Picture this: A bustling emergency room. A patient arrives with chest pain, but their symptoms are ambiguous. The attending physician reviews the medical history, but it offers limited clues. Time is of the essence and that’s where data analytics steps in as a powerful tool. It would help to know if the same symptoms or similar conditions were reported earlier to understand any relevant pattern. By analyzing vast amounts of anonymized patient data sharing a similar demographics, the system can identify patterns and correlations potentially arriving at a more accurate diagnosis, saving time and the patient’s life.
Data analytics in healthcare isn’t about flashy theatrics; it’s about harnessing the power of information to improve decision-making at the critical moments, when it matters most. It’s about leveraging the collective experience of countless patients to guide care for the one in front of you, ultimately transforming a hospital or clinic from a reactive environment to a data-driven center of informed intervention.
Healthcare generates a massive volume of data, from patient records, medical journals, prescriptions, books and every piece of information that matters to financial and operational details. This data is a goldmine of insights when harnessed effectively. Data analytics transforms this raw information into actionable knowledge, empowering healthcare providers to make informed decisions, predict health risks, and optimize resource allocation. It’s not just about numbers; it’s about improving patient outcomes and driving efficiency. As the healthcare industry shifts towards value-based care, data analytics becomes even more critical in measuring performance and delivering better value.
Understanding healthcare data analytics
The data analytics lifecycle
Data is the lifeblood of value-based care (VBC). To thrive in this model, healthcare organizations must transform data into actionable insights.
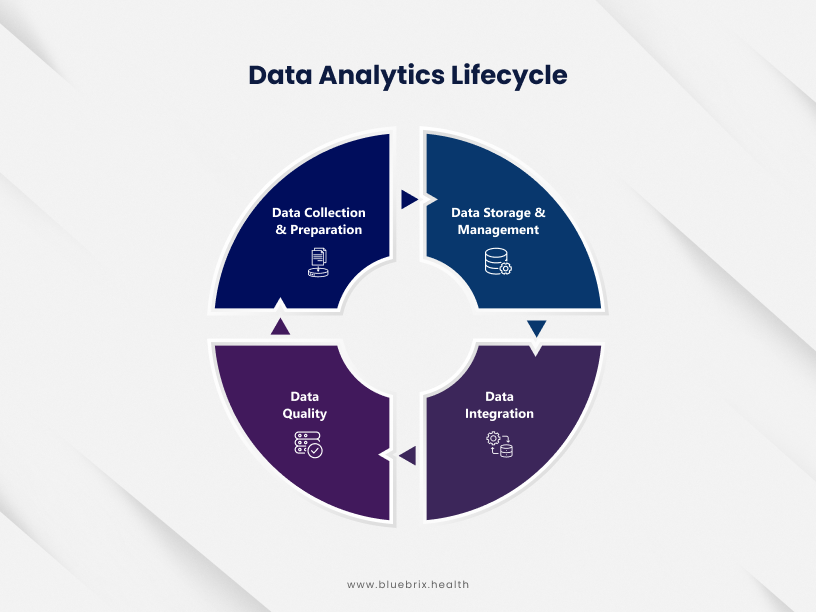
The foundation
- Data collection and preparation: Gathering comprehensive data from various sources is essential. Ensuring data quality through cleansing, standardization, and integration is crucial for accurate analysis.
- Data storage and management: Employing data warehouses and data lakes to store and manage vast datasets including patient’s medical history, demographics, medical records, clinical notes, images, audio recordings, claims data, financial information etc., efficiently supports analysis and reporting.
- Data integration: Effective data analysis hinges on the quality and accessibility of data. Data integration involves consolidating information from diverse sources, including Electronic Health records, claims data, and patient-generated health data. This process requires meticulous data cleansing, transformation, and standardization to ensure accuracy and consistency. Advanced techniques like data mapping and ETL (Extract, Transform, Load) processes facilitate this integration, creating a unified data foundation for analysis.
- Data quality: Data quality is paramount for deriving accurate and actionable insights. It involves rigorous checks for completeness, accuracy, consistency, and timeliness. Data profiling, validation, and cleansing are critical steps in ensuring data reliability. Implementing data governance practices, including data stewardship and quality metrics, is essential for maintaining data integrity over time.
The process
The analytics process is a critical component of the data analytics lifecycle. It involves transforming raw data into meaningful insights that drive decision-making.
Key stages of the analytics process
1. Data exploration and preparation:
- Understanding data structure, format, and quality.
- Cleaning and preprocessing data to remove inconsistencies and errors.
- Creating relevant data subsets or samples for analysis.
2. Data modeling:
- Selecting appropriate statistical or machine learning techniques.
- Building models to identify patterns and relationships within the data.
- Evaluating model performance and accuracy.
3. Data analysis:
- Applying statistical methods to extract meaningful insights from data.
- Using data visualization techniques such as charts, graphs, interactive dashboards etc. to transform complex data into understandable and actionable insights and communicate findings effectively.
- Identifying trends, patterns, and anomalies.
4. Predictive modeling:
- Building models to forecast future trends and outcomes.
- Evaluating model performance and accuracy.
5. Prescriptive analytics:
- Recommending actions based on insights and predictions.
- Developing strategies to optimize outcomes.
Types of analytics
- Descriptive analytics: Understanding past and current performance through metrics like patient demographics, disease prevalence, and resource utilization.
- Diagnostic analytics: Identifying the root causes of issues by analysing underlying factors and patterns.
- Predictive analytics: Forecasting future trends and outcomes using statistical models and machine learning.
- Prescriptive analytics: Recommending optimal actions based on data-driven insights.
By effectively harnessing data, healthcare organizations can optimize resource allocation, improve patient outcomes, and achieve long-term sustainability under the value-based care model.
