, asthma, and other health issues.
A diabetic patient living in a food desert may struggle to manage their blood sugar due to limited access to healthy groceries. VBC programs could address this by partnering with local food banks or delivery services to ensure access to healthy food options. Another aspect is a low-income patient skipping preventive screenings due to cost concerns. VBC models could incorporate financial assistance programs or offer flexible scheduling to improve access to preventive care.
Strategies for integrating SDOH into care models to promote health equity
Covid-19 highlighted existing health inequities rooted in social determinants of health. Vulnerable populations faced disproportionate impacts due to SDOH factors. Access to resources like healthcare, employment, and housing played a crucial role in outcomes. This asserted the fact that addressing SDOH is essential for mitigating disparities and promoting health equity during pandemics. Because SDOH significantly affects health outcomes, addressing these factors alongside medical care can improve health overall, especially for disadvantaged communities. This means healthcare providers may need to consider a patient’s social circumstances and medical conditions to provide the best possible care.
Considering the current technological disruptions and socio-economic developments, the WHO suggests the following strategies for integrating SDOH into care models to promote health equity:
1.Monitor social determinants of health (SDOH) to identify inequities
Regularly collect data on factors like income, education, housing, and access to healthcare across your patient population. Utilize SDOH screening tools during intake or patient portals. Partner with community organizations to gather data on social services available in your region.
A VBC program that identifies a specific zip code having a higher rate of asthma is investigated which reveals limited access to parks and green spaces in the area, suggesting a link to environmental factors.
2.Disaggregate data to understand disparities and inform interventions
Analyze SDOH data segmented by demographics like race, ethnicity, and socioeconomic status. Develop reports that show how SDOH factors vary among patient groups. Use this data to identify populations experiencing health inequities.
Data shows that diabetic patients with low income have higher rates of uncontrolled blood sugar. This could inform interventions like providing access to affordable healthy food options.
3.Strengthen capacity-building for data collection and analysis
Train staff on collecting and interpreting SDOH data. Invest in data management and analytics tools. Provide workshops on SDOH and data collection techniques for healthcare personnel. Partner with data scientists to develop tools for analyzing SDOH data effectively.
Train care coordinators to use SDOH screening tools and integrate them into patient workflows.
4.Translate data into policy actions to address health inequities
Use data to advocate for policies that address upstream social factors impacting health. Partner with community organizations and policymakers to develop interventions based on identified needs. Secure funding for programs that target SDOH.
Data reveals a high correlation between food insecurity and poor glycemic control. A VBC program advocates for increased access to SNAP benefits in their community.
5.Collaborate with stakeholders for regional and global monitoring of SDOH
Partner with other healthcare organizations and public health agencies to share data and best practices. Participate in regional health information exchanges to gain insights into broader population health trends. Collaborate on grant proposals to secure funding for SDOH initiatives.
A VBC program collaborates with a local public health department to develop a community garden project in a neighborhood with limited access to fresh produce.
By implementing these strategies, VBC programs can gain a deeper understanding of the social factors influencing health outcomes in their patient populations. This data can then be used to develop interventions aimed at reducing health inequities and achieving better health outcomes for all.
Addressing disparities in access and outcomes
Healthcare disparities exist when certain population groups experience poorer health outcomes or have less access to quality care compared to others. Here, we explore approaches to reduce these disparities and improve access for underserved communities, along with the importance of community engagement in addressing social determinants of health.
Approaches for reducing healthcare disparities and improving access to care for underserved populations
To reduce health disparities, a larger spectrum of stakeholders and authorities including the WHO and CIS must be involved as it requires regulatory changes and monitory subsidies at least in the beginning stages. The following points touch upon some such actionable approaches:
1. Collect and analyze data: Gather and analyze data on disparities in access and outcomes to identify trends and disparities. Use this information to inform decision-making and prioritize interventions that target the most pressing issues.
2. Address systemic inequalities: Identify and address systemic barriers that contribute to disparities, such as discriminatory policies and practices that perpetuate inequality. Implement policies and initiatives that promote equity and level the playing field for all individuals.
