At its heart, care coordination is the art and science of orchestrating a patient’s healthcare journey across multiple providers, settings, and time. It’s about ensuring that every interaction, from a primary care visit to a specialist consultation and beyond, is aligned and working towards the best possible outcome for the individual. In the context of value-based care, where the focus shifts from volume to value, effective care coordination isn’t just a nice-to-have – it’s a fundamental necessity.
Now, picture trying to conduct that complex orchestration without a shared musical score. The result? Fragmented efforts, duplicated tests, and a frustrating experience for both patients and providers. This is where integrated EHR systems step onto the stage as the indispensable conductor’s baton. By providing a single, unified platform for all patient data – from medical history and medications to real-time updates and shared care plans – these systems break down the silos that have long plagued healthcare. They empower seamless communication and collaboration, laying the groundwork for truly coordinated and effective care management. The Office of the National Coordinator for Health Information Technology (ONC) emphasizes the importance of EHRs in improving care quality and coordination.
Understanding care coordination in value-based care
Care coordination involves proactively organizing and sharing information among all individuals and entities involved in a patient’s care. This includes primary care physicians, specialists, nurses, social workers, family members, and, most importantly, the patient themselves. Key concepts underpinning effective care coordination include:
- Communication: Clear, timely, and accurate exchange of information.
- Collaboration: Working together towards shared goals for the patient’s well-being.
- Information sharing: Seamless access to relevant patient data across the care continuum.
- Transition management: Ensuring smooth movement of patients between different care settings.
- Patient engagement: Actively involving patients in their care plans and decisions.
Types of coordination in value-based care
Care coordination isn’t a one-size-fits-all concept. It manifests in different ways:
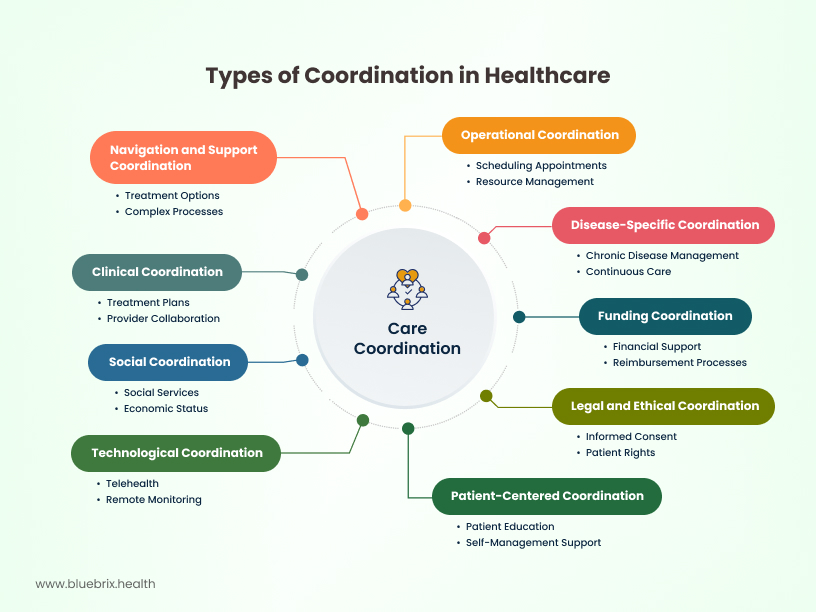
Clinical Coordination: Clinical coordination is focused on making sure that patients receive the appropriate treatment from the different healthcare providers involved in providing treatment.
- Disease-specific coordination: This type of coordination pertains specifically to the treatment of patients suffering from chronic diseases (such as diabetes or mental health problems) and aims to ensure that they receive on-going and continuous, uninterrupted care.
- Funding coordination: This form of coordination focuses on providing financial support for the patient and proper reimbursement processes for the provider by addressing the financial aspects of the care management process (treatment plans, payer management, etc.)
- Social coordination: By integrating social services (ex: support groups) with healthcare, this type of coordination addresses the factors affecting the patient’s overall health, outside of just their immediate health concerns. This would include their economic status, their employment status, environmental factors, and more.
- Technological coordination: Enhances care management and better informs the provider on their patients’ health through the integration of technological tools such as telehealth, remote monitoring, and patient engagement tools.
- Legal and ethical coordination: Focuses on addressing legal matters related to care provision (informed consent, the rights of the patient, permission to share sensitive health data, etc.) and prevention of ethical lines being crossed.
