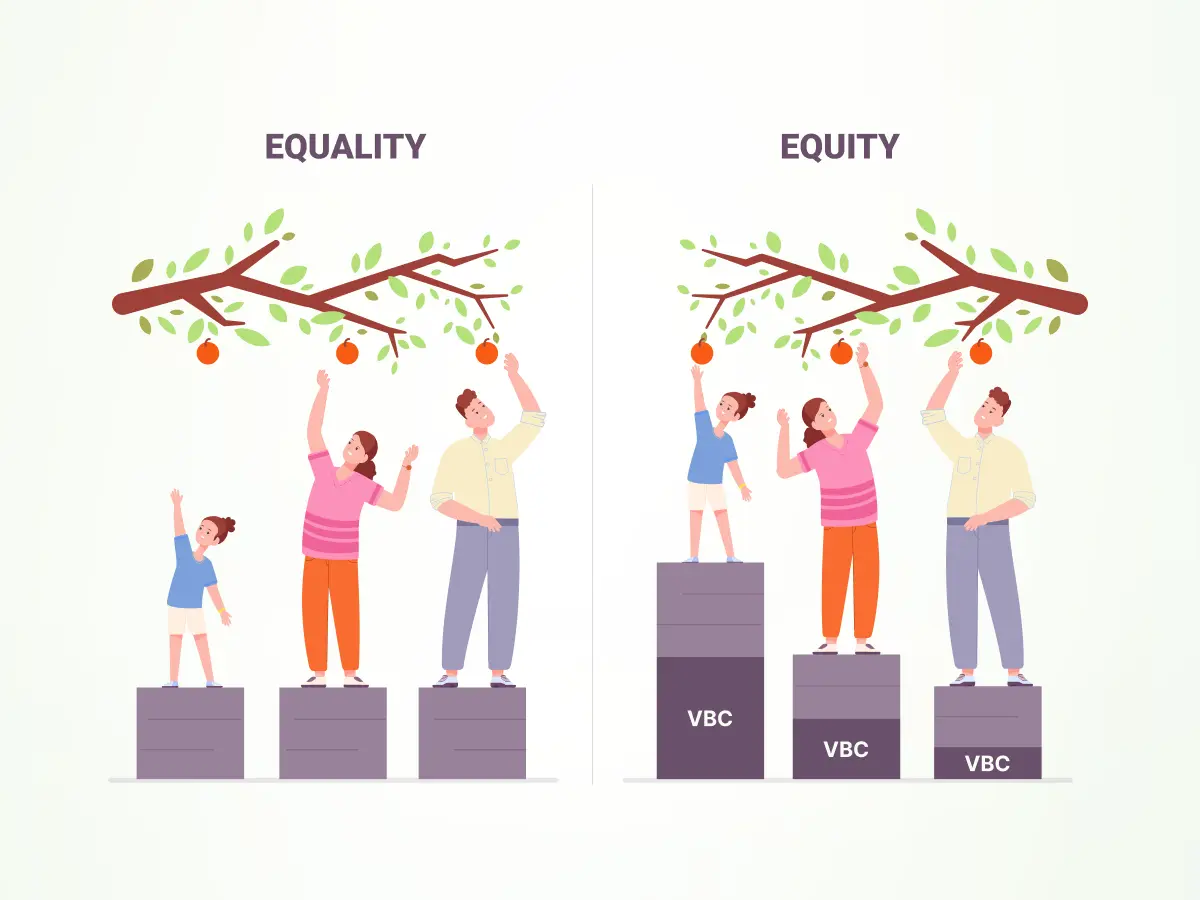
The US healthcare ecosystem is transitioning to value-based care (VBC) aiming at improving health outcomes and reducing healthcare costs. However, achieving true equity in healthcare remains a pressing challenge.
Imagine two people:
Alex and Riley. Alex lives in a safe neighborhood with access to fresh food, good schools, and quality healthcare. Riley lives in a community with high crime rates, limited access to healthy options, and overcrowded schools.
Health equity means ensuring both Alex and Riley have the same opportunities to be healthy, regardless of where they live. It’s about giving Riley the same chances as Alex to thrive.
Let’s understand health equity, social determinants of health, health equity gap and how to close the gap using data analytics in this blog. We’ll cover the following:
- Understanding healthcare equity and why it matters
- Social determinants of health & the equity gap
- Challenges in closing the health equity gap
- Strategies for success
- The future of equitable health
Healthcare Equity: Why does it matter?
Health equity is a concept rooted in fairness and justice within public health and healthcare delivery. It acknowledges that people’s health depends not only on individual decisions and heredity but also on social, economic, environmental, and structural factors in which people live, also known as Social Determinants of Health (SDOH).
