Every behavioral health practice eventually hits that point where operations are getting bigger, payers are tightening rules, and compliance feels like a moving target. And right there, leadership faces a tough but familiar question:
Should you hand off billing to a company that knows the game inside out, or take control with a behavioral health EHR that keeps everything in-house?
At first glance, it seems like a trade-off between convenience and control. But anyone who’s been in this space knows the truth, it’s never that simple. Your choice here doesn’t just affect revenue cycles; it shapes how clinicians document, how compliant your data stays, and how scalable your operations will be as the business grows.
In the sections that follow, we’ll take an honest look at both sides:
- What billing companies actually bring to the table
- Where EHRs outperform them
- Why the most forward-thinking behavioral health practices are moving toward systems that blend the best of both worlds.
The “either/or” decision is quickly becoming outdated. The future belongs to unified behavioral health platforms that connect care, compliance, and cash flow in one place.
The case for billing companies: the shortcut that keeps practices afloat
If you’ve ever managed billing in a behavioral health practice, you know it can drain the life out of your day. Claims get rejected for the smallest errors, payers move the goalposts without notice, and before you know it, your team is spending more time fighting with portals than supporting patients.
That’s why many practices make the same strategic move, they outsource billing. And honestly, it makes sense. For a lot of organizations, this is the fastest way to stabilize revenue and reduce operational chaos.
Billing companies exist for one reason: to make sure you get paid faster, more consistently, and with fewer headaches. They know every payer quirk, every modifier rule, and every compliance update that matters to behavioral health. They live in that world, so you don’t have to.
Here’s why this model works. At least for a while.
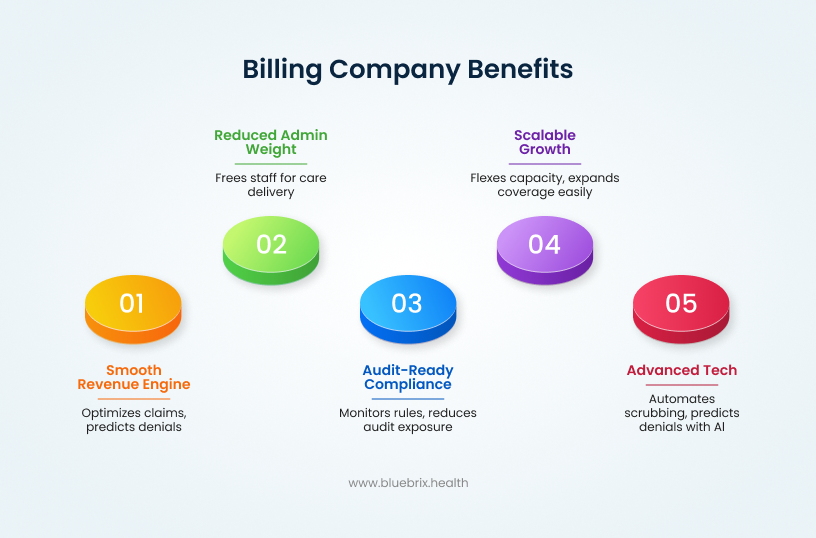
1. They keep the revenue engine running smoothly
Good billing companies know how to optimize claims so nothing slips through the cracks. They understand behavioral health-specific codes from therapy sessions and IOP programs to telehealth visits and besides, they know how to get them approved.
They stay on top of payer rule changes and use denial-tracking systems to spot problems before they snowball. That consistency is gold for practices that need predictable cash flow to stay operational.
The best ones even use analytics to identify underpaid claims and missed revenue opportunities. For most practices, getting that level of visibility in-house would take serious time, tech, and training.
2. They take the admin weight off your team
Behavioral health billing is a full-time job and then some. You’ve got insurance verification, pre-authorizations, claim scrubbing, denial management, patient statements; all pulling your staff away from care delivery.
Outsourcing gives your clinicians and front-office team breathing room. It reduces internal churn and lowers the need to constantly recruit and train billing staff. The workflow becomes simpler, and the administrative noise drops significantly.
The result? Happier staff, fewer billing errors, and a lot less time spent chasing down claims.
3. They help you stay audit-ready and compliant
Billing companies also take on the role of compliance watchdog. They keep up with every new payer requirement, documentation rule, and audit guideline including behavioral health’s unique demands like treatment plan validation, medical necessity notes, and prior authorization tracking.
Their proactive monitoring means fewer compliance mistakes and less exposure during payer audits. You get peace of mind knowing your billing stands up to scrutiny.