- Navigation and support coordination: Designed to assist and support patients in managing the complex processes that might arise when navigating treatment options.
- Operational coordination: Deals with the logistical aspects of care delivery, including scheduling appointments, managing resources, and ensuring efficient workflows. Think about how a hospital coordinates admissions, discharges, and bed management.
- Patient-centered coordination: Places the patient at the heart of the coordination efforts. It involves understanding their needs, preferences, and goals, and tailoring care plans accordingly. This might include providing patient education, support for self-management, and addressing social determinants of health.
Challenges in traditional care coordination
Traditional care coordination often faces significant hurdles:
- Fragmented information: Lack of interoperability between disparate systems leads to information silos, making it difficult for providers to get a complete picture of a patient’s health journey.
- Communication gaps: Poor communication between different providers and care settings can result in duplicated tests, medication errors, and delays in care.
- Manual processes: Reliance on manual processes like phone calls, faxes, and paper records is inefficient, time-consuming, and prone to errors.
- Lack of accountability: Without clear roles and responsibilities, it can be challenging to ensure that all aspects of a patient’s care are addressed.
- Patient disengagement: Patients may feel lost or overwhelmed if they are not actively involved in their care planning and lack the tools to manage their health effectively.
Benefits of effective care coordination
Overcoming these challenges through effective care coordination yields significant benefits:
- Improved patient outcomes: Better management of chronic conditions, reduced hospital readmissions, and enhanced overall health. A study published in Health Affairs highlights the link between care coordination and improved outcomes.
- Reduced healthcare costs: Prevention of unnecessary tests and procedures, decreased emergency room visits, and more efficient resource utilization.
- Enhanced patient experience: Increased satisfaction, better understanding of their care plan, and improved adherence to treatment.
- Increased provider satisfaction: Streamlined workflows, better communication, and the ability to deliver more effective care.
- Improved quality metrics: Better performance on key quality indicators like HEDIS and MIPS, which are crucial in value-based care models.
The role of integrated systems in care coordination
Integrated systems in healthcare refer to a network of technologies and processes that are designed to work together seamlessly, sharing data and coordinating workflows across different departments, settings, and even organizations. Think of it as moving from a collection of isolated apps on your phone to a unified operating system where everything communicates and functions harmoniously. In healthcare, this primarily revolves around a central EHR system that connects various modules and external platforms.
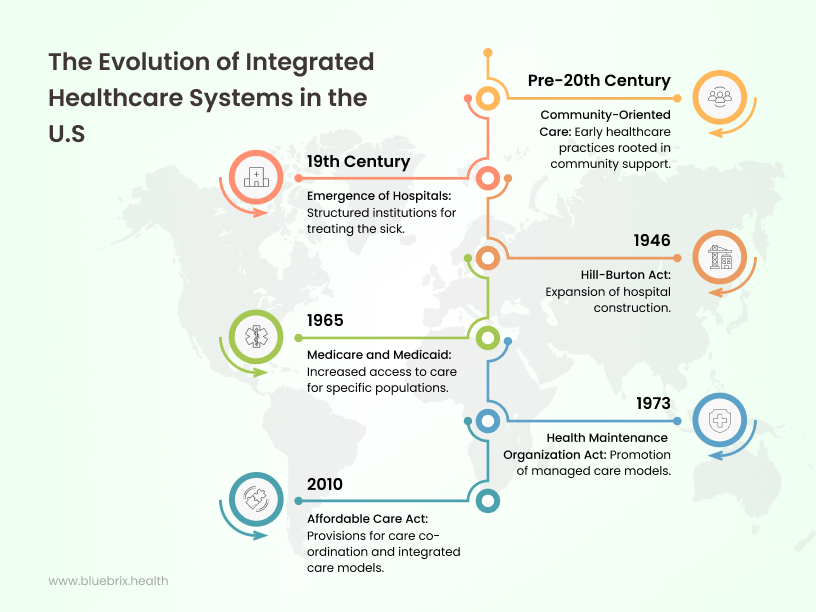
Historically, healthcare in the U.S. was characterized by fragmented, siloed systems where different providers and institutions operated independently, often with incompatible record-keeping methods. The journey towards integrated healthcare systems has been a gradual but significant shift, driven by the recognition that better coordination is essential for improving quality and controlling costs. This evolution has seen a move from paper-based records to disparate electronic systems and now towards interconnected digital ecosystems where data flows freely and securely.
