Healthcare providers are at a crossroads as they transition from volume-driven care to value-based care (VBC). Key metrics such as patient outcomes, cost reduction, satisfaction scores, physician burnout, care coordination, and preventive care could be crucial in driving value-based care. This article dives into these critical metrics, offering practical insights for improvement and exploring how blueBriX’s tailored digital health solutions empower providers to excel in VBC. From reducing administrative burdens to enhancing patient engagement, discover actionable strategies to thrive in a value-driven healthcare landscape.
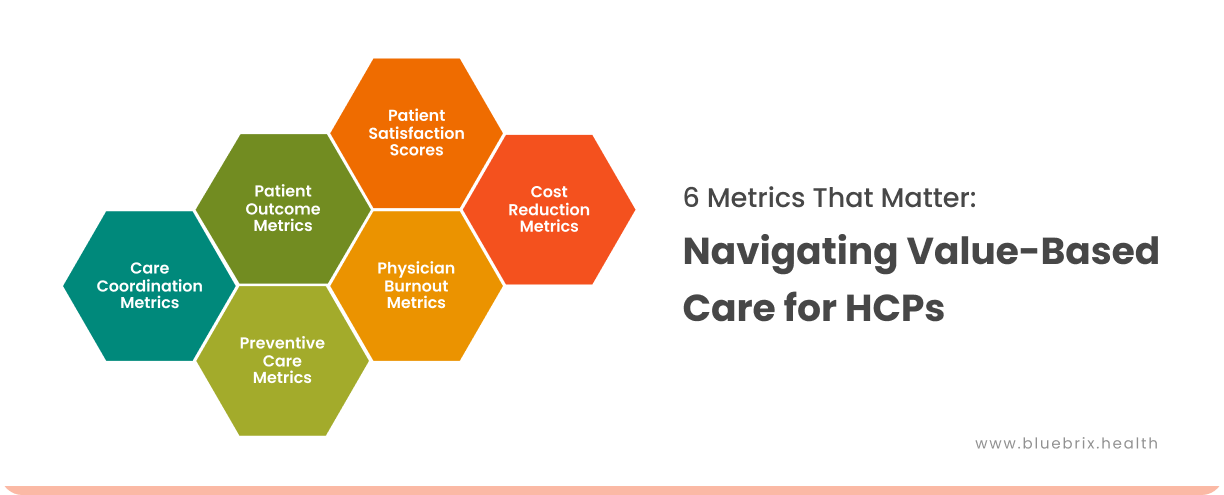
Transitioning to value-based care represents a significant shift for healthcare providers (HCPs), requiring a reorientation from volume-driven metrics to those focused-on value, outcomes, and patient satisfaction. Success in this model depends on identifying and tracking the right metrics—ones that optimize health outcomes, reduce costs, and enhance satisfaction for both patients and providers. Importantly, addressing metrics tied to physician burnout is crucial for sustainable VBC implementation. Here are the key metrics every provider should prioritize, along with practical insights for improvement.
1. Patient Outcome Metrics
Definition: These metrics measure the effectiveness of care in improving patient health outcomes, including recovery rates, chronic disease management, and mortality rates.
Examples:
- Readmission Rates: Tracks the percentage of patients who are readmitted to a hospital within 30 days of discharge.
- Chronic Disease Control: Metrics like HbA1c levels for diabetes or blood pressure management for hypertension.
How It’s Calculated:
- Readmission Rate = (Number of Readmitted Patients / Total Discharged Patients) × 100
Challenges:
- Inconsistent patient adherence to treatment plans.
- Social determinants of health (SDOH) impacting outcomes.
Tips to Improve:
- Leverage patient engagement tools like reminders for follow-ups or medication adherence.
- Integrate SDOH data into care planning.
- Utilize care management platforms like blueBriX to personalize interventions.
2. Cost Reduction Metrics
Definition: Focuses on minimizing unnecessary spending while maintaining high-quality care.
Examples:
- Cost Per Episode of Care: Measures total costs associated with treating a specific condition or performing a procedure.
- Avoidable Emergency Department (ED) Visits: Tracks ED visits for non-urgent issues.
How It’s Calculated:
- Cost Per Episode = Total Cost of Care / Number of Cases
- Avoidable ED Visits = (Avoidable ED Visits / Total ED Visits) × 100
Challenges:
- Difficulty in identifying and addressing inefficiencies within workflows.