Value-Based Care requires a significant shift from the current norm of fee-for-service model in healthcare delivery. VBC focuses on improving patient outcomes and reducing costs by rewarding providers based on healthcare quality provided rather than quantity of services. While this model holds promise, it also highlights disparities in healthcare access and outcomes among different demographic groups. Alabamans with low incomes are 7 times more likely to put off necessary medical care because of cost. Inequalities in healthcare continue to exist, with marginalized groups receiving limited or poor-quality care. Equitable healthcare is possible only by addressing such disparities.
The World Health Organization (WHO) believes everyone deserves a fair chance at good health. This means addressing the unfair differences in health outcomes between different groups of people. These differences aren’t just about biology; they’re often caused by social factors like where you live, your income, and your education. To achieve true health equity, we need to tackle these underlying issues and create opportunities for everyone to live healthy lives.
Knowing the Root Causes of Equity Gap

Socio-Economic Determinants of Health
SDOH considers the conditions in which people are born, grow up, live, work and age, which directly or indirectly contribute to their health outcomes. It plays a significant role, influencing up to 50% of a person’s overall health outcomes, as recognized by the U.S. Department of Health and Human Services (HHS).
The economic insecurity rooted in lower socioeconomic status draws limitations to care access and poor health outcomes. Poor living conditions and safety problems in the neighborhood can trigger respiratory and nervous system issues due to stress and a lack of activity. A 2019 study in Health Affairs highlighted that diabetes prevalence is notably higher in low-income neighborhoods. Moreover, the study revealed that income-related disparities in diabetes have progressively widened over the past decade. Strong social support networks and community engagement improve well-being, whereas barriers to healthcare access, including lack of insurance, higher cost of medications, inability to maintain a healthy diet and lifestyle due to financial constraints etc. hinder preventive care and timely treatment. These are SDOH, addressing which is crucial for reducing disparities and promoting equitable health outcomes.
Take diabetes, a common condition amongst people, regardless of their income groups and living conditions. The following table lists the disparate needs of people with diabetes. It is a classic example that showcases how social determinants of health affect health conditions and result in an equity gap.
| High-income groups with diabetes | Low-income groups with diabetes |
|---|---|
| Complex Care Needs: High-income individuals often have more complex health conditions, requiring specialized care and management. | Access to Healthcare: Lower-income individuals often face barriers to accessing quality healthcare, including preventive screenings and regular check-ups. This can delay diagnosis. |
| Time Constraints: Busy lifestyles can hinder consistent adherence to diabetes management plans. | Medication Adherence: High costs of diabetes medications can lead to non-adherence among low-income individuals, resulting in uncontrolled blood sugar levels and complications. |
| Psychological Stress: High-pressure jobs and demanding schedules can contribute to stress, impacting diabetes control. | Healthy Food Access: Limited access to fresh, nutritious foods in lower-income neighborhoods contributes to higher rates of obesity and type 2 diabetes. |
| Misconceptions about Diabetes: There’s a misconception that diabetes primarily affects low-income populations, leading to delayed diagnosis or inadequate care in high-income individuals. | Education and Health Literacy: Lower levels of education can impact diabetes self-management skills, leading to poorer health outcomes. |
| Accessibility Issues: Despite financial resources, geographical location or other barriers might limit access to specialized diabetes care. | Transportation: Difficulty accessing healthcare facilities due to lack of reliable transportation can hinder diabetes care. |
The high-income groups with diabetes have a different set of challenges compared to the low-income group with the same condition. Addressing such disparities requires a comprehensive approach that considers the unique challenges faced by both low and high-income populations.
Challenges in Closing Health Equity Gap
While analytics can help resolve the health equity disparity, many factors challenge the effectiveness of the gap analysis and implementation of recommended solutions. Many of these challenges can be resolved using the right digital health tools, though some require a larger social action such as building trust and addressing ethical matters. Let’s explore the major challenges:
- Data Fragmentation: Healthcare data from underserved communities is fragmented; the fragmentation may be between different providers or across different systems, it is cumbersome to have complete analysis and insights without getting a complete picture.
- Digital Divide: Due to restricted access to technology, incomplete or outdated base data can accumulate on digital health resources, hence exacerbating disparities in data-driven health interventions.
- Language and Cultural Barriers: Language diversity and cultural nuances can bias data collection and interpretation and require culturally sensitive approaches that ensure accurate representation.
- Transparency: Communicating clearly about how patient data will be used and protected builds trust and encourages participation.
- Poor Health Literacy: People from underserved geographical locations with limited access to the digital world may lack health literacy which impacts identifying health issues at the outset.