The role of federal policies (HITECH, MACRA, CMS Interoperability Rule)
Several federal policies have played a pivotal role in accelerating the adoption of integrated healthcare systems:
- Health information technology for economic and clinical health (HITECH) Act (2009): This legislation provided significant incentives for the adoption and meaningful use of EHRs, laying the foundation for digital record-keeping across the country.
- Medicare access and CHIP reauthorization act (MACRA) (2015): This act shifted the focus from fee-for-service to value-based care, incentivizing providers to deliver high-quality, coordinated care. It established the Quality Payment Program (QPP), which includes MIPS and Advanced APMs, both requiring effective data sharing and coordination.
- CMS interoperability and patient access final rule (2020): This rule aims to improve patient access to their health information and promote data exchange between payers and providers through open APIs.
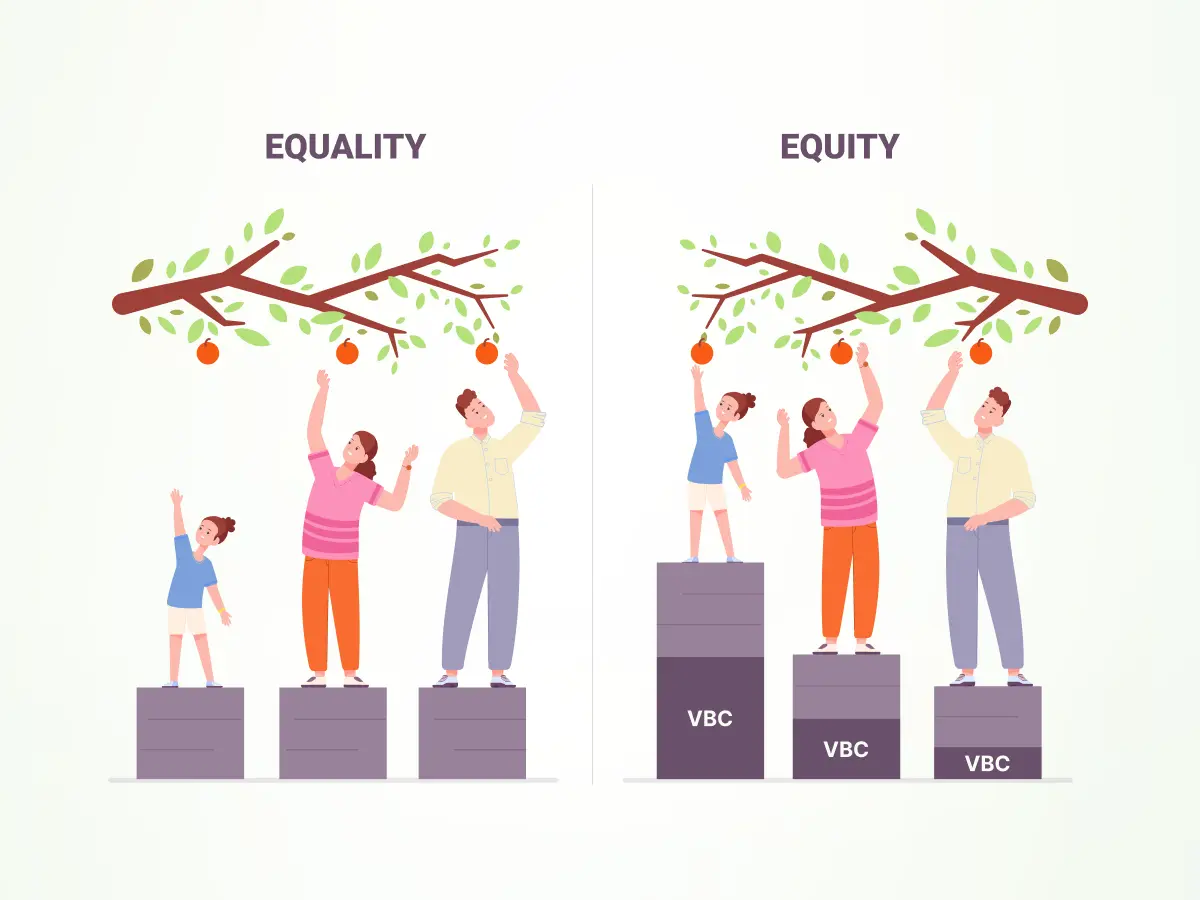
The push toward value-based and population health models
The increasing adoption of value-based care (VBC) and population health management (PHM) models is a significant driver for integrated healthcare systems. VBC emphasizes paying providers based on patient outcomes rather than the volume of services, inherently requiring better coordination to manage the total cost of care and improve patient health. PHM focuses on improving the health of a defined population, necessitating robust data analytics, proactive outreach, and coordinated care delivery across various settings.
