The surge of healthcare technology was meant to simplify care delivery, but instead, it has evolved into a sprawling ecosystem of disconnected tools. A 2024 survey of more than 900 health IT leaders found that outdated and poorly integrated systems cost U.S. healthcare nearly $8 billion annually in operational inefficiencies, fueling the digital chaos providers navigate daily. Physicians now toggle between five or more platforms to access complete patient information, resulting in fragmented care, staff fatigue, and compromised outcomes.
Each day spent managing these disconnected systems adds complexity that slows care and increases risk. As clinician demands rise and regulations tighten, the urgency to unify workflows and data has never been greater. Leadership, clinicians, and administrators must act now to break down silos, strengthen coordination, and build streamlined, patient-centered systems before these hidden costs escalate further.
This blog explains why unified healthcare systems matter and how they work.
Siloed systems, scattered care: how disconnected systems disrupt care coordination and continuity
Your individual systems may get the job done for specific tasks, but will they help you achieve the bigger goal: unified care coordination? This disconnection in integration is the main fracture in care delivery today. When platforms, patient data, and workflows are scattered across siloed systems, it becomes nearly impossible to provide seamless, continuous care. These silos result in critical information gaps, inefficiencies, burnout, delayed decisions, and ultimately fragmented patient experiences.

Breakdowns in transitions
Critical updates during care handoffs across hospitals, specialists, and primary care often get lost or delayed due to disconnected systems. This increases risks of hospital readmissions and missed follow-up appointments, disrupting the continuum of care and leading to poorer outcomes for patients.
Redundant testing and missed history
When your records are fragmented, you end up ordering repeat tests or procedures for your patient because previous results are scattered or simply not available where you need them. This leads to unnecessary costs and inconveniences for your patients.
Medication and treatment errors
Disconnected systems mean incomplete medication lists and missing allergy information. You can’t see what your patients are already taking or allergic to, leading to dangerous drug interactions and preventable harm.
Communication failures
Your care teams juggle between multiple communication channels like phones, emails, faxes, fragmented apps to share critical patient information and coordinate care. But this constant juggling consumes valuable time, increases the chances of errors, slows urgent decision-making, and causes duplicated efforts. Messages get missed, updates arrive late, and critical information doesn’t reach the right people when it matters most, hampering timely interventions and putting patients at risk.
Inaccurate or delayed documentation
When you need to reconcile conflicting or incomplete data from several systems, clinical documentation suffers delays and inaccuracies. This impacts not only patient care decisions but also timely coding and billing, affecting financial health and regulatory compliance.
Poor patient experience
Patients often must repeat their histories, receive inconsistent plans, and feel lost in a fragmented care process. This erodes trust, reduces satisfaction, and negatively affects engagement and adherence, creating barriers to effective chronic disease management.
Operational and financial inefficiency
Fragmentation in healthcare systems inflates costs by creating inefficiencies, avoidable clinical complications, and administrative burdens. This not only wastes valuable resources but also undermines efforts to succeed in value-based care by limiting care coordination and preventing maximum reimbursement opportunities.
What a unified care coordination platform means
A unified care coordination platform is a comprehensive digital platform designed to bring together clinical and operational workflows into a single, seamless solution. Its primary goal is to streamline communication, optimize workflows, and provide actionable insights that enhance patient care while supporting efficient healthcare operations.