- Patient Empowerment: Involving patients in decision-making processes regarding their data promotes autonomy and ensures their perspectives are considered.
- Cultural Competence: Understand the cultural beliefs and practices; respect them to improve patient-provider relationships, which in turn improves data collection accuracy.
- Bias in Data: Historical biases in healthcare data, such as underrepresentation of minority groups, can perpetuate disparities if not properly addressed.
- Algorithm Interpretability: Making transparent the algorithm decisional processes, reducing biases in healthcare outcomes.
- Equity Impact Assessments: Regular assessments on different population groups about how algorithms affect them may be used to notice and rectify deviations of biases.
- Privacy and Ethical Considerations: Protecting sensitive patient data while leveraging it for the greater good is a complex balancing act.
- Collaboration and Partnerships: Addressing health disparities often requires collaboration with community organizations, government agencies, and other stakeholders, which can be challenging to coordinate.
Building SDOH-Informed VBC Programs with Data Analytics
Data analytics is a powerful tool for identifying and addressing health disparities. Data can pinpoint specific communities or demographics experiencing higher rates of chronic diseases, lower life expectancy, or limited access to care. By analyzing vast datasets, healthcare organizations can uncover patterns, trends, and disparities that contribute to health inequities. Data can quantify disparities in care, outcomes, and access to services, providing evidence for targeted interventions. Data can be used to assess the impact of programs and initiatives aimed at reducing health disparities, allowing for continuous improvement.
To effectively incorporate SDOH into Value-Based Care programs, leveraging data analytics is crucial. Here are some key strategies:
Data Collection and Integration
- Identify relevant SDOH data sources: This includes data from census, housing, education, and healthcare records.
- Develop a standardized data collection process: Ensure data consistency and accuracy across different sources.
- Integrate SDOH data with clinical data: Combine social and medical information for a comprehensive patient view. Integrating demographic, socioeconomic, and health-related data sets provides holistic SDOH insights for tailored interventions.
Data Analysis and Insights
- Risk stratification: Identify high-risk populations based on SDOH factors.
- Correlational analysis: Explore the relationship between SDOH and health outcomes.
- Predictive modeling: Forecast potential health risks based on SDOH and clinical data. Predictive modeling shows which populations are at a high risk and general trends in health care related to SDOH, thus helping develop proactive interventions.
Targeted Interventions
- Community-based programs: Develop programs addressing specific SDOH needs, such as housing assistance, nutrition education, or transportation support.
- Care coordination: Enhance care management by addressing SDOH barriers to care.
- Social service referrals: Connect patients with appropriate social services to address their needs.
Measurement and Evaluation
- Track SDOH-related outcomes: Monitor changes in health outcomes and disparities over time.
- Evaluate the impact of interventions: Assess the effectiveness of SDOH-focused programs.
- Refine strategies: Use data to continuously improve program design and implementation. Apply data-driven insights to highlight health-care disparities in need of policy reforms aimed at Health Equity and reducing SDOH.
Collaboration and Partnerships
- Build relationships with community organizations: Collaborate on SDOH initiatives. Engage with community organizations to understand better local SDOH dynamics as a driver of comprehensive program development.
- Engage with local government: Advocate for policies that support health equity.
- Partner with payers: Align VBC strategies with payer initiatives.
By effectively implementing these strategies, healthcare organizations can leverage data analytics to address SDOH, improve population health, and achieve better outcomes in value-based care. Using the right data analytics tools, healthcare organizations can gain a deeper understanding of health inequities, develop targeted interventions, and ultimately work towards a healthier and more equitable society.
A Healthier Tomorrow: The Future of Healthcare and Equity
The future of healthcare is inextricably linked to health equity. With the power of data analytics, artificial intelligence, and emerging technologies, we can envision a healthcare landscape where disparities are minimized, and everyone has an equal opportunity to achieve optimal health. A world with better health equity will come with:
- Personalized Precision Medicine: Tailoring treatments based on individual genetic makeup and lifestyle factors will lead to more effective and equitable care.
- Expanded Access to Care: Telehealth and remote monitoring will break down geographic barriers, improving access to care for underserved populations.
- AI-Driven Health Equity: Leveraging AI to identify and address disparities in data, treatment, and outcomes.
- Stronger Community Partnerships: Collaborating with community organizations to address social determinants of health.
- Patient Empowerment: Equipping individuals with tools and knowledge to manage their health proactively.
By prioritizing health equity and investing in innovative solutions, we can create a future where everyone thrives, regardless of their background or circumstances. At blueBriX, we believe advancing health equity isn’t just about better health – it’s about promoting social justice and human rights globally. As innovation and collaboration continue to drive progress, let’s seize this opportunity to build a healthcare system that is both just and equitable for future generations.