Key components of integrated systems
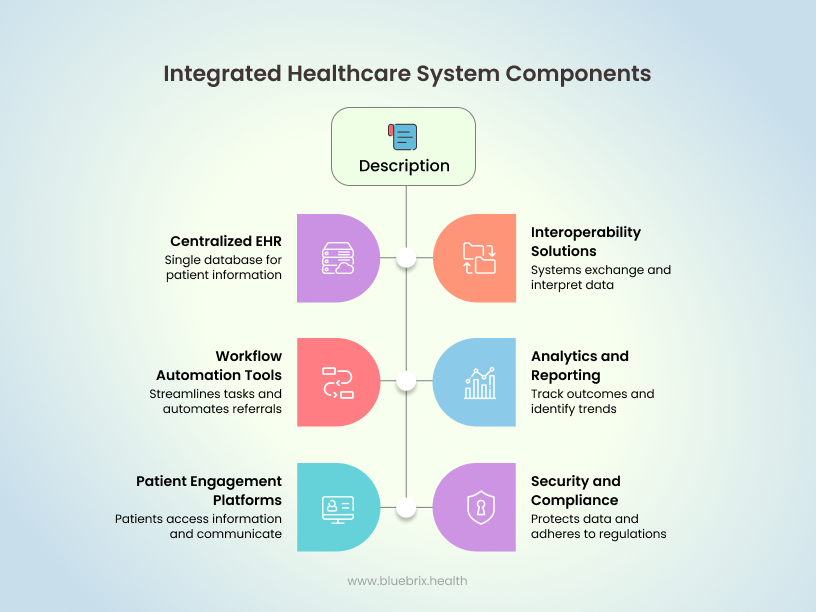
Several key components contribute to a truly integrated healthcare system:
- A centralized EHR: This forms the backbone, housing all patient information in a single, accessible database.
- Interoperability solutions: Technologies and standards that enable different systems (even those from different vendors) to exchange and interpret data effectively.
- Workflow automation tools: Features that streamline routine tasks, automate referrals, and manage care transitions.
- Analytics and reporting capabilities: Tools that allow providers to track patient outcomes, identify trends, and make data-driven decisions.
- Patient engagement platforms: Portals and applications that enable patients to access their health information, communicate with their care team, and participate in their care.
- Security and compliance frameworks: Robust measures to protect patient data and adhere to regulations like HIPAA.
How integrated systems improve care coordination
Integrated systems are the engine that drives effective care coordination by:
- Breaking down information silos: Providing a single source of truth for patient data, accessible to all authorized care team members, regardless of their location or specialty.
- Facilitating seamless communication: Enabling secure and efficient communication between providers, patients, and other stakeholders through features like secure messaging and shared care plans.
- Streamlining workflows: Automating tasks such as referrals, appointment scheduling, and medication reconciliation, reducing administrative burden and the risk of errors.
- Providing real-time insights: Offering analytics and decision support tools that help providers identify patients at high risk, track progress against care goals, and make timely interventions.
- Empowering patients: Giving patients access to their health information and tools for self-management, fostering greater engagement in their care.
- Improving transitions of care: Ensuring that critical patient information follows them as they move between different care settings, reducing the likelihood of adverse events and readmissions. blueBriX’s integrated EHR is designed with seamless data sharing and communication at its core, addressing the common challenges of fragmented care.