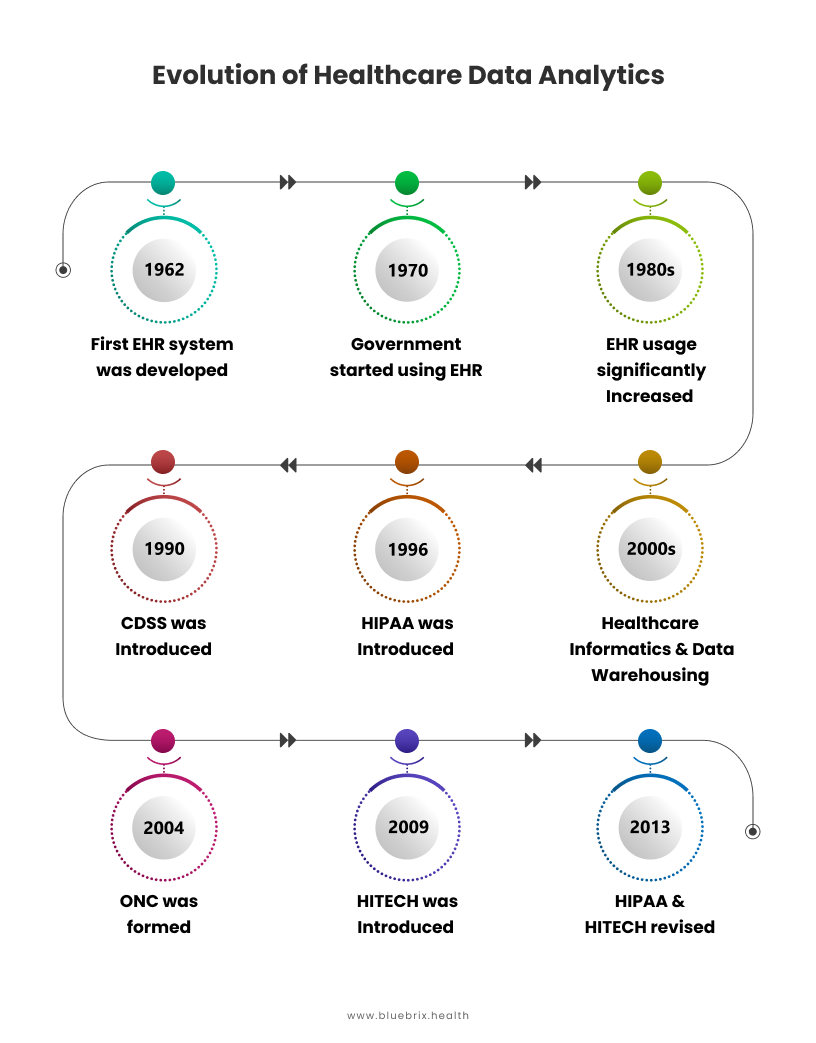
Evolution of healthcare data analytics
Since the inception of Electronic Health Records (EHRs) in the 1960s, healthcare has undergone a digital transformation. What began as simple data storage systems has evolved into a complex ecosystem generating vast amounts of data. Today, data analytics is at the forefront of transforming this data into actionable insights, driving improvements in patient care, operational efficiency, and population health management.
More recent developments:
Advancements in predictive analytics and machine learning
Between 2000 and 2010, rapid technological advancements enabled the adoption of predictive analytics and machine learning in healthcare. These technologies eased the development of predictive models for risk stratification, early disease discovery, and personalized medication.
Big data and real-time analytics
Big Data met healthcare, fuelled by digital health data such as genomic information, wearable detectors, and IoT. Healthcare organizations started to leverage real- time analytics to cover patient health, optimize treatment pathways, and enhance functional efficacy.
Integration of AI and natural language processing (NLP)
AI and NLP became integral to healthcare analytics around the same time. AI algorithms break down complex datasets, help in medical image analysis, automate administrative tasks, and support clinical decision-making.
Telehealth, remote, monitoring, and personalized medicine
Telehealth and remote monitoring have expanded, improving access to care outside traditional settings. Personalized medicine allows healthcare providers to tailor treatments based on individual genetic profiles, marking a significant shift towards more precise and effective patient care strategies.
The current state
Growth in data volume: Approximately 30% of the world’s data comes from healthcare – patient records, claims data, clinical trials, and more. Health data is expected to be 36% of the world’s data in another year. This exponential growth highlights the immense potential of data analytics.
Mergers & acquisitions: There’s a growing trend of healthcare organizations acquiring analytics solution providers that emphasize the importance of data analytics in healthcare. Definitive Healthcare, UnitedHealth Group, TPG Capital, and WellSky are among the few healthcare stalwarts who have acquired technology companies to improve their healthcare delivery.
Tech collaborations: Another interesting trend is healthcare providers collaborating with technology vendors for advanced analytics. Some notable recent collaborations are Google Cloud with Mayo Clinic and Anthem, CVS Health with Microsoft, and Cleveland Clinic with IBM.
The ethical dilemma with AI: Whether to use AI in healthcare, the ethical quandary that persists is yet to be resolved. Although almost 30% of providers are already using AI, and a majority plan to implement it for good, there still exist a significant number of providers that are not convinced of AI usage.
Some interesting statistics worth mentioning are:
A study by McKinsey & Company found that data analytics can potentially generate $100 billion to $450 billion in annual value for the US healthcare system.
A HIMSS Analytics survey revealed that only 23% of healthcare organizations have achieved a high level of data analytics maturity.
How is data analytics adding value to the healthcare ecosystem?
Data analytics is revolutionizing healthcare by unlocking a treasure trove of insights from vast amounts of patient data. This empowers healthcare organizations to move beyond reactive care towards a proactive and data-driven approach. This is particularly relevant in a value-based care model. Here’s how data analytics is creating exciting opportunities:
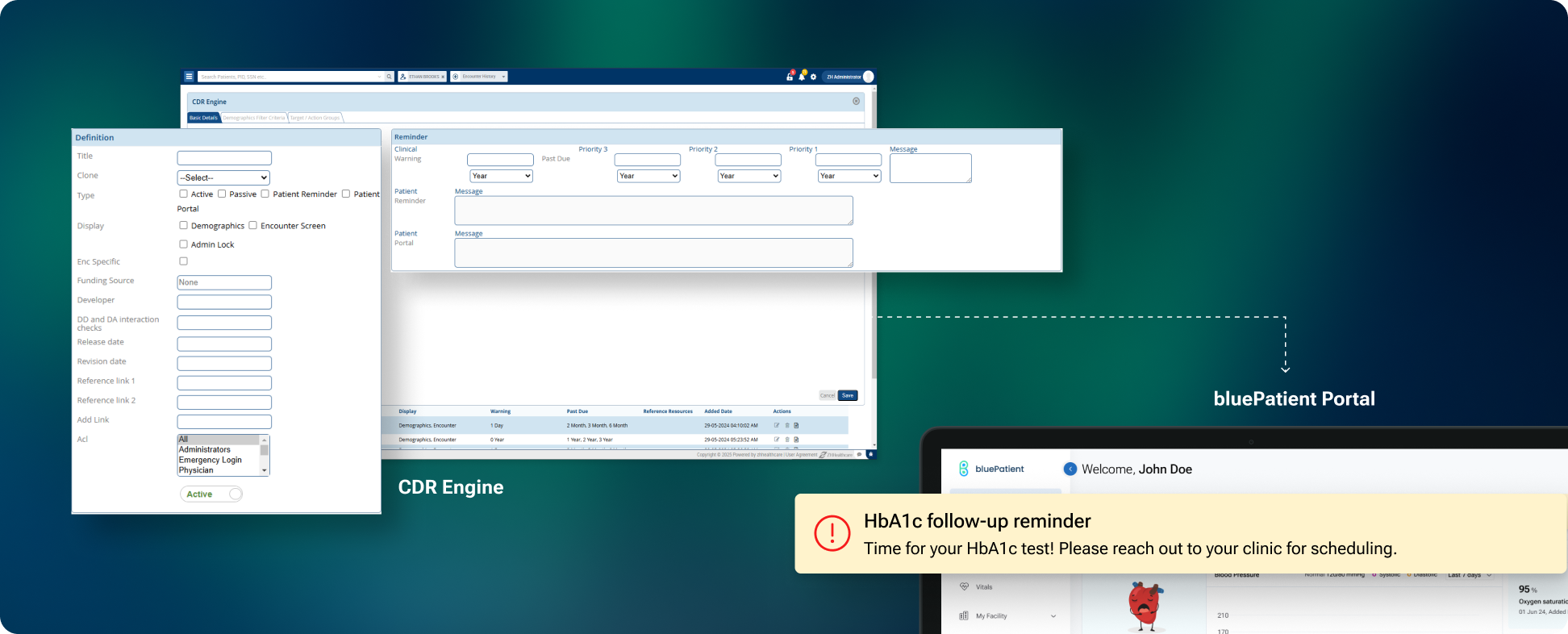
- Clinical decision support system (CDSS): Implementing data analytics in decision support tools enhances clinical decision making. Such systems can process patient data in real time and help healthcare providers make more accurate diagnoses, select the right treatment plans and thus enhance the quality of patient care.