Core components of the platform
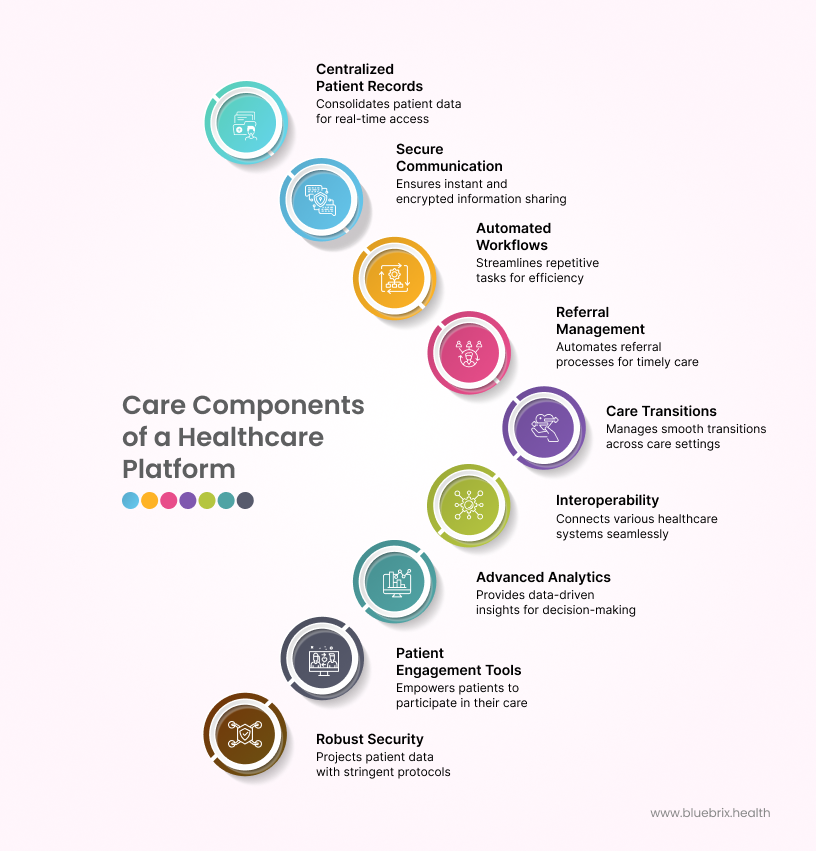
Centralized patient records
All patient data like clinical history, medications, allergies, social determinants, care goals are consolidated. Care teams get a complete, real-time view of each patient without hunting through multiple systems. This eliminates duplicate tests, prevents information gaps, and supports better clinical decisions.
Secure real-time communication
Encrypted messaging and alert systems let care teams share critical information instantly. No more phone tags or delayed updates. The right information reaches the right people immediately, preventing care delays and reducing errors caused by communication breakdowns.
Automated workflows and task management
Repetitive tasks like appointment scheduling, referral tracking, and care follow-ups run automatically. Staff spend less time on administrative work and more time on patient care. Automation ensures nothing falls through the cracks and timely interventions happen consistently.
Robust referral management
The platform automates the entire referral process, from request to specialist follow-up. Referrals are instantly routed, status updates shared in real time, and all communication tracked in the patient’s record. Nothing gets lost or delayed. Every referral is accounted for, and patients get timely access to the care they need.
Active care transitions and handoffs
The platform manages smooth transitions across care settings, from hospital to home and hospital to primary care. Automated alerts notify all providers when transitions happen. Updated records are instantly shared. Care teams know what to do next, medications are reconciled, and follow-up appointments are confirmed. This eliminates care gaps and reduces preventable readmissions.
Interoperability across systems
The platform connects seamlessly with EHRs, labs, telehealth platforms, pharmacies, and payer systems using standards like HL7 and FHIR. Patient data flows accurately between systems without manual data entry or reconciliation, enabling true care coordination.
Advanced analytics and reporting
Aggregated data generate actionable insights on patient outcomes, resource use, care gaps, and population health trends. Providers and administrators make data-driven decisions that improve care quality and operational efficiency instead of relying on incomplete information.
Patient engagement tools
Patients access secure portals and mobile apps to view care plans, communicate with providers, schedule appointments, and get educational resources. When patients can actively participate in their care, adherence improves, and outcomes get better.
Reliable security and compliance
Built with stringent security protocols such as data encryption, role-based access, multi-factor authentication, and audit trails, the platform ensures compliance with healthcare regulations like HIPAA. This protects patient privacy and builds trust among patients and providers alike.