Pillars of integration that drive effective coordination
Effective care coordination through integrated systems rests on several key pillars:
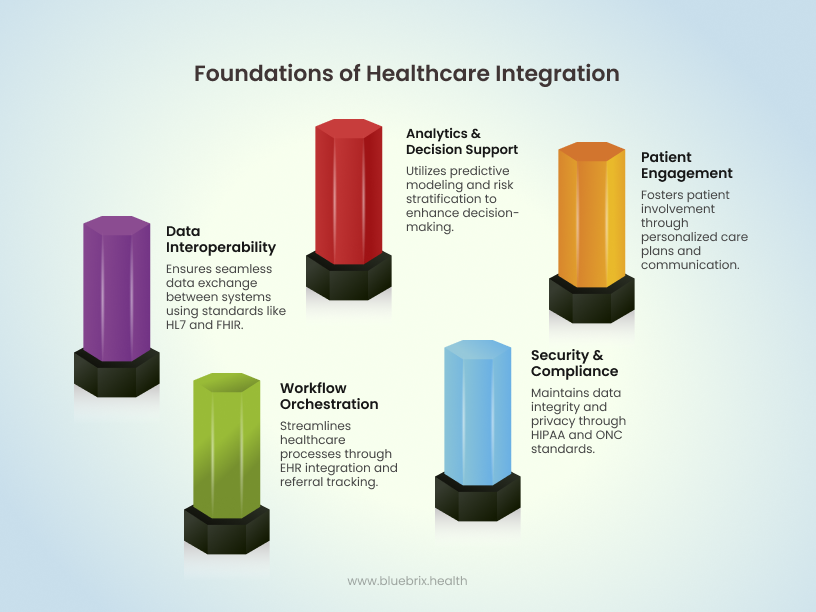
Data interoperability: HL7, FHIR, API-led connectivity
Data interoperability is the ability of different information systems to access, exchange, integrate, and cooperatively use data in a coordinated manner. This is crucial for a holistic view of the patient. Key standards and technologies enabling interoperability include:
- Health level seven international (HL7): A set of international standards for the exchange, integration, sharing, and retrieval of electronic health information. HL7 standards like HL7v2 have been foundational for data exchange for decades.
- Fast healthcare interoperability resources (FHIR): A newer generation of HL7 standards that leverages modern web technologies (like RESTful APIs and JSON) to make data exchange more seamless and efficient. FHIR is designed to be easier to implement and more adaptable to various use cases.
- API-led connectivity: Using Application Programming Interfaces (APIs) to enable different software systems to communicate and share data in a standardized way. This allows for more flexible and modular integration. blueBriX leverages modern API-led connectivity and supports FHIR standards to ensure seamless data exchange with other systems.
Workflow orchestration: EHR integration, referral tracking
Integrated systems facilitate the orchestration of clinical workflows, ensuring smooth transitions and timely interventions:
- EHR integration: Embedding tools and functionalities within the EHR to manage various aspects of care coordination, such as scheduling, documentation, and communication.
- Referral tracking: Systems that automate and track the referral process, ensuring patients see the right specialists in a timely manner and that relevant information is shared efficiently. This includes electronic referrals (e-referrals) and automated follow-up reminders.
Analytics & decision support: Predictive modeling, risk stratification
Integrated systems provide powerful analytics capabilities to support proactive and informed care:
- Predictive modeling: Using historical data to identify patients at high risk for certain conditions or adverse events, allowing for early interventions. For example, predictive models can help identify patients at high risk of hospital readmission.
- Risk stratification: Categorizing patients based on their risk factors and healthcare needs, enabling providers to tailor care plans and allocate resources effectively.
Patient engagement: Multichannel communication, personalized care plans
Engaging patients is a critical aspect of care coordination, and integrated systems offer tools to facilitate this:
- Multichannel communication: Enabling communication with patients through various channels, such as secure messaging within patient portals, email, SMS, and video conferencing.
- Personalized care plans: Creating and sharing individualized care plans with patients through digital platforms, empowering them to actively participate in their health management. blueBriX offers robust patient engagement tools, including secure messaging and personalized care plans, integrated directly within our platform.
Security & compliance: HIPAA, ONC Certification, audit trails
Maintaining the security and privacy of patient data is paramount. Integrated systems must adhere to stringent regulations:
- HIPAA compliance: Implementing technical and administrative safeguards to protect Protected Health Information (PHI) as mandated by the Health Insurance Portability and Accountability Act.
- ONC health IT certification: Ensuring that the EHR and other health IT systems meet the standards and criteria set by the Office of the National Coordinator for Health Information Technology.
- Audit trails: Maintaining detailed logs of system access and data modifications to ensure accountability and facilitate compliance audits.