- Patient education gaps about appropriate care settings.
Tips to Improve:
- Make the patients aware of alternatives such as telehealth, video consulting, urgent care etc.
- Implement predictive analytics to flag high-cost cases early.
- Adopt cost analytics tools from platforms like blueBriX to monitor and adjust spending patterns.
3. Patient Satisfaction Scores
Definition: Reflects the patient’s experience and perceived quality of care.
Examples:
- Net Promoter Score (NPS): Measures the likelihood of a patient recommending the provider.
- CAHPS Surveys: Comprehensive surveys designed to capture patient experiences across various aspects of care delivery, such as communication, access to care, and provider responsiveness.
- Patient-Reported Outcome Measures (PROMs): Focuses on patient-reported data regarding their health status and quality of life.
- Real-Time Feedback Tools: Digital tools that collect immediate feedback from patients after appointments or interactions.
How It’s Calculated:
- NPS = % Promoters – % Detractors
Challenges:
- Misalignment between patient expectations and clinical realities.
- Extended wait times or insufficient communication.
- Difficulty integrating real-time feedback into workflows.
Tips to Improve:
- Use patient feedback tools to gather actionable insights.
- Simplify communication through patient-friendly portals.
- Train the staff to improve patient interactions.
- Leverage real-time feedback tools to address concerns promptly.
4. Physician Burnout Metrics
Definition: Measures the extent to which providers experience stress, fatigue, or dissatisfaction in their roles.
Examples:
- Work-Life Balance Score: Self-reported score by physicians on their perceived balance.
- Administrative Burden Hours: Tracks the amount of time spent on non-clinical tasks.
How It’s Calculated:
- Work-Life Balance = (Satisfied Physicians / Total Physicians) × 100
Challenges:
- Excessive documentation requirements.
- Misalignment between clinical work and administrative tasks.
Tips to Improve:
- Introduce automation tools for administrative tasks.
- Implement EHR systems with streamlined workflows.
- Foster a culture of feedback and support to address burnout proactively.
5. Care Coordination Metrics
Definition: Tracks the efficiency of communication and collaboration across care teams and settings.
Examples:
- Referral Completion Rates: Measures the percentage of referred patients who follow through with specialist visits.
- Care Plan Adherence Rates: Tracks the extent to which care plans are implemented as designed.
How It’s Calculated:
- Referral Completion = (Completed Referrals / Total Referrals) × 100
- Care Plan Adherence Rate = (Number of patients who adhered to the care plan /Total number of patients with a prescribed care plan) × 100
Challenges:
- Gaps in communication between primary care providers and specialists.
- Lack of integrated care management systems.
Tips to Improve:
- Use centralized communication platforms to track referrals and care plans.
- Leverage blueBriX’s care coordination tools to enhance collaboration.
6. Preventive Care Metrics
Definition: Measures the effectiveness of proactive interventions to avoid chronic diseases or complications.
Examples:
- Vaccination Rates: Percentage of eligible patients who received recommended vaccines.
- Screening Adherence Rates: Tracks adherence to preventive screenings like mammograms or colonoscopies.
How It’s Calculated:
- Screening Adherence = (Patients Screened / Eligible Patients) × 100
Challenges:
- Patient hesitancy or lack of awareness.
- Resource constraints in reaching underserved populations.
Tips to Improve:
- Deploy targeted education campaigns using patient engagement platforms.
- Offer convenient scheduling options like mobile screenings or telehealth.
- Monitor progress with population health management tools.
How can blueBriX help HCPs improve these metrics?
As healthcare organizations transition to value-based care, the healthcare providers (HCPs) need to track and optimize specific metrics as given above that directly impact patient outcomes, costs, satisfaction, and provider well-being. blueBriX offers tailored digital health solutions to address these needs, enabling providers to meet the demands of VBC while streamlining operations and improving care delivery. Below is a detailed look at how blueBriX supports HCPs in achieving excellence across critical metrics.
Patient Outcome Metrics
blueBriX empowers HCPs to improve patient outcomes by leveraging advanced analytics, care management tools, and patient engagement solutions.
- Predictive Analytics: blueBriX uses AI-driven analytics to identify at-risk patients and forecast potential complications, enabling early interventions.