4. They scale as you grow
Growth is great until it breaks your systems. As your practice adds new programs, locations, or providers, scaling an internal billing team can be a nightmare.
Billing vendors, on the other hand, can flex capacity almost instantly. Need to process more claims or add new service types like telehealth or group therapy? They can expand coverage without you hiring a single new staff member.
That flexibility makes them a reliable partner during growth phases or payer expansion cycles.
5. They bring tech you don’t have to pay for
Unlike most billing companies that rely heavily on manual processes, blueBriX integrates advanced technology directly into its RCM operations. With automation for claim scrubbing, AI-driven denial prediction, and real-time reimbursement dashboards, blueBriX ensures revenue flows stay consistent and transparent.
That gives you advanced financial insights without forcing you to buy or maintain expensive software. In many ways, it feels like upgrading your revenue cycle without upgrading your IT department.
So yes, partnering with a billing company without the right technology can sometimes feel like plugging a hole in a leaking boat. You gain speed, stability, and short-term relief, but the real efficiency comes when billing is backed by technology that connects directly to your clinical data.
That’s where blueBriX stands apart; combining experienced billing operations with intelligent, tech-driven processes that keep revenue flowing seamlessly and insightfully.
The limitations of relying solely on billing companies
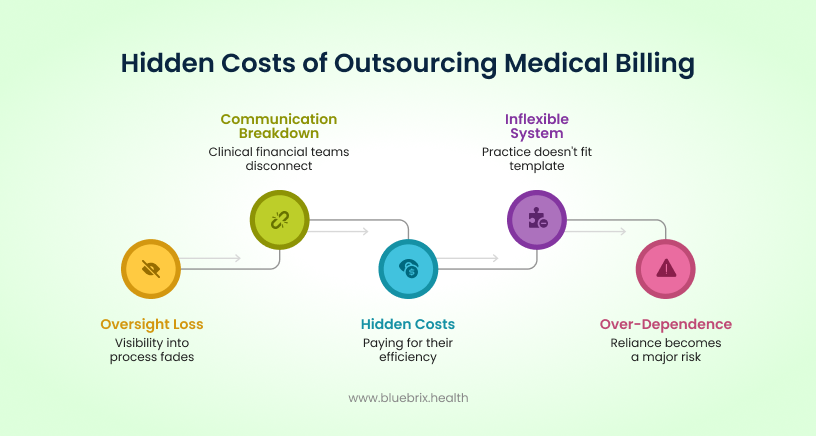
Outsourcing billing is often a practical and effective way to keep revenue cycles steady. It brings much-needed relief to busy behavioral health teams and ensures claims are handled by specialists who know the payer landscape inside out. But when billing operates entirely outside your clinical system, small inefficiencies can start to compound.
The real challenge isn’t with the billing companies themselves — it’s with the lack of integration. When clinical data and billing processes live in separate systems, oversight becomes harder, communication slows, and decision-making gets delayed. Leaders end up relying on periodic reports instead of real-time insight, which can make it difficult to trace denials or identify performance trends.
Most billing companies also work within standardized frameworks, which, while efficient, don’t always flex easily for behavioral health programs that combine therapy, psychiatry, and group services. Over time, those rigid workflows can create friction that impacts both speed and accuracy.
That’s why many forward-looking organizations are shifting toward a hybrid model, one that pairs expert billing services with technology designed to connect care, compliance, and revenue at the source. blueBriX was built around that very principle: combining deep RCM expertise with a unified, tech-driven infrastructure that keeps billing, documentation, and analytics in sync.
In short, outsourcing can stabilize your revenue but true scalability comes when that billing expertise is powered by technology that keeps your clinical and financial data moving together.
The promise of top ehrs: integration, insight, and interoperability
If billing companies keep your revenue flowing, EHRs keep your operations connected. They don’t just manage documentation; they shape how care, compliance, and cash flow come together behind the scenes.
In behavioral health, that connection matters more than ever. You’re not just billing for services; you’re managing complex care journeys, documenting progress notes, tracking outcomes, and proving medical necessity. That’s where behavioral health EHRs shine. They bring everything into one system of record, where care data and billing data actually talk to each other.