How integrated systems solve real-world coordination challenges
Integrated systems directly address many of the pain points in traditional care coordination:
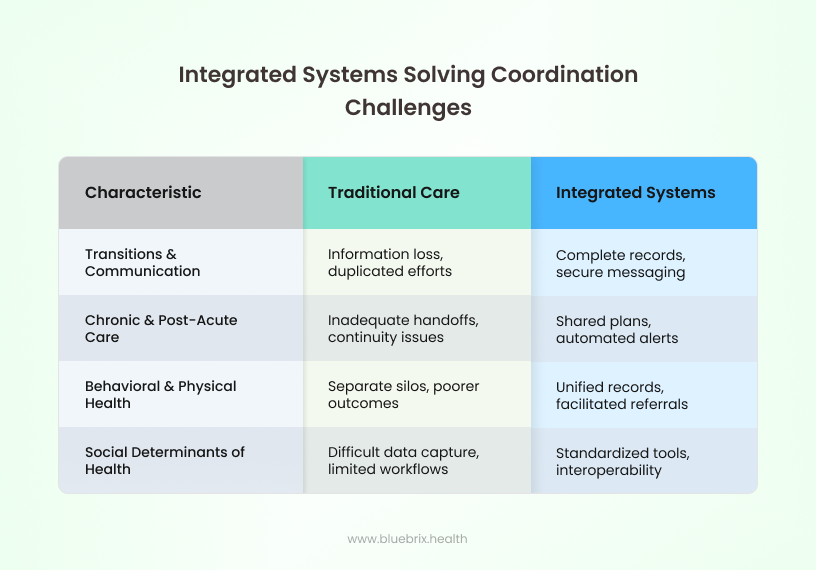
Poor transitions of care and fragmented communications
- Challenge: When patients move between different care settings (e.g., hospital to home, primary care to specialist), critical information can be lost or delayed, leading to errors and increased risk of adverse events. Fragmented communication among providers results in duplicated efforts and a lack of a unified care plan.
- Solution: Integrated EHRs ensure that a patient’s complete medical history and care plan are readily available to all authorized providers involved in the transition. Secure messaging and shared care plans facilitate seamless communication and handoffs. For example, discharge summaries, medication lists, and follow-up instructions can be electronically transmitted to the receiving provider in real-time.
Inadequate handoffs in chronic disease and post-acute care
- Challenge: Managing chronic conditions requires ongoing coordination among multiple specialists, primary care physicians, and other healthcare professionals. In post-acute care settings, ensuring continuity of care and preventing readmissions requires effective communication and information sharing. The cited PubMed Central article (if accessible) likely discusses the complexities and risks associated with inadequate handoffs in these settings.
- Solution: Integrated systems enable the creation of comprehensive, shared care plans that are accessible to all members of the patient’s care team. Automated alerts for follow-up appointments, medication refills, and potential complications help ensure proactive management. For post-acute care, integrated systems facilitate the timely sharing of discharge summaries, rehabilitation plans, and progress notes with the patient’s primary care physician and other relevant providers.
Behavioral and physical health silos
- Challenge: Historically, behavioral and physical healthcare have often operated in separate silos, hindering a holistic approach to patient well-being. This lack of integration can lead to poorer outcomes and increased costs, as mental and physical health conditions often influence each other.
- Solution: Integrated EHRs that can capture and share both behavioral and physical health information in a unified record are crucial. This allows providers to have a more complete understanding of the patient’s needs and to coordinate care that addresses both aspects of their health. Integrated systems can also facilitate referrals and communication between behavioral health specialists and primary care providers.
Social determinants of health (SDoH) data inclusion
- Challenge: Factors like socioeconomic status, education, access to healthy food, and housing can significantly impact a patient’s health outcomes. Traditionally, this data has been difficult to capture and integrate into clinical workflows.
- Solution: Integrated systems are evolving to incorporate SDoH data through standardized data collection tools and interoperability with community-based organizations. This allows providers to identify and address patients’ social needs as part of their overall care plan, leading to more effective and equitable care. blueBriX recognizes the importance of SDoH and is actively working to integrate relevant data points into our platform to provide a more comprehensive view of patient needs.
blueBriX's approach to integrated care
At blueBriX, we understand that truly effective care coordination hinges on a seamlessly integrated technology ecosystem. Our approach is built on decades of experience in value-based care, focusing on solutions that are not just technologically advanced but also deeply aligned with the practical needs of healthcare providers and the well-being of their patients.