How blueBriX solves the care coordination crisis
Here’s how blueBriX integrates data, workflows, and intelligence to streamline operations, strengthen clinical collaboration, and enhance care quality.
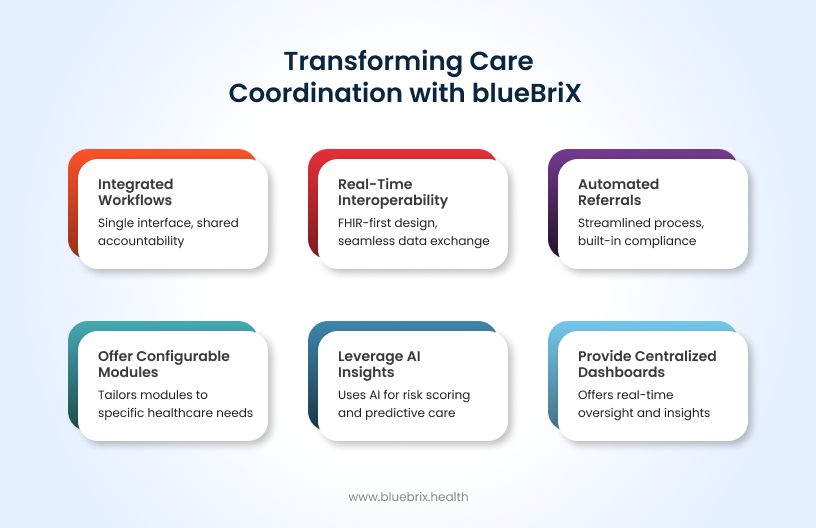
Built for both operational and clinical excellence
blueBriX integrates administrative and clinical workflows within a single interface, allowing frontline teams to operate with shared information and shared accountability. Operational leaders gain visibility into referral completion rates, turnaround times, and staff workload, while clinicians access up-to-date patient data and communication tools in real time. This dual focus ensures efficiency doesn’t come at the cost of quality care.
FHIR-first design enabling real-time interoperability
blueBriX is built on FHIR architecture, enabling real-time data exchange across EHRs, labs, imaging systems, payers, and other health IT platforms. It supports bidirectional communication with legacy HL7 and C-CDA systems, ensuring compatibility with existing infrastructure while staying future-ready. The result: a truly interoperable ecosystem that eliminates manual data reconciliation and supports seamless care continuity.
Automated referral workflows with built-in compliance
Traditional referrals fail because of manual tracking and missing documentation. blueBriX automates every stage, starting from referral initiation and status alerts to provider confirmations. Built-in compliance checkpoints ensure proper documentation, consent, and follow-up notes are captured automatically, reducing delays and audit risk. Every care transition has full accountability and traceability.
Centralized dashboards for real-time oversight
Stakeholders and care managers get consolidated dashboards showing clinical performance metrics alongside operational KPIs. Monitor patient throughput, referral conversion rates, coding completeness, and more all in one place. blueBriX turns fragmented reporting into a single view of actionable insight, giving executives visibility and operational control simultaneously.
Configurable modules tailored to your needs
You receive access to ready-to-use modules such as telehealth, scheduling, billing can be deployed immediately. There’s no need to build anything from scratch or endure long development delays. Whether you are part of a hospital, ACO, or behavioral health network, these modules can be configured to fit your specific workflows, local policies, and payer requirements. This approach ensures faster implementation and lets your system evolve smoothly alongside your organization’s needs.
AI-powered risk scoring and predictive insights
blueBriX leverages AI-powered risk scoring and predictive insights to help care teams proactively identify patients at risk of complications or gaps in care. By analyzing clinical data, social determinants, and historical patterns, the platform prioritizes interventions, anticipates care needs, and enables more informed decision-making. This predictive approach ensures timely, targeted, and personalized care coordination, improving outcomes while reducing unnecessary costs and hospitalizations.