- Healthcare fraud detection: Fraud detection and prevention is a key area where data analytics is useful in identifying any suspicious activity to minimize or prevent fraud cases, thus reducing financial losses while improving compliance with set regulatory requirements.
- Early disease detection and prediction: By analyzing historical data and identifying patterns, data analytics can predict potential health risks in individuals. This allows for early intervention and preventive measures, leading to better patient outcomes and reduced disease burden which directly aligns with value-based care.
- Personalized medicine and prescriptive analytics: Data analytics empowers healthcare to move beyond a one-size-fits-all approach. By analyzing a patient’s medical history, genetics, and lifestyle factors, healthcare professionals can tailor treatment plans and preventative strategies to individual needs which is the key aspect of patient-centered care. Prescriptive analytics can even suggest the most effective medications or treatment options for specific patient profiles.
- Improved population health management: Data analytics enables healthcare organizations to identify at-risk populations within a community. By analyzing trends and social determinants of health (SDoH), interventions can be targeted to address specific population health needs, leading to improved overall health outcomes for the community.
- Clinical risk intervention and predictive analytics: Data analytics can predict potential complications and adverse events before they occur. This allows healthcare professionals to implement preventative measures and improve patient safety. Predictive analytics can also optimize resource allocation by identifying patients at high risk of hospitalization, allowing for focused care management.
- Measuring and managing evidence-based care, care visibility, and waste reduction: Data analytics enables the tracking and measurement of care quality. By analyzing treatment effectiveness and patient outcomes, healthcare organizations can identify areas for improvement and implement evidence-based practices. Additionally, data visibility allows for better care coordination and reduces wasteful practices by identifying areas of inefficiency.
- Efficient report production and improved agility: Data analytics streamlines reporting processes. By automating report generation and providing real-time data insights, healthcare organizations can react quickly to changes and make data-driven decisions with greater agility.
- Prevention of readmissions: By analyzing patient data, healthcare organizations can identify patients at high risk of readmission after discharge. This allows for targeted interventions and care plans to improve patient recovery and reduce hospital readmission rates.
- Better staff management and cost optimization: Data analytics empowers data-driven staffing decisions. By analyzing patient volumes, appointment schedules, and staff performance, healthcare organizations can optimize staffing levels and resource allocation. Additionally, cost analysis through data insights can identify areas for cost reduction and improve overall financial performance.
- Enhanced care coordination: Data analytics fosters better communication and collaboration between healthcare providers. By sharing patient data securely, different healthcare professionals involved in a patient’s care can gain a holistic view and provide more coordinated care.
- Improved patient engagement: Data analytics can be used to develop personalized patient education materials and self-management tools. This empowers patients to take a more active role in their health and adhere to treatment plans more effectively.
- Clinical trial optimization: Data analytics can streamline clinical trial design by identifying potential participants and predicting trial outcomes. This can accelerate research efforts and lead to faster development of new treatments.
- Public health surveillance and outbreak detection: By analyzing real-time data on patient symptoms, emergency room visits, and social media trends, data analytics can help identify potential outbreaks and disease threats faster. This allows for quicker public health interventions and mitigation strategies.
- Value-based care optimization: Data analytics plays a crucial role in value-based care models. By tracking patient outcomes, resource utilization, and cost-effectiveness of care, healthcare organizations can demonstrate the value they deliver and receive appropriate reimbursement under value-based payment structures.
- Drug discovery and development: Data analytics can be used to analyze vast datasets of genetic information, protein structures, and patient outcomes. This can accelerate drug discovery and development by identifying promising drug targets and predicting the effectiveness of potential treatments.
- Benchmarking performance against industry standards and competitors: Data analytics empowers healthcare organizations to benchmark their performance against industry standards and competitors in Value Based Care models. This allows for identifying areas for improvement and implementing best practices to deliver high-quality, cost-effective care.
- Healthcare supply chain optimization: Utilizes data analytics in the optimization of healthcare supply chains for the timely availability of medications, medical devices, and supplies at the lowest cost and optimal utilization to reduce wastage.
- Improve accessibility and optimize delivery: By analyzing remote patient and telehealth data in real-time, healthcare providers can take informed decisions on improving accessibility, increasing physical clinic locations, make the right recommendations for infrastructure improvement etc.
Leveraging data analytics for value-based care
The vast amount of data generated in healthcare presents a goldmine of opportunity. By leveraging data to identify at-risk populations, optimize care delivery, and track performance metrics, healthcare organizations can achieve better patient outcomes and financial sustainability under Value Based Care models. To harness this potential, building a robust data analytics framework is essential. This framework needs to encompass the right KPIs for value-based care success, along with effective data integration and transformation strategies.
