Excellence in healthcare isn’t just about skilled clinicians. It’s about how well teams work together. From ACOs and FQHCs to multi-specialty clinics and DPC practices, every organization dealing with complex care requirements, need the best care coordination software to streamline workflows, close gaps in patient care, and deliver better outcomes. Here are the top 7 platforms you need to know.

Let’s be honest: coordinating patient care can feel like juggling flaming torches while riding a unicycle. Between referrals, follow-ups, lab results, and care transitions, even the most organized teams can struggle to keep everyone on the same page. That’s why care coordination tools have become a game-changer.
The right platform doesn’t just track tasks—it gives your team a clear view of each patient’s journey, makes it easy to communicate across departments and providers, and ensures nothing slips through the cracks. Whether you’re running an ACO, a public health clinic, a multi-specialty practice, or a Direct Primary Care (DPC) model, investing in smart care coordination tools can save time, reduce stress, and improve patient outcomes.
In this guide, we’ll walk you through seven top care coordination platforms that are helping healthcare organizations take control of complexity and transform it into connected, patient-centered care. Think of this as your roadmap to smarter workflows, happier teams, and healthier patients.
Top 7 Care Coordination Software Platforms
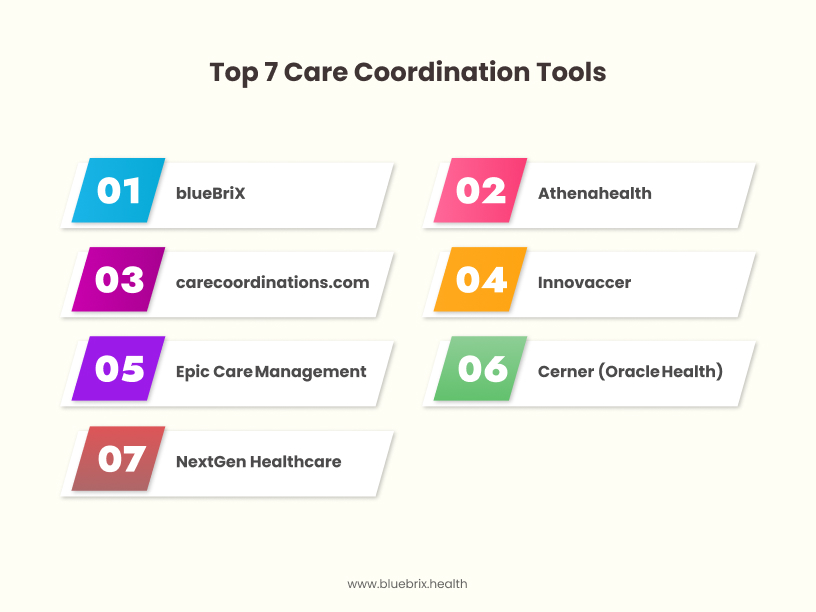
- blueBriX
- Athenahealth
- carecoordinations.com
- Innovaccer
- Epic Care Management
- Cerner (Oracle Health)
- NextGen Healthcare
1. blueBriX
blueBriX is designed for care teams who need coordination intelligence that actually fits their day-to-day work, not just static reports. It adapts to real patient journeys, enabling care teams to collaborate seamlessly across multiple disciplines. With a fast, non-disruptive deployment, it integrates into existing EHR systems without requiring a full IT overhaul.
Key Features & Strengths:
- Adaptive Longitudinal Care Plans:
Care plans evolve dynamically with patient progress. Teams can track interventions, monitor outcomes, and adjust treatments in real time, ensuring that care truly follows the patient, not a rigid template. - Multidisciplinary Team Collaboration:
Clinicians, social workers, care coordinators, and specialists can communicate directly within the platform. Tasks, notes, and updates are shared contextually, reducing miscommunication and ensuring accountability. - EHR-Agnostic Interoperability Layer:
While blueBriX comes with a robust native EHR, it also works with any existing EHR or data source. There’s no need to rip out legacy systems or disrupt ongoing operations, making it ideal for organizations with multiple platforms or complex IT environments. - Real-Time Patient Insights:
Teams have a consolidated view of each patient’s journey—current care status, upcoming tasks, risk alerts, and recent interventions—allowing for proactive decision-making and faster response to changes. - Automated Workflows & Task Management:
Routine follow-ups, referral tracking, and care transitions are automated, freeing staff to focus on meaningful patient interactions rather than manual coordination. - Scalable Across Care Models:
Whether you’re a DPC practice, an ACO, a multi-specialty clinic, or a public health network, blueBriX scales to fit your team size and organizational complexity, without introducing unnecessary overhead.
Best Suited For:
- ACOs and value-based care organizations: These teams need centralized oversight and real-time insights to manage complex patient populations across multiple providers.
- FQHCs and public health clinics: Organizations that serve diverse communities benefit from adaptive care plans and workflow automation to ensure patients don’t fall through the cracks.
- Multi-specialty practices and hospital networks: Large, multidisciplinary teams require seamless collaboration, task tracking, and interoperability across EHRs and departments.