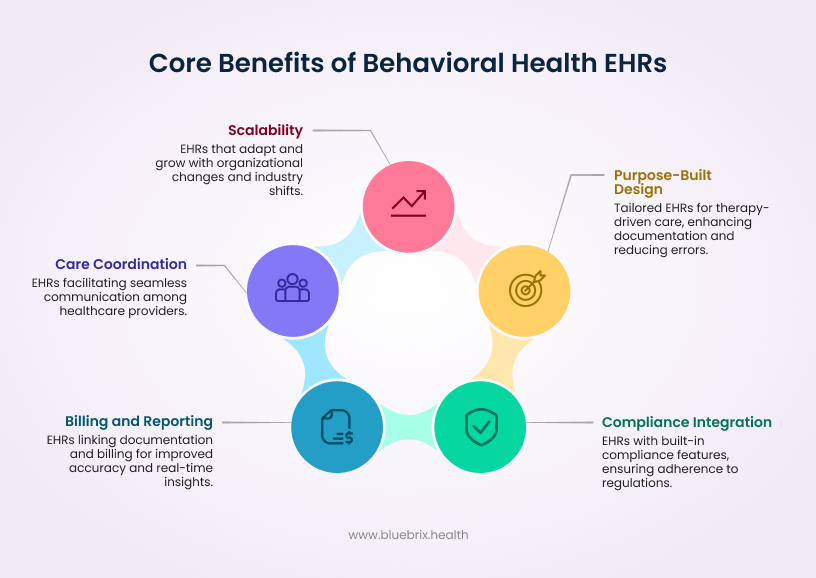
1. Purpose-built for behavioral health care
Generic EHRs struggle to capture the nuances of therapy-driven care. Behavioral health EHRs are built differently. They’re designed for the real-world flow of therapy notes, treatment plans, group sessions, and outcome tracking.
The templates adapt to each clinician’s workflow, cutting down redundancy, and improving documentation speed. The result? Fewer errors, better compliance, and cleaner documentation that translates directly into more accurate behavioral health billing.
Every note tells a complete story; not just for auditors, but for payers too, ensuring claims reflect the full clinical context and get approved faster.
2. Compliance built right into the workflow
Behavioral health practices live in one of the most regulated corners of healthcare. Between HIPAA, 42 CFR Part 2, and constant payer audits, compliance can’t just be an afterthought. It has to be part of how your team works every day.
Top behavioral health EHRs bake compliance into the process. They include role-based access controls, automatic audit trails, and data segmentation for sensitive substance use or mental health information.
That means your clinicians don’t have to worry about whether a note or signature meets a regulation, instead, the system makes sure it does.
3. Care coordination that actually works
Modern behavioral health care is rarely delivered in isolation. Your patients often see multiple providers including therapists, psychiatrists, primary care physicians, and even social workers. Coordination across that network can be a nightmare without proper data flow.
Advanced behavioral health EHRs solve that by enabling secure, real-time integration with primary care systems, community programs, and payer networks. Referrals, updates, and care plans move automatically between teams, creating a more connected care experience without compromising privacy.
And when care is connected, outcomes improve. Patients stay more engaged, transitions are smoother, and your team doesn’t waste hours chasing down information that should already be there.
4. Billing and reporting that work hand in hand
This is where behavioral health EHRs start closing the gap with billing companies. Instead of exporting data for someone else to clean up, billing happens directly from the same system clinicians use every day.
Because documentation and billing are linked, claim accuracy improves dramatically. The EHR catches missing modifiers, incomplete authorizations, and coding errors before a claim ever leaves the system. That means fewer denials, faster payments, and no surprises during audits.
Plus, built-in reporting tools give leaders real-time visibility into performance from reimbursement timelines to clinician productivity and payer mix. You’re no longer waiting for end-of-month reports; you can see what’s happening as it happens.
5. Scalable systems that evolve with you
Behavioral health organizations don’t stand still. You might add new programs, expand locations, or take on value-based contracts. A strong behavioral health EHR scales with you.
The best systems are modular, allowing you to add analytics, telehealth, population health tracking, or Medicaid reporting without disrupting what’s already working. They’re designed to evolve as payer models and compliance frameworks shift, so your operations stay consistent even when the industry doesn’t.
In short, behavioral health EHRs give practices control. They connect data, automate documentation, and align billing with care delivery. But even the best systems have a ceiling.
Because while they master the clinical and compliance side of the equation, most EHRs still struggle with the full financial picture. That’s the next piece of the story and it’s where the future of behavioral health tech is heading.
The gaps in most EHR-only systems
Behavioral health EHRs have come a long way. They’ve solved major pain points around documentation, compliance, and data visibility. But if you’ve ever run your practice entirely through one, you already know the catch. EHRs aren’t built to manage the full business of healthcare.