Key Performance Indicators (KPIs) for VBC
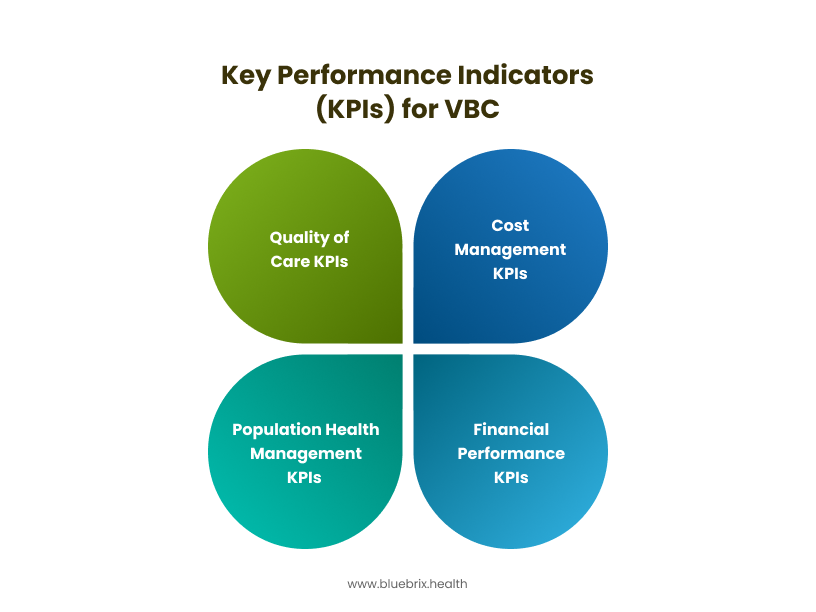
Effective data analytics hinges on identifying and tracking the right metrics. Here’s a breakdown of crucial KPIs for Value Based Care success:
- Quality of care KPIs
- Healthcare effectiveness institute (HEI) measures: These standardized measures assess the effectiveness of care provided for specific conditions. Tracking HEI measures helps ensure evidence-based practices and improve patient outcomes.
- Patient satisfaction scores: Measuring patient satisfaction with care delivery is crucial in Value Based Care models. High patient satisfaction scores can translate to better quality of care ratings and improved financial performance
- Hospital readmission rates: Lower readmission rates indicate better care coordination and improved patient management, leading to positive Value Based Care performance.
- Cost Management KPIs
- Total Cost of Care (TCOC): Tracking TCOC per patient allows healthcare organizations to identify areas of cost inefficiency and optimize resource allocation.
- Return on Investment (ROI): Measuring the ROI of specific interventions helps determine their effectiveness in reducing costs and improving population health outcomes under Value Based Care models
- Resource Utilization Rates: Analyzing resource utilization data for services like lab tests, imaging, and specialist referrals helps identify areas for potential cost reduction.
- Population Health Management KPIs
- Disease Prevalence Rates: Tracking the prevalence of chronic diseases within the patient population allows for targeted interventions and preventive measures to improve population health outcomes.
- Preventive Care Rates: Ensuring high rates of preventive care services like vaccinations and screenings reduces the risk of future complications and lowers overall healthcare costs.
- Health Promotion and Risk Stratification: Identifying at-risk individuals and implementing targeted health promotion programs can improve population health and reduce healthcare costs in the long run.
- Financial Performance KPIs
- Value-Based Modifier (VBM) Scores: VBM scores determine a portion of Medicare reimbursement under Value Based Care models. Tracking VBM scores allows healthcare organizations to monitor their performance and identify areas for improvement.
- Contractual Performance Metrics: Value Based Care contracts often have specific performance metrics tied to financial rewards or penalties. Tracking these metrics ensures compliance and maximizes financial rewards under the Value Based Care contract.
- Risk Adjustment Scores: Risk adjustment scores account for the health complexity of a patient population. Understanding these scores allows healthcare organizations to ensure fair reimbursement under Value Based Care models.
Once the KPIs are set, the next aspect to focus on is how the information is collated, processed and managed. This is where data integration and transformation strategies come into play. These strategies act as the bridge, seamlessly merging data from various sources and transforming it into a unified, high-quality format.
Using Analytics to accelerate the shift to Value-based Care
Value-based care (VBC) represents a fundamental shift in healthcare payment models, focusing on delivering better patient outcomes at a lower cost. The transition from fee-for-service to value-based care requires a data-driven approach. Data analytics plays a pivotal role in optimizing patient outcomes and maximizing financial performance. Let’s look at the core principles of Value Based Care and how data analytics plays a crucial role in achieving them:
- Focus on Patient Outcomes: Value Based Care prioritizes improving patient health outcomes and overall well-being. Data analytics helps by:
- Identifying high-risk patients: Analytics can analyze patient data to identify individuals at risk for developing chronic diseases or complications.
- Monitoring and tracking progress: Data empowers healthcare professionals to monitor patient progress and adjust care plans as needed.
- Measuring quality of care: Analytics helps measure and track key quality metrics, providing valuable feedback on the effectiveness of care delivery.
- Preventive Care and Early Intervention: Value Based Care emphasizes preventive care and early intervention to avoid costly complications. Data analytics plays a critical role by:
- Predicting potential health risks: Advanced analytics can predict future health issues based on patient data, allowing for preventive measures.
- Identifying opportunities for early intervention: By analysing trends and patterns, healthcare providers can identify patients who might benefit from early intervention to prevent complications.
- Optimizing care protocols: Utilizing data can help identify the most effective preventive and treatment strategies, leading to improved clinical outcomes.
- Care Coordination and Collaboration: Value Based Care necessitates collaboration among different healthcare providers to ensure seamless care delivery. Data analytics supports this by:
- Facilitating data sharing: Analytics platforms enable secure data exchange between different healthcare systems, providing a holistic view of patient health.
- Improving communication: Data-driven insights can foster better communication between providers, leading to more coordinated care plans.
- Identifying gaps in care: Analyzing data can identify gaps or inefficiencies in care delivery processes, allowing for coordinated efforts to bridge those gaps.
- Cost Efficiency and Resource Optimization: Value Based Care aims to deliver high-quality care while being more cost-effective. Data analytics contributes to this by:
- Identifying cost drivers: Data can reveal areas where healthcare spending can be optimized, allowing for more efficient resource allocation.
- Reducing waste and redundancy: Analyzing data helps identify and eliminate unnecessary procedures or inefficiencies in resource utilization.
- Promoting evidence-based decision making: Data-driven insights enable better decision-making around resource allocation and treatment options, leading to cost savings.