3. Increase funding and resources for underserved communities: Invest in programs and services that target specific disparities in access to healthcare, education, employment, and other essential services.
4. Improve education and awareness: Provide education and outreach programs to raise awareness about disparities and promote understanding of the root causes. This can help empower individuals to advocate for themselves and access the resources they need.
5. Support community-led initiatives: Collaborate with community organizations and leaders to develop and implement value based care solutions that address the unique needs of underserved populations. Empower communities to drive change from within and advocate for their own interests.
6.Increase diversity and representation: Ensure that decision-making bodies, institutions, and organizations reflect the diversity of the populations they serve. This can help ensure that policies and initiatives are inclusive and responsive to the needs of all individuals.
7. Foster collaboration and partnerships: Bring together stakeholders from various sectors, including government, non-profit organizations, healthcare providers, and community members, to work together towards addressing disparities in access and outcomes. Collaboration can help leverage resources and expertise to drive meaningful change.
8. Expand health insurance coverage: Public programs like Medicaid and subsidies for private insurance can significantly increase access for low-income populations
9. Culturally and linguistically appropriate services (CLAS): Providing healthcare services and materials in patients’ preferred languages and addressing cultural sensitivities improves communication and trust, leading to better health outcomes
10. Telehealth and mobile health (mHealth): Technologies like video conferencing and smartphone apps can expand access to care in geographically isolated areas or for patients with transportation barriers
11. Sliding scale fee clinics and community health centers: These facilities offer reduced-cost or free care to low-income and uninsured patients, increasing access to essential healthcare services
Importance of community engagement and partnerships in addressing social determinants
Social determinants of health (SDOH) are deeply rooted within communities. Building strong partnerships with community organizations allows for a deeper understanding of the population’s specific needs. Community engagement and partnerships can address social determinants by:
1.Identifying community needs: Partnering with community organizations helps healthcare providers understand the specific challenges faced by their patient population
2. Developing culturally appropriate interventions: Community collaboration ensures interventions address the unique needs and preferences of the population
3. Increasing access to resources: By engaging with community members and forming partnerships with local organizations, resources such as food banks, healthcare services, and educational programs can be made more accessible to those in need.
4. Providing education and information: Community engagement efforts can help raise awareness about social determinants of health and provide information on how individuals can overcome barriers to accessing resources and services.
5. Advocating for policy change: By working together with community members and organizations, partnerships can advocate for policy changes that address systemic issues that contribute to social determinants of health, such as affordable housing, access to healthcare, and quality education.
6. Building social support networks: Community engagement activities can help build social support networks that provide individuals with the resources and connections they need to address social determinants of health, such as job training programs, mental health services, and childcare assistance.
7. Empowering communities: By involving community members in decision-making processes and giving them a voice in shaping policies and programs that affect their lives, partnerships can empower communities to address social determinants of health in a way that is meaningful and sustainable.
By implementing these approaches and fostering strong community partnerships, healthcare systems can move towards a more equitable future where everyone can achieve optimal health.
Regulations and policies that impact value-based care models
Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) established a new “value-based” payment system and Quality Payment Program (QPP) with financial rewards and risks for providers transitioning away from fee-for-service models.
Affordable Care Act (ACA) introduced the Center for Medicare & Medicaid Innovation (CMMI) testing alternative payment models, and the Medicare Shared Savings Program (MSSP), a national ACO program.
Anti-Kickback Statute and Stark Law originally aimed to prevent fraud in fee-for-service but can be barriers to collaboration in value-based care. Recent reforms allow for more flexibility.
Medicaid Drug Rebate Program (MDRP) impacts affordability and accessibility of medications within value-based models. Regulations are being reviewed to adapt to new treatments.
Hospital Readmissions Reduction Program (HRRP) is a value-based purchasing program that financially incentivizes hospitals to reduce avoidable readmissions through improved communication and care coordination.
HIPAA Privacy Rule protects patient privacy but can limit data sharing for care coordination. Recent modifications aim to address this.
State-Driven Initiatives exist to further support the move towards value-based care.