They handle the “care” part beautifully. The “revenue” part? Not so much.
Let’s break that down.
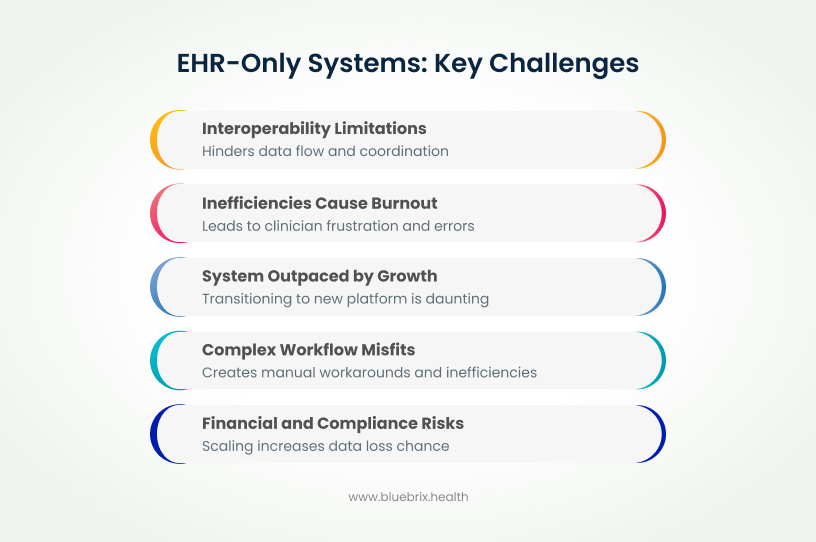
1. Interoperability still has a long way to go
Most EHRs work well within their own walls but struggle to communicate beyond them. Integrating with primary care, hospital networks, or payer systems often requires custom workarounds or outdated data exchange methods.
In behavioral health, that isolation is costly. When your data can’t flow to other providers or payers, you lose out on referrals, collaboration opportunities, and participation in value-based care programs.
Even modern standards like FHIR and HL7 aren’t always implemented consistently. That leaves behavioral health practices stuck on the sidelines of broader care coordination efforts not by choice, but by design.
2. Complex workflows don’t always fit
Behavioral healthcare rarely follows a straight line. Patients move between therapy, psychiatry, case management, and external support services sometimes within the same episode of care. Most EHRs, however, are designed around linear workflows.
That means you end up working around your system instead of with it. Teams rely on manual logs, spreadsheets, or external tools just to keep programs in sync. Over time, that patchwork drains productivity and clouds visibility into what’s actually happening across the organization.
It’s not that EHRs can’t support complex care models, it’s that most weren’t built with them in mind.
3. Inefficiencies that lead to burnout
If your clinicians complain about too many clicks, they’re not exaggerating. Many behavioral health EHRs try to do everything, but in doing so, they often sacrifice usability. Rigid templates, outdated design, and endless navigation steps turn documentation into a chore.
The result? Clinician frustration, rushed notes, and declining data quality all of which feed directly into compliance and billing errors. Over time, that digital fatigue becomes a major driver of burnout, something behavioral health can’t afford to overlook.
4. Financial and compliance risks multiply at scale
As practices grow, the cracks widen. Smaller teams can manage with partial automation and manual oversight, but scaling up without integrated billing and compliance tools invites risk.
Standalone EHRs typically rely on third-party add-ons or exports to handle revenue cycle management. Every extra handoff increases the chance of data loss, duplication, or compliance gaps.
And since many EHRs weren’t built for enterprise-level security, maintaining HIPAA and 42 CFR Part 2 compliance across multiple sites becomes more expensive and more complicated with every expansion.
5. Growth eventually outpaces the system
EHRs that once fit perfectly eventually become a bottleneck. Whether it’s limited analytics, slow updates, or outdated infrastructure, growth eventually tests the limits of what standalone systems can handle.
By the time a practice realizes this, transitioning to a new platform feels daunting. Data migration is messy, staff retraining is disruptive, and leadership hesitates to risk downtime. The organization ends up stuck operationally stable but strategically stagnant.
So yes, basic EHRs have changed the game, but they’re not the endgame. They’re a critical piece of the behavioral health puzzle, just not the whole picture.
As practices look beyond documentation and compliance, the next question becomes clear: What if your clinical system could manage the financial side too. Even without adding new vendors or integrations?