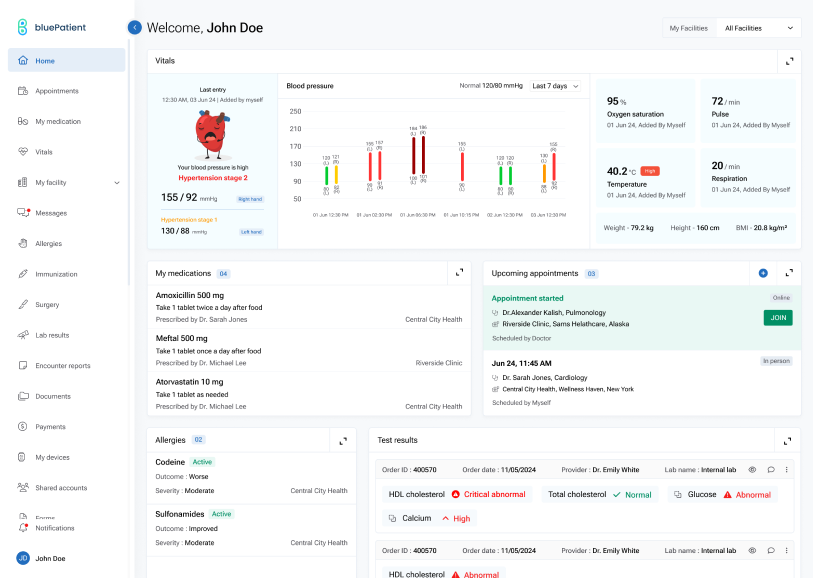
- Patient Engagement: Value Based Care encourages patient engagement in their own health management. Data analytics supports this by:
- Providing patients with access to their own data: Analytics tools can empower patients to track their health information and understand their care plans.
- Facilitating self-management: Data can be used to develop personalized health education resources and support patients in managing chronic conditions.
- Improving patient satisfaction: By putting patients in control of their health data and care plans, data analytics can improve patient satisfaction with the healthcare system.
Enhancing outcomes and patient satisfaction using data analytics
The power of data analytics in Value Based Care extends beyond optimizing cost and performance. It can also be harnessed to create a more patient-centric and personalized care experience which helps improve outcomes and patient satisfaction. This section explores how data analytics empowers healthcare organizations to put patients at the center of their Value Based Care strategy.
Care coordination
Effective care coordination is essential for delivering high-quality, patient-centered care. By leveraging data analytics, healthcare organizations can optimize care transitions, reduce readmissions, and improve communication among care providers.
- Improved patient transitions: Analyze patient data to identify potential gaps in care during transitions between care settings (hospital to home, primary to specialty care).
- Reduced readmissions: Utilize predictive modeling to identify patients at risk of readmission and implement targeted interventions.
- Enhanced communication: Facilitate seamless information sharing among care providers through data integration.
Population health management
Population health management focuses on improving the health outcomes of a defined population. Healthcare organizations can identify at-risk populations, implement targeted interventions, and measure the impact of their efforts using data analytics.
- Risk stratification: Identify high-risk populations for chronic diseases or preventive care interventions.
- Outcome measurement: Track population health metrics to assess the impact of interventions.
- Resource allocation: Optimize resource distribution based on population needs and disease prevalence.
- Patient engagement: Utilize data to tailor communication and education programs for specific patient segments.
Identifying high-risk patients and optimizing care delivery
As discussed previously, data analytics excels at identifying patients at high risk for complications, readmissions, or disease progression. This allows for:
- Stratified care management: Patients can be categorized into risk groups based on their needs, allowing for targeted care management strategies to improve outcomes and optimize resource allocation.
- Chronic disease management programs: Data insights can be used to develop and tailor chronic disease management programs that address specific patient needs and prevent complications.
- Remote patient monitoring: Data from wearable devices and remote monitoring tools can be integrated with analytics to proactively identify health concerns and intervene before complications arise.
Shared decision-making
One of the most crucial aspects of patient-centric care is empowering patients to be active participants in their healthcare decisions. Data analytics can support shared decision-making by:
- Providing patients with personalized data insights: Data can be presented to patients in a clear and understandable format, allowing them to understand their health status and treatment options.
- Decision support tools: Data-driven decision support tools can be developed to empower patients to weigh the risks and benefits of various treatment options and make informed decisions aligned with their preferences.
- Patient-reported outcomes (PROs): Collecting and analyzing PRO data allows healthcare professionals to understand the impact of treatment decisions on a patient’s quality of life, fostering shared decision-making that prioritizes patient values.
Enhancing patient experience
Data analytics can revolutionize patient experiences in several ways:
- Personalized care plans: By analyzing a patient’s medical history, social determinants of health, and lifestyle data, data analytics can inform the development of personalized care plans that address their individual needs and preferences.
- Improved communication and engagement: Data insights can be used to identify patients who may benefit from targeted educational resources or communication strategies, fostering better patient engagement in their own healthcare.
- Proactive outreach and preventive care: Analyzing data on past health trends and risk factors allows for proactive outreach to patients at risk for developing chronic conditions, facilitating early intervention and preventive care measures.
Cost reduction strategies through data-driven insights
While cost-effectiveness is crucial in Value Based Care, achieving it shouldn’t come at the expense of patient care. Data analytics can identify areas for cost reduction while maintaining or improving patient outcomes:
- Identifying and reducing low-value care: Data analytics can help identify unnecessary procedures or tests, allowing for a focus on high-value care that delivers the most benefit to patients.
- Waste reduction and resource optimization: Analyzing resource utilization data allows for identifying areas of waste and streamlining processes to optimize resource allocation.
- Predictive analytics for cost management: Predictive analytics can be used to identify patients at high risk for expensive procedures or hospitalizations, allowing for proactive interventions that may reduce overall healthcare costs.
Enabling the shift from reactive to proactive healthcare
The field of data analytics in healthcare is constantly evolving. This section explores some of the most exciting advancements that hold immense potential to revolutionize healthcare delivery in the Value based Care landscape:
Predictive analytics
Predictive analytics goes beyond simply analyzing past data. It uses advanced algorithms to predict potential health risks, disease progression, and potential complications based on historical and real-time data. Let’s explore how predictive analytics is enabling proactive interventions, personalized care plans, and improved resource allocation:
- Disease risk prediction: By analyzing factors like genetics, lifestyle habits, and family history, predictive analytics can identify individuals at high risk for developing specific diseases like heart disease, diabetes, or even certain cancers. This allows for early intervention and preventive measures.
- Hospital readmission risk stratification: Analyzing patient data can help predict which patients are at high risk for readmission after hospitalization. This allows for targeted interventions, such as medication management programs or transitional care services, to reduce readmission rates.
- Proactive deterioration prediction: Real-time data from wearable devices and electronic health records (EHRs) can be used to predict potential patient deterioration in hospitals or intensive care units. This allows for early intervention and improved patient outcomes.
- Resource allocation and cost management: Predictive analytics can forecast future patient volumes and resource needs, allowing for better staffing schedules, equipment allocation, and bed management in hospitals. This leads to improved operational efficiency and cost management.
- Personalized medicine: Predictive analytics can be used to identify the most effective treatment options for individual patients based on their unique genetic makeup and medical history. This approach to personalized medicine leads to improved treatment efficacy and reduced side effects.