Our technology solutions
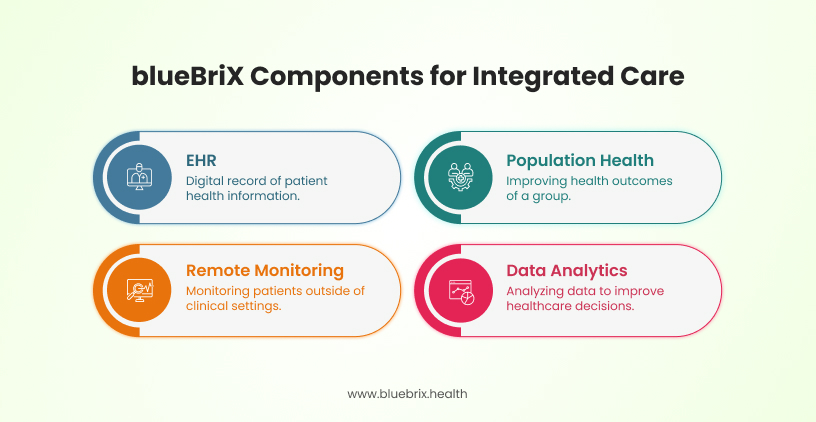
We offer a suite of integrated solutions designed to address the multifaceted challenges of care coordination in value-based care:
- Electronic health records (EHR): Our EHR system serves as the central hub for all patient information, providing a unified and comprehensive view of the patient’s health journey. It’s designed for intuitive use, facilitating efficient documentation, order entry, and secure communication among care team members. The blueBriX integrated EHR is built with interoperability in mind, ensuring seamless data exchange with other systems.
- Population health management: Our platform enables proactive management of patient populations, identifying at-risk individuals, tracking key metrics, and facilitating targeted interventions. It integrates data from various sources to provide actionable insights for improving population health outcomes and managing costs effectively.
- Remote patient monitoring (RPM): Our RPM solutions allow providers to monitor patients’ health remotely, enabling early detection of potential issues and timely interventions. This is particularly valuable for managing chronic conditions and supporting patients in post-acute care settings, enhancing patient engagement and reducing the need for in-person visits.
- Advanced data analytics: Our analytics tools empower healthcare organizations to derive meaningful insights from their data. This includes predictive modeling for risk stratification, performance reporting on quality metrics, and identification of opportunities for process improvement. blueBriX’s advanced analytics capabilities provide the data-driven insights necessary for effective care coordination and value-based performance.
Case studies and success stories
While our technology provides the foundation, it’s the real-world impact that truly matters. Here are a couple of examples of how blueBriX’s integrated systems have helped organizations achieve their care coordination and value-based care goals:
- Improved patient outcomes: A large multi-specialty clinic implemented blueBriX’s integrated EHR and population health management tools. By having a unified view of patient data and leveraging risk stratification, they were able to proactively identify patients with poorly controlled diabetes. Through targeted outreach, personalized care plans, and remote monitoring, they saw a significant improvement in HbA1c levels across their diabetic patient population and a reduction in diabetes-related hospitalizations.
- Enhanced operational efficiency: A network of skilled nursing facilities adopted blueBriX’s integrated EHR and referral management system. This streamlined the process of receiving patient referrals from hospitals, ensuring all necessary patient information was available from the outset. Automated workflows for care planning and communication among the facility’s care team led to more efficient care delivery, reduced administrative burden, and improved staff satisfaction.
Key features of blueBriX's integrated systems
Our integrated systems are packed with features designed to empower effective care coordination:
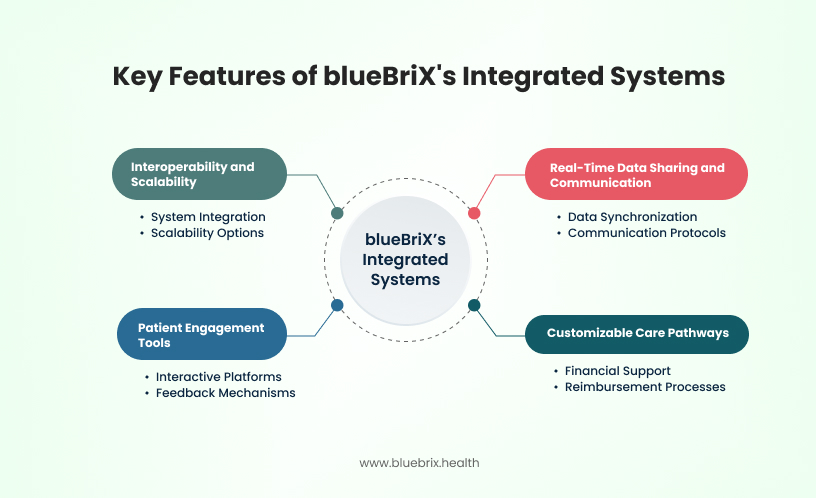
Interoperability and scalability
Our platform is built on open standards and APIs, ensuring seamless interoperability with other healthcare systems, regardless of the vendor. This allows for a holistic view of patient data across the care continuum. Furthermore, our solutions are designed to be highly scalable, adapting to the growing needs of healthcare organizations of all sizes.