That’s where the next evolution of behavioral health technology is already heading.
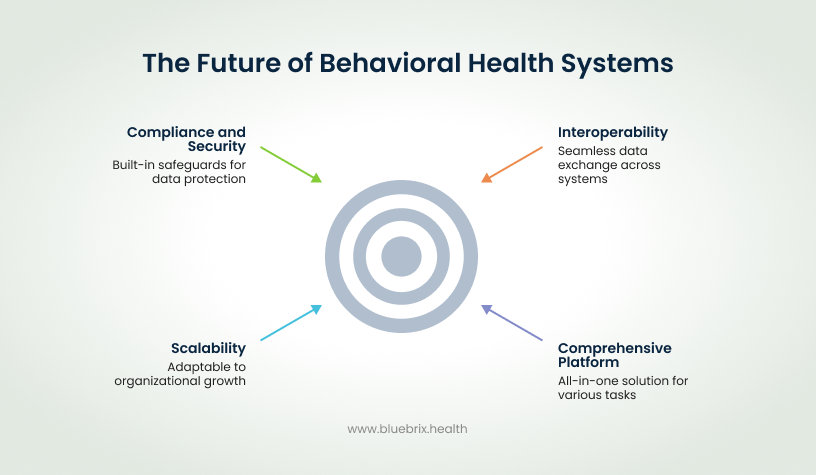
The future model: unified systems that combine clinical and financial intelligence
The next generation of behavioral health technology isn’t about choosing between a billing company or an EHR. It’s about eliminating that choice entirely.
The smartest organizations are moving toward unified platforms. That is systems that merge the clinical precision of a behavioral health EHR with the financial intelligence of a full revenue cycle engine. One login, one workflow, one data source.
Unified platforms bridge the gap between care delivery and cash flow, letting practices manage treatment plans, claims, reporting, and compliance from a single place. They remove the friction that’s been built into the healthcare process for decades the constant handoffs, the duplicate data, the siloed tools that make scaling so painful.
Here’s what that shift looks like in practice.
1. Interoperability that actually delivers
- A unified system connects everything your EHR, your billing, your scheduling, and even external networks like hospitals, payers, and referral partners.
- Data moves securely in real time across the entire care ecosystem. That means fewer phone calls, fewer faxes, and fewer blind spots in care coordination.
- By adhering to modern standards like FHIR and HL7, these platforms make it easy for behavioral health organizations to participate in value-based care models where outcomes, not just services, drive reimbursement.
2. One platform, every capability
- Instead of juggling separate systems for documentation, billing, telehealth, and analytics, unified platforms combine them all.
- Imagine your therapist documenting a session, and that note instantly validating against payer rules, generating the right claim code, and syncing into reporting dashboards automatically. No data entry, no manual review, no waiting for a third-party system to catch up.
- It’s behavioral health management in real time, not after the fact.
3. Scalable, adaptive, and always evolving
- The problem with traditional systems is that they don’t grow with you. Unified platforms fix that. They’re modular and configurable, allowing you to scale operations without tearing anything down.
- New program? Add it. New payer model? Configure it. Multi-site expansion? Turn it on. Everything adjusts around your growth and not the other way around.
- Because these systems are built with future regulations, AI-driven analytics, and compliance automation in mind, they evolve right alongside your organization.
4. Compliance and security you can trust
- In behavioral health, compliance can’t be delegated. It needs to be built into your workflow.
- Unified platforms keep compliance guardrails in place at every step. They monitor HIPAA, 42 CFR Part 2, and payer-specific rules automatically flagging errors before they become liabilities.
- And because data never leaves the system, you get end-to-end security. No third-party transfers, no missing audit trails, and no guessing who has access to what.
In short: the future of behavioral health operations isn’t about better billing companies or smarter EHRs it’s about integration. It’s about building one intelligent infrastructure where care delivery, compliance, and cash flow are no longer competing priorities.
Practices that adopt this model are actually building operational ecosystems that are faster, safer, and ready for what’s next.
The new standard in behavioral health operations
The debate between top billing companies and top behavioral health EHRs is ending where it always was headed; in the middle.
Both models brought something valuable. Billing companies deliver speed and expertise. EHRs deliver structure and compliance. But neither can truly unify the business of care. Behavioral health operations today demand more than accurate claims and organized notes. They demand connection, transparency, and real-time intelligence.
That’s why the future belongs to integrated behavioral health platforms: systems that bring clinical, financial, and operational workflows