- Public health monitoring: By analyzing disease trends and social determinants of health, predictive analytics can help identify potential outbreaks or public health emergencies. This allows for proactive public health measures and targeted interventions.
- Predictive modeling for population health management: Predictive analytics can be used to identify at-risk populations within a community and target public health interventions to address potential outbreaks or chronic disease trends.
Automation and optimization
Artificial intelligence (AI) and machine learning (ML) are rapidly transforming data analytics in healthcare with automation and process optimization. These powerful tools can analyze vast amounts of complex data, identify hidden patterns, and generate insights that may be overlooked during human analysis. Potential applications include:
- Automated patient risk assessment: AI algorithms can analyze patient data to predict potential complications or hospital readmissions, allowing for proactive interventions.
- Clinical trial design and optimization: ML can be used to identify potential participants for clinical trials based on specific criteria, streamlining the trial process and accelerating drug development.
- Personalized medicine and treatment recommendations: AI can analyze a patient’s medical history, genetics, and lifestyle factors to recommend personalized treatment options with higher potential for success.
Real-time analytics and clinical decision support
Real-time analytics leverages data collected in real-time from various sources, including wearable devices, electronic health records (EHRs), and remote monitoring tools. This allows for:
- Continuous patient monitoring: Healthcare professionals can gain real-time insights into a patient’s health status, allowing for immediate intervention if vital signs deviate from normal ranges.
- Improved point-of-care decision making: Real-time data can be integrated with clinical decision support tools to provide healthcare professionals with evidence-based recommendations at the point of care.
- Enhanced remote patient management: Real-time data from wearable devices can be used to monitor patients remotely, identify potential health concerns early on, and prevent complications.
Beyond traditional specialties
The potential of data analytics in Value Based Care extends far beyond traditional specialties like cardiology or diabetes management. Here’s a glimpse into how data analytics can revolutionize care delivery in various specialties:
- Autism spectrum disorder (ASD): Data from wearable devices tracking activity levels, sleep patterns, and potential triggers can be combined with behavioral observations to personalize interventions and improve patient outcomes.
- Behavioral management: Analyzing data on patient interactions and treatment responses can inform personalized behavior modification plans for conditions like ADHD or eating disorders.
- Mental health: Data analytics can be used to track patient symptoms, medication adherence, and treatment effectiveness. This allows for the development of targeted interventions and early identification of potential mental health crises.
- Pediatric care: Predictive analytics can be used to identify children at high risk for developmental delays or chronic illnesses. Additionally, data from wearable devices can monitor growth and activity patterns, allowing for early intervention and preventive measures.
- Neurology: Analyzing brain scans and other neurological data alongside patient symptoms can improve diagnosis accuracy and inform personalized treatment plans for conditions like epilepsy or Parkinson’s disease.
- Gynecology: Data analytics can be used to identify women at high risk for pregnancy complications, allowing for proactive interventions and improved maternal health outcomes.
- Postpartum care: Data from wearable devices and patient surveys can be used to monitor postpartum depression and anxiety, allowing for early intervention and improved mental health support for new mothers.
- Personalized pain management: Chronic pain management is another area where data analytics holds immense potential. By analyzing data from wearable devices tracking pain intensity, location, and sleep patterns, alongside patient-reported outcomes, healthcare providers can gain valuable insights into a patient’s unique pain experience. This data can be used to develop personalized pain management plans that combine medication, physical therapy, and behavioral interventions tailored to the specific needs of each patient, ultimately leading to improved pain control and quality of life.
- Maternity care and birth outcomes: Data analytics can bridge the gap in rural areas by identifying high-risk pregnancies and facilitating remote monitoring through wearable devices and telehealth consultations. It can also help predict areas with high birth rates, allowing for targeted resource allocation and ensuring adequate staffing and equipment in rural healthcare facilities. Analyzing data on air quality, water pollution, and exposure to environmental toxins can identify potential risks to maternal and fetal health, allowing for targeted interventions and preventive measures. Data analytics can be used to study the impact of climate change on factors like heat stress and pregnancy complications, informing strategies to mitigate these risks.
- Genomic and microbiome integration: Genomic data can be analyzed to identify women at risk for genetic disorders or complications during pregnancy. Data on the maternal microbiome can offer insights into potential risks for pre-eclampsia, preterm birth, and infant development, informing preventative measures and personalized care plans.
With data analytics, healthcare organizations can move beyond traditional Value Based Care models and deliver truly patient-centric care across a wider spectrum of health needs. This comprehensive approach can improve population health outcomes, optimize resource allocation, and ultimately, transform healthcare delivery for the better.
Operational efficiency and cost-effectiveness
Data analytics empowers healthcare organizations to identify inefficiencies, optimize resource allocation, and reduce costs. By analyzing operational data such as appointment scheduling, resource utilization, and supply chain management, providers can streamline processes, reduce waste, and improve overall efficiency.
Key areas of focus include:
- Appointment optimization: Analyzing scheduling patterns to reduce wait times, increase patient satisfaction, and improve resource utilization.
- Supply chain management: Optimizing inventory levels, reducing waste, and ensuring timely supply availability.
- Cost reduction: Identifying areas of cost overruns and implementing strategies to reduce expenses without compromising care quality.
Creating viable value based care contracts with a data and analytics framework
Data analytics plays a crucial role in developing and managing value-based care contracts. By analyzing patient populations, risk profiles, and cost trends, healthcare organizations can accurately assess risk and negotiate favorable contract terms.
Key considerations include:
- Risk adjustment: Utilizing data to accurately assess patient risk and adjust contract payments accordingly.
- Performance measurement: Tracking key performance indicators (KPIs) to measure outcomes and identify areas for improvement.
- Predictive modeling: Forecasting future costs and resource utilization to inform contract negotiations.
- Contract optimization: Analyzing contract performance to identify opportunities for renegotiation or improvement.
Challenges in healthcare data analytics
While data analytics holds immense potential, several challenges hinder its full utilization in healthcare.
Data integration challenges:
Data silos and interoperability: Fragmented healthcare systems often lead to data being stored in disparate sources – electronic health records (EHRs), claims databases, public health records, and social determinants of health (SDOH) data. Integrating and harmonizing data across these silos remains a hurdle. Inconsistent data formats and proprietary systems create technical barriers, hindering comprehensive analysis of a patient’s health journey.
Data quality and standardization: The accuracy of data analytics hinges on the quality of the underlying data. Unfortunately, healthcare data often suffers from inconsistencies, missing information, and errors due to manual entry mistakes or variations in coding practices which could lead to biased decision-making. The lack of standardized data formats across different healthcare systems further complicates analysis and makes it difficult to compare data sets.