Real-time data sharing and communication
blueBriX’s systems facilitate the real-time sharing of critical patient information among authorized care team members. Secure messaging, alerts, and notifications ensure that everyone is on the same page, enabling timely and coordinated responses to patient needs.
Customizable care pathways
We understand that different patient populations and conditions require tailored approaches. Our platform allows for the creation and implementation of customizable care pathways, ensuring that patients receive evidence-based and personalized care that aligns with best practices.
Patient engagement tools
Our integrated patient portal and mobile applications empower patients to actively participate in their care. Features like secure messaging with their care team, access to their health records, appointment scheduling, medication reminders, and educational resources enhance patient engagement and adherence to care plans. blueBriX’s commitment to patient engagement is evident in the intuitive and comprehensive tools integrated into our platform.
Driving value-based care outcomes through coordination
The ultimate goal of effective care coordination, enabled by integrated systems like blueBriX, is to drive positive outcomes in value-based care models:
Aligning care delivery with outcomes
Integrated systems provide the data and tools necessary to align care delivery with desired outcomes. By tracking patient progress against specific goals and quality metrics, providers can adjust care plans in real-time to optimize results.
Cost savings from avoided duplication and unnecessary utilization
Seamless information sharing and coordinated workflows minimize duplicated tests, procedures, and unnecessary hospitalizations or emergency room visits. This leads to significant cost savings for healthcare organizations operating under value-based payment models.
Provider satisfaction and reduced burnout
When systems are integrated and workflows are streamlined, providers experience less administrative burden, improved communication, and a greater sense of control over patient care. This can lead to increased job satisfaction and a reduction in burnout, which is a critical concern in today’s healthcare environment.
Enhancing patient satisfaction and engagement
Patients who experience well-coordinated care feel more supported, informed, and involved in their healthcare journey. This translates to higher patient satisfaction scores and improved engagement in their own health management.
Quality metrics improved by integrated systems: HEDIS, MIPS, PROMs
Integrated systems are instrumental in improving performance on key quality metrics that are central to value-based care reimbursement models:
- Healthcare effectiveness data and information set (HEDIS): These are a set of standardized performance measures used by health plans and other organizations to assess the quality of care and service they provide. Integrated systems facilitate the collection and reporting of HEDIS data.
- Merit-based incentive payment system (MIPS): A track within the Quality Payment Program (QPP) that assesses eligible clinicians based on quality, cost, improvement activities, and promoting interoperability. Integrated EHRs are crucial for meeting the interoperability requirements and tracking performance on quality measures.
- Patient-reported outcome measures (PROMs): These are standardized questionnaires completed by patients to assess their health status, functional capacity, and quality of life from their own perspective. Integrated systems can facilitate the collection and analysis of PROMs data, providing valuable insights into the impact of care.
Future outlook: AI, automation & next-gen interoperability
The evolution of integrated healthcare systems is far from over. The future holds exciting possibilities with the integration of artificial intelligence (AI), automation, and next-generation interoperability standards:
- Predictive and prescriptive analytics: AI-powered analytics will move beyond identifying past trends to predicting future outcomes and suggesting the best course of action. This could include predicting which patients are at highest risk of readmission or identifying the most effective treatment pathways for specific conditions.
- Automated care gap alerts and next-best action engines: AI can also automate the identification of care gaps (e.g., missed screenings, overdue vaccinations) and suggest the “next best action” for providers to take to ensure comprehensive and timely care.
- Patient-directed health data exchange (TEFCA readiness): The Trusted Exchange Framework and Common Agreement (TEFCA) aims to establish a national infrastructure for secure and seamless exchange of electronic health information. Future integrated systems will need to be TEFCA-ready, empowering patients with greater control over their health data and facilitating interoperability on a national scale.
- Integrating wearables, RPM, and smart devices for continuous care: The increasing use of wearables, remote patient monitoring devices, and smart home technologies will generate a wealth of real-time patient data. Future integrated systems will need to seamlessly incorporate this data, enabling continuous monitoring and proactive interventions, moving towards a truly connected and preventative healthcare model.