- Direct Primary Care (DPC) practices: Smaller, agile practices need fast deployment and flexible workflows to deliver patient-centered care without disrupting daily operations.
- Care management and population health teams: Groups focused on longitudinal care plans and proactive interventions gain from real-time dashboards and automated follow-ups to improve outcomes.
2. Athenahealth
Athenahealth is a cloud-based platform that combines EHR, billing, and practice management with care coordination functionality. It emphasizes integrated workflows and patient engagement across ambulatory practices.
Key Features & Strengths:
- Cloud-based EHR and practice management
- Patient engagement tools (messaging, reminders, portal access)
- Reporting and analytics for population health
- Referral management and care tracking
Best Suited For:
- Small to mid-sized practices: Looking to unify EHR, billing, and care coordination in one platform.
- Ambulatory care clinics: Need integrated workflows for patient communication and task management.
- Organizations invested in Athena ecosystem: Benefit from seamless connectivity across Athena modules.
Note: While Athenahealth offers strong integration across its ecosystem, practices new to the platform may face a learning curve for complex care coordination workflows.
3. CareCoordinations.com
CareCoordinations.com is focused on structured care management workflows, enabling referral tracking, care plan documentation, and patient monitoring.
Key Features & Strengths:
- Structured care plan templates for chronic conditions
- Referral and care transition tracking
- EHR integration for data consistency
- Task assignment and workflow management
Best Suited For:
- Public health clinics and community health centers: Require structured management for diverse patient populations.
- Multi-specialty practices: Benefit from clear task ownership and workflow templates.
- Value-based care organizations: Need robust reporting and follow-up tracking for outcomes.
Note: The platform is structured and workflow-driven, which can feel rigid for teams looking for more flexibility in patient-centered workflows.
4. Innovaccer
Innovaccer focuses on data unification and analytics, providing insights for population health and care team coordination.
Key Features & Strengths:
- Population health analytics and dashboards
- Care team collaboration tools
- Data aggregation from multiple EHRs and sources
- Risk stratification and proactive care alerts
Best Suited For:
- ACOs and health networks: Need actionable insights for population health initiatives.
- Large multi-specialty organizations: Benefit from consolidated data and analytics.
- Care management teams: Use data-driven alerts and reporting to improve outcomes.
Note: Powerful analytics and data aggregation are strengths, but lack a robust native EHR. Smaller practices may find implementation and onboarding time-intensive.
5. Epic Care Management
Epic Care Management offers enterprise-grade coordination tools integrated deeply with Epic EHR systems. It supports complex workflows and large-scale organizations.
Key Features & Strengths:
- Comprehensive care management capabilities
- Tight integration with Epic EHR and modules
- Advanced reporting and analytics
- Task management for multidisciplinary teams
Best Suited For:
- Large hospital systems and health networks: Require enterprise-grade, integrated solutions.
- Organizations already using Epic EHR: Benefit from seamless integration.
- Population health teams: Need advanced analytics and reporting for large patient populations.
Note: Epic is enterprise-grade and feature-rich, but deployment and training often take months, making it less agile for fast-moving care teams.
6. Cerner (Oracle Health)
Cerner provides scalable enterprise care management tools with strong interoperability and analytics, suitable for large healthcare networks.
Key Features & Strengths:
- Enterprise-grade interoperability
- Population health management and reporting
- Task management and care coordination across departments
- Scalable to multi-hospital networks
Best Suited For:
- Large health systems and hospital networks: Require scalable solutions for complex care operations.
- Value-based care organizations: Benefit from population health analytics and integrated workflows.
- Multidisciplinary teams: Need centralized dashboards and automated task management.
Note: Cerner is scalable and robust, yet smaller or mid-sized organizations may find it resource-heavy and slower to implement.
7. NextGen Healthcare
NextGen Healthcare is designed for ambulatory and multi-specialty practices, offering flexible coordination tools integrated with NextGen EHR.
Key Features & Strengths:
- Ambulatory-focused care coordination
- Task automation and patient communication
- Integration with NextGen EHR and PM systems
- Reporting and workflow management
Best Suited For:
- Multi-specialty practices and smaller health systems: Need workflow support and task management without enterprise complexity.
- Ambulatory clinics: Benefit from patient communication tools and automated follow-ups.
- Care management teams: Use NextGen’s integration to streamline coordination and reporting.
Note: NextGen is flexible for ambulatory settings, but advanced care coordination features may require customization and staff training to fully leverage.
Why Care Coordination Software Matters Today
As our care settings are evolving, patients are moving between specialists, labs, hospitals, and primary care. Every handoff is an opportunity for something to slip through the cracks. Miscommunication, siloed data, and scattered workflows don’t just slow teams down and can impact patient outcomes.
Modern care platforms act as a central hub, consolidating information, automating routine tasks, and enabling providers to collaborate effectively across the continuum of care. This translates into faster decision-making, fewer errors, and more proactive patient management.
Whether you’re an ACO, FQHC, public health clinic, multi-specialty practice, value-based care organization, or DPC, having the right platform can turn reactive, chaotic care into proactive, connected, and patient-centered delivery.