- Personalized Care Plans: Through its care management platform, blueBriX allows providers to create tailored care plans based on patient data, ensuring more effective treatments.
- Remote Patient Monitoring (RPM): blueBriX integrates wearable devices and telehealth solutions to monitor patient health in real time, enabling timely responses to deteriorating conditions.
- Education and Engagement: The platform provides educational resources and tools to help patients understand their conditions and adhere to treatment plans.
Impact: Improved HbA1c levels in diabetic patients achieved through personalized care plans and continuous monitoring, reducing complications.
Cost Reduction Metrics
blueBriX helps providers reduce costs by minimizing inefficiencies and targeting high-cost areas through data-driven value-based care solutions.
- Cost Analytics: The platform provides detailed insights into spending patterns, identifying areas where costs can be reduced without compromising care quality.
- Avoidable ED Visit Prevention: blueBriX’s telehealth tools and predictive modeling help guide patients to appropriate care settings, reducing unnecessary emergency department visits
- Resource Optimization: By streamlining workflows and automating administrative tasks, blueBriX ensures that resources are used efficiently.
Impact: Reduction in avoidable hospital readmissions through predictive analytics and targeted interventions.
Patient Satisfaction Scores
blueBriX enhances the patient experience through its comprehensive engagement tools, leading to improved satisfaction scores.
- Real-Time Feedback Collection: blueBriX’s digital tools allow providers to gather immediate feedback from patients post-appointment, identifying and addressing concerns promptly.
- Streamlined Communication: Patient portals facilitate easy scheduling, access to medical records, and direct communication with care teams, enhancing the patient experience.
- Customized Education: The platform provides tailored educational content to empower patients, improving their confidence in managing their health.
Impact: Increased Net Promoter Scores (NPS) due to simplified communication and timely responses to patient needs.
Physician Burnout Metrics
blueBriX addresses physician burnout by automating repetitive tasks and improving workflow efficiency.
- Administrative Task Automation: The platform automates documentation, coding, and billing tasks, freeing up time for providers to focus on patient care.
- Streamlined Workflows: Intuitive interfaces and integrated systems reduce time spent navigating complex EHR systems.
- Wellness Monitoring: blueBriX includes tools to monitor physician workload and satisfaction, providing insights to leadership for addressing burnout proactively.
Impact: Reduced administrative burden hours, improving work-life balance for providers.
Care Coordination Metrics
blueBriX promotes seamless collaboration among care teams and across healthcare settings, improving care coordination.
- Centralized Communication: The platform facilitates real-time information sharing among care teams, ensuring everyone is aligned on patient care plans.
- Referral Tracking: blueBriX tracks referrals and follow-ups, ensuring patients complete recommended treatments or specialist visits.
- Integrated Care Plans: Providers can collaborate on a single, unified care plan within the platform, reducing gaps in care.
Impact: Increased referral completion rates through real-time tracking and streamlined communication.
Preventive Care Metrics
blueBriX supports preventive care initiatives with tools that encourage proactive health management.
- Patient Outreach Campaigns: Automated reminders and personalized communication tools help ensure patients schedule and attend screenings, vaccinations, and wellness visits.
- Population Health Management: blueBriX identifies at-risk populations and enables targeted preventive interventions.
- Data Integration: The platform combines data from various sources, including wearables and EHRs, to provide a comprehensive view of patient health and track preventive care adherence.
Impact: Increased vaccination rates and adherence to cancer screening schedules through automated reminders and targeted outreach.
blueBriX value-based care solutions are tailored to align seamlessly with each provider’s unique care delivery strategies and objectives. By leveraging blueBriX, healthcare providers can harness advanced technology and actionable information without disrupting existing workflows, ensuring enhanced automation and streamlined access.
Conclusion
By addressing key metrics such as patient outcomes, cost reduction, satisfaction scores, physician burnout, care coordination, and preventive care, blueBriX empowers providers to improve performance, reduce costs, and enhance the patient experience.
As the shift toward value-based care continues, blueBriX serves as a trusted partner in navigating the complexities of this model. To thrive in value-based care, it’s essential to not only measure but also act upon these metrics with precision and purpose.Start your journey toward better outcomes and operational excellence.Explore how blueBriX can transform your practice and drive success in value-based care today.