Interoperability standards adoption: While standardized data formats for data exchange exist (e.g., HL7 v2/v3, CDA, FHIR, DDI, SDMX, JSON, xml etc.), they’re not yet widely adopted by healthcare systems. This lack of consistent standards continues to impede seamless data exchange and integration for comprehensive analysis.
Legacy infrastructure: Many healthcare organizations rely on legacy IT infrastructure that may not be equipped to handle the demands of big data analytics. Modernizing infrastructure to support data analytics capabilities can be a significant cost factor.
Technical challenges:
Data pipelining & collection: Building robust data pipelines to efficiently collect, clean, and transform raw data into a usable format for analysis requires significant expertise and resources.
Data visualization: Presenting complex data sets in clear and actionable visualizations that healthcare professionals can readily understand remains a challenge.
Infrastructure limitations: Insufficient computing power, storage, and networking capabilities can hinder data analysis.
Data management tools: Selecting and implementing appropriate data management and analytics tools can be complex.
Security challenges:
Data security: Safeguarding patient data is paramount. Healthcare organizations must implement robust security protocols to protect patient data. This includes encryption technologies, access control measures and other measures including physical safety of information.
Cyberattacks: The increasing sophistication of cyber threats makes healthcare organizations vulnerable to data breaches.
Insider threats: The risk of data breaches by employees or contractors cannot be overlooked.
Data encryption: Ensuring data is encrypted both at rest and in transit is crucial for protecting sensitive information.
Regulation and policy concerns:
Data anonymization: Ensuring patient data anonymization while enabling its use for analytics requires careful consideration of ethical and regulatory frameworks.
Big data & data governance: The sheer volume of data generated in healthcare can be overwhelming. Managing and governing this “big data” requires robust data governance strategies to ensure data quality, security, and compliance with regulations. Establishing clear ownership, access controls, and data usage policies is crucial for responsible data analytics practices.
Regulatory landscape: The ever-evolving regulatory environment surrounding data privacy and security can create complexities for healthcare organizations implementing data analytics solutions. Staying up-to-date on compliance requirements and navigating regulations can be burdensome.
Privacy challenges:
Data privacy: Safeguarding patient data is paramount. Healthcare organizations must comply with patient privacy rules stipulated by federal rules. This includes compliance with data privacy regulations like HIPAA (Health Insurance Portability and Accountability Act), GDPR, PCI DSS, CCPA, DPDP, DISHA, HITECH, Telehealth Privacy etc.
Patient buy-in and trust: Building trust with patients regarding data collection and usage for analytics is crucial. Addressing patient concerns about data privacy and ensuring transparency about how their data is used is essential for successful data analytics initiatives.
Talent and expertise:
Data literacy: Many healthcare providers lack the training and expertise to fully understand and utilize data analytics effectively. Bridging this data literacy gap is crucial for healthcare professionals to leverage data insights for informed decision-making.
Limited analytical expertise: While data literacy is a broad concern, the lack of qualified data scientists and analysts specifically trained in healthcare data is a significant challenge. This expertise gap can limit the ability of healthcare organizations to translate raw data into actionable insights.
Budgetary constraints:
Cost: Implementing and maintaining a data analytics infrastructure requires significant investment.
Budget: Limited budgets, particularly for smaller healthcare organizations, can hinder their ability to fully capitalize on data analytics.
Return on investment (ROI): Demonstrating the value of data analytics and justifying expenditures can be challenging.
Biases:
Data collection bias: If data is primarily collected from a specific population, it may not represent the entire patient population.
Algorithmic bias: Algorithms trained on biased data can perpetuate disparities.
Implicit bias: Human biases can inadvertently influence data collection and analysis.
Lack of diversity in data: Limited representation of certain populations in datasets can lead to biased models.
Navigating the data-driven healthcare landscape
The landscape of data analytics in healthcare is constantly evolving, presenting exciting possibilities for the future of Value Based Care. This section explores how healthcare providers can stay ahead of the curve using data analytics.
Healthcare sustainability
Balancing the need to deliver high-quality care with the pressure to control costs is a major challenge to sustain in healthcare. Value-based care (VBC) models present a promising solution, focusing on delivering better outcomes at lower costs. However, achieving Value Based Care success requires a fundamental shift towards data-driven decision making. Here, data analytics emerges as a powerful tool for building a sustainable future for healthcare. Let’s explore how data analytics lead to sustainability in healthcare:
- Optimizing resource allocation and cost management
- Data analytics can identify areas of waste and inefficiency in healthcare delivery.
- By analyzing resource utilization data, healthcare organizations can optimize staffing levels, equipment allocation, and service delivery processes, leading to cost savings.
- Predictive analytics can help anticipate potential high-cost cases, allowing for proactive interventions and preventative measures to reduce overall healthcare expenditures.
- Improving population health management
- Data analytics empowers healthcare organizations to identify at-risk populations within a community.
- This data can be used to develop targeted public health initiatives and preventive care programs, focusing on areas with the highest disease burden and potential for cost reduction.
- By focusing on preventive measures and early intervention, data analytics can help reduce the prevalence of chronic diseases and associated healthcare costs in the long run.
- Enhancing quality of care and patient outcomes
- Data analytics allows for continuous monitoring and evaluation of healthcare quality metrics.
- By identifying areas for improvement in care delivery processes, healthcare organizations can implement targeted interventions to enhance quality and patient outcomes.
- Real-time data from wearable devices and remote monitoring tools can be used to identify potential health concerns early on, leading to timely interventions and improved patient outcomes, reducing the need for costly hospitalizations.
- Promoting value-based care models
- Data analytics plays a crucial role in demonstrating the value delivered under Value Based Care models.
- By analyzing data on cost savings, improved patient outcomes, and resource utilization, healthcare organizations can effectively showcase the benefits of Value Based Care to payers and policymakers.
- Data-driven insights can also inform the development of more effective Value Based Care payment models, ensuring fair compensation for delivering high-quality, cost-effective care.
Building a data-driven culture
The successful implementation of data analytics goes beyond technology and tools. To build a sustainable future for healthcare, a data-driven culture is essential. This involves:
- Investing in workforce development: Healthcare organizations need to invest in training and development programs to equip staff with data analysis skills and the ability to translate data insights into actionable strategies.
- Fostering collaboration: Breaking down silos between departments and fostering collaboration between clinicians, data analysts, and administrators is crucial for leveraging data effectively.
- Promoting data literacy: Educating patients about the importance of data and fostering trust in data collection and usage practices is key to building a sustainable data-driven healthcare ecosystem.
With a data-driven culture, healthcare organizations can unlock a future of value-based care that prioritizes both cost-effectiveness and quality care. This approach can contribute to a more sustainable healthcare system, improve population health outcomes, and ultimately, pave the way for a healthier future for all.