The takeaway: The best tools do more than check boxes. They give your team real-time visibility, actionable insights, and workflow automation, so every patient is supported, every transition is smooth, and no one falls through the cracks. In short, they make delivering quality care feel a whole lot easier.
Comprehensive Checklist: Choosing the Right Care Coordination Software
Use this questionnaire to assess and compare platforms before finalizing your care coordination tool. Score each item or take notes to guide your decision.
1. Workflow Alignment
- Does the platform support your real-world care processes without forcing teams to adapt?
- Can it handle different care models (DPC, multi-specialty, ACOs, FQHCs)?
2. EHR & System Integration
- Can it integrate seamlessly with your existing EHR(s) and other systems?
- Is it truly EHR-agnostic, or will it require replacing legacy systems?
3. Scalability & Flexibility
- Can it scale across locations, teams, and patient populations?
- Does it allow for future growth without major IT changes?
4. Multidisciplinary Collaboration
- Can care teams communicate in real time across specialties?
- Are tasks, notes, and updates shared contextually to reduce errors?
5. Automation & Workflow Efficiency
- Does it automate follow-ups, referrals, and care transitions?
- Can it reduce administrative burden for staff without losing oversight?
6. Real-Time Insights & Analytics
- Are dashboards and alerts actionable?
- Does it provide reports that tie directly to patient outcomes and organizational KPIs?
7. Deployment & Onboarding
- How quickly can it be deployed?
- Will implementation disrupt daily operations?
- What training and support are included?
8. Patient Experience
- Does it enhance communication and engagement for patients?
- Are reminders, care plan visibility, and coordination tools patient-friendly?
9. Compliance & Security
- Is it HIPAA-compliant and secure for patient data?
- Are audit trails and reporting available for regulatory needs?
10. Vendor Support & Longevity
- Does the vendor offer ongoing support and updates?
- Are there references or case studies demonstrating long-term success?
The Future of Care Coordination: Smarter, Faster, and More Connected
Healthcare is evolving at a pace like never before, and so is the way care teams collaborate. The future of care coordination is no longer just about tracking referrals or sharing notes—it’s about creating intelligent, proactive systems that anticipate patient needs and streamline every handoff across the care continuum.
Here’s what’s coming:
- AI and Predictive Insights: Platforms will increasingly use AI to identify high-risk patients, flag potential gaps in care, and suggest next-best actions for care teams. Instead of reacting to problems, teams can act before issues escalate.
- Seamless Interoperability: True data fluidity across systems will become standard. Whether it’s hospital EHRs, lab systems, or telehealth platforms, care teams will operate in a unified digital ecosystem, making every patient transition smoother and safer.
- Patient-Centered Automation: Routine follow-ups, reminders, and care plan updates will be automated, freeing clinicians to focus on meaningful patient interactions. Patients will experience coordinated care without feeling like a number on a list.
- Collaborative, Multidisciplinary Workflows: Teams across specialties, locations, and organizations will work together in real time, supported by dashboards, shared care plans, and instant communication tools. Collaboration will no longer be siloed; it will be baked into the platform.
- Outcome-Driven Metrics: With advanced analytics and integrated reporting, organizations will measure not just efficiency, but actual patient outcomes, tying care coordination directly to quality metrics, value-based incentives, and population health goals.
The future of care coordination isn’t a distant vision; it’s unfolding now. Organizations that embrace flexible, interoperable, and intelligent platforms will not only improve outcomes and reduce operational strain but also stay ahead in a rapidly evolving healthcare landscape.
The takeaway: The next generation of care coordination tools will shift healthcare from reactive to proactive, from fragmented to connected, and from transactional to truly patient-centered.
Connect Care, Improve Outcomes, and Move Forward
Coordinating patient care is no longer optional. It’s mission-critical! From ACOs and FQHCs to multi-specialty clinics and DPC practices, every organization faces the challenge of managing complex patient journeys across multiple providers and systems. Missed handoffs, delayed referrals, and siloed communication aren’t just operational headaches. They directly impact patient outcomes, satisfaction, and even revenue.
The right care coordination software can turn this complexity into clarity. Platforms like blueBriX offer fast deployment, real-world workflow alignment, and seamless integration with existing EHRs, helping care teams collaborate, track progress, and act proactively.
Why you shouldn’t wait: Every day your team operates with fragmented workflows is a day patients may slip through the cracks, delays pile up, and opportunities for improved outcomes are missed. The sooner your organization implements a platform that fits your workflows and supports real-time collaboration, the sooner you can reduce inefficiencies, improve adherence, and deliver care that truly matters.
The future of healthcare rewards teams that can move quickly, see the full patient picture, and act on insights in real time. Investing in a modern care coordination platform is all about giving your care teams the tools to deliver smarter, faster, and more effective care.
Inefficient care coordination contributes to approximately $27.2 billion to $78.2 billion in unnecessary healthcare spending annually in the United States. Don’t let indecision slow your team or compromise patient outcomes. The time to choose the right care coordination platform is now. Streamline collaboration, close gaps in care, and make every handoff count. Let’s connect!