Future directions and potential developments
The healthcare ecosystem is rapidly transforming along with evolving technological advancements, changing patient expectations, and the imperative to deliver high-quality, cost-effective care. Value-based care (VBC) models are at the forefront of this evolution, and their future trajectory is closely intertwined with emerging trends and innovations.
The age of responsible AI: Partner, not alternative
AI and machine learning are poised to revolutionize healthcare delivery and drive the evolution of VBC models. Despite AI being considered a disruptor, the most optimal way to use AI is to be a tech-partner to improving results than an alternative to human resources. Responsible AI in healthcare utilizes technology’s potential to enable and empower patients, improve accuracy and reduce biases in diagnoses, and safeguard trust without replacing human judgment and transparency. It can be a powerful partner for providers, clinical teams, payers, and self-funded employers.
- The potential of artificial intelligence and machine learning in transforming healthcare delivery: These technologies offer immense potential to analyze vast datasets, identify patterns, and make predictions, enabling more precise and personalized care. Advanced data management tools that ingest, cleanse, normalize, and stitch data to each patient from the vast resources of information available can ease the workload of healthcare professionals letting them focus more on providing better care.
For example, AI-powered chat bots can provide initial patient triage, answer frequently asked questions, and schedule appointments, freeing up healthcare professionals to focus on complex patient cases.
- Innovative care models leveraging AI for improved outcomes: By combining AI with other technologies, such as IoT and wearables, innovative care models can be developed.
- Streamlining prior authorization: A recent American Medical Association survey revealed the frustrations many healthcare professionals experience because of prior authorizations. Currently, physicians and their staff spend an average of 14 hours per week, or approximately 728 hours per year, completing prior authorizations. AI-powered tools can streamline this process by automating decision-making, leading to faster approvals and improved patient outcomes.
- The internet of medical things (IoMT): IoMTs are the future of healthcare systems where every medical device will be connected and monitored over the Internet by healthcare professionals. This evolving technique is expected to offer faster care at lower cost over time.
- Predictive interventions: Even though predictive intervention is being used by several healthcare organizations for preventive care, a larger percentage of users is yet to benefit from this technological evolution. Predictive interventions help with:
- Real-time health risk assessments using IoT and wearable data
- Proactive interventions based on predictive modeling
- Automated patient outreach for preventive care
- Integrated virtual care ecosystems: The future will see more virtual care ecosystems with more user-friendly infrastructure. Seamless integration of in-person, telehealth, and remote monitoring services will increase accessibility and reduce the cost of healthcare. The following care models are in their experimental process:
- Virtual-first care models for specific conditions
- AR/VR technologies for remote consultations and treatments
Focus on population health
One of the major aspects of VBC is the shift toward population health management. By focusing on the health of entire populations rather than individual patients, healthcare organizations can prevent diseases, manage chronic conditions effectively, and reduce overall healthcare costs.
- Shifting from episodic care to population health management: This involves moving away from a fee-for-service model to one that rewards providers for improving the health of a defined population. Accountable Care Organizations (ACOs) are a prime example of this shift, as they focus on coordinating care for a specific population and sharing in the financial rewards or penalties based on the overall health of the population.
- Emphasis on preventive care and early intervention to enhance overall health outcomes: By investing in preventive services, such as vaccinations, screenings, and health education, healthcare organizations can identify and address health risks early, reducing the likelihood of costly complications. For example, implementing population-wide wellness programs, including exercise initiatives, and nutrition counseling can help prevent chronic diseases like diabetes and heart disease.
Universal health coverage (UHC)
The concept of Universal Health Coverage (UHC) was first proposed in 2005 by the World Health Organization (WHO) to ensure that all individuals and communities have access to the health services they need without suffering financial hardship. Despite progress since 2000, global advancements towards UHC have slowed, with 4.5 billion people not fully covered by essential services in 2021. The COVID-19 pandemic exacerbated these challenges, disrupting essential services in most countries. It was highlighted as a key target in the United Nations Sustainable Development Goals (SDGs) in 2015, particularly in SDG 3.8, which aims to achieve UHC by 2030. The goal emphasizes the importance of access to essential health services, quality care, and financial protection for everyone, everywhere.