Generative AI in data analytics
Generative AI has immense opportunities in healthcare data analytics. It can be used for automating tasks, uncovering hidden patterns, and accelerating insights. It can process vast amounts of data, generating new data points or completing tasks previously done by humans.
Key applications include:
1. Extracting information from images and videos
- Medical image analysis: AI algorithms can analyze medical images like X-rays, MRIs, and CT scans to detect abnormalities and assist in diagnosis.
- Video analysis: Analyzing surgical videos to improve surgical techniques and outcomes.
2. Medical diagnosis and treatment plans
- Disease prediction: Identifying patients at risk for specific diseases based on medical history, lifestyle, and genetic data.
- Treatment recommendations: Suggesting optimal treatment plans based on patient-specific factors and clinical guidelines.
3. Medical imaging analysis
- Image segmentation: Identifying and isolating specific regions of interest in medical images.
- Object detection: Locating and classifying objects within medical images.
- Image reconstruction: Creating 3D models from 2D images for better visualization.
4. Remote patient assistance
- Virtual assistants: Providing patient support, answering questions, and scheduling appointments.

- Remote monitoring: Tracking patient vital signs and detecting anomalies for early intervention.
- Telemedicine: Enabling virtual consultations between patients and healthcare providers.
5. Virtual assistants and chatbots
- Patient engagement: Providing information, answering questions, and offering support.
- Administrative tasks: Scheduling appointments, handling billing inquiries, and providing appointment reminders.
- Clinical decision support: Assisting healthcare providers in making informed decisions.
6. Creating interactive dashboards and reports
- Data visualization: Presenting complex data in a clear and understandable format.
- Performance monitoring: Tracking key performance indicators (KPIs) to measure the effectiveness of care delivery.
- Predictive analytics: Visualizing future trends and outcomes based on data analysis.
7. Drug discovery
- Molecular modeling: Simulating molecular interactions to identify potential drug candidates.
- Drug repurposing: Identifying new uses for existing drugs.
- Clinical trial optimization: Predicting patient outcomes and optimizing trial design.
8. Personalized medicine
- Precision medicine: Tailoring treatment plans based on individual patient characteristics.
- Genomic analysis: Analyzing genetic information to identify personalized treatment options.
- Patient risk assessment: Predicting disease risk based on patient data.

While challenges like data privacy and model bias exist, the potential benefits of generative AI in healthcare data analytics are immense. It promises to enhance efficiency, accuracy, and the overall value derived from data.
Healthcare AI agents
AI agents are advanced software systems that leverage artificial intelligence to perform tasks traditionally done by humans. In healthcare, they are revolutionizing how care is delivered, managed, and experienced.
Key roles of AI agents in healthcare:
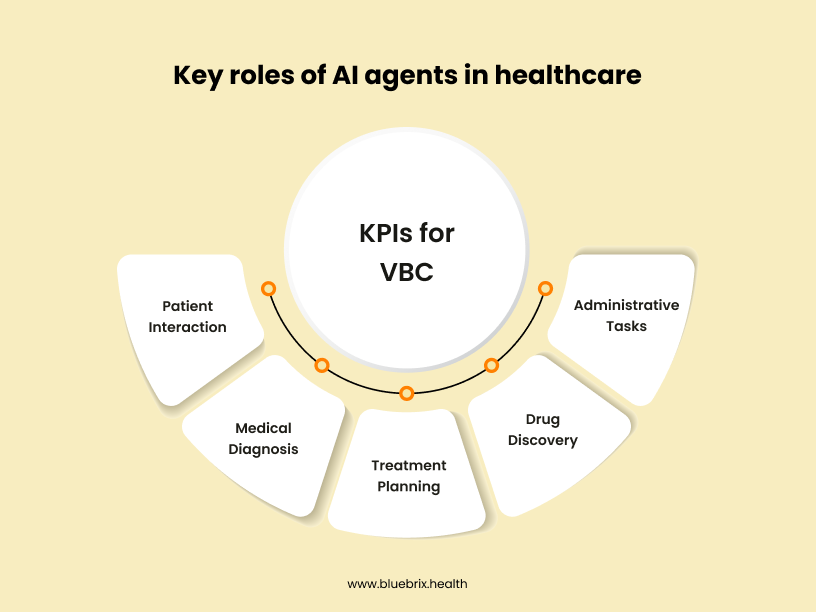
- Patient interaction: Acting as virtual assistants, answering patient inquiries, scheduling appointments, and providing health information.
- Medical diagnosis: Assisting doctors in diagnosing diseases by analysing patient data, medical history, and symptoms.
- Treatment planning: Creating personalized treatment plans based on patient-specific data and clinical guidelines.
- Drug discovery: Accelerating drug discovery by analysing vast amounts of data to identify potential drug candidates.
- Administrative tasks: Automating routine tasks like medical record management and insurance claims processing.
Benefits of AI agents in healthcare:
- Improved patient experience
- Enhanced diagnostic accuracy
- Increased efficiency and productivity
- Reduced costs
- Expanded access to care
While AI agents hold immense potential, challenges such as data privacy, algorithm bias, and regulatory compliance need to be addressed for their widespread adoption.
Anticipated breakthroughs
- Integration of social determinants of health (SDOH) and wearable device data: The seamless integration of SDOH data like social factors and economic determinants with clinical data and information from wearable devices will enable a more holistic understanding of patient health and inform targeted interventions.
- Advanced analytics and artificial intelligence (AI): The continued advancement of AI and machine learning will lead to more sophisticated analytics capabilities. AI could be used for tasks like:
-
- Automated risk stratification: AI algorithms will become even more adept at identifying patients at high risk for specific conditions, allowing for preventive measures and personalized care plans.
- Real-time disease detection and prediction: AI-powered analytics may enable real-time detection of potential health issues based on continuous data streams, allowing for immediate intervention.
- Natural language processing (NLP) for unstructured data analysis: NLP advancements will unlock the potential of analyzing unstructured data like physician notes and patient narratives, providing deeper insights into patient care.
- Interoperability and standardization: The healthcare industry is moving towards greater interoperability of data systems and standardized data formats. This will facilitate seamless data exchange and improve the efficiency of data-driven decision making.
- Focus on interoperability and data sharing: Increased collaboration between healthcare providers, payers, and public health agencies will lead to more comprehensive data sets and facilitate the development of population health management strategies.
- The rise of explainable AI (XAI): As AI plays a larger role in healthcare, ensuring transparency and explainability of AI models’ decision-making processes will be crucial for building trust with patients and healthcare professionals.
- Social media and data analytics: Social media data (when anonymized and ethically collected) can offer insights into social determinants of health like access to healthy food or transportation, impacting mothers and babies in rural areas. Social media platforms can be leveraged for targeted outreach programs and educational resources to promote healthy pregnancy practices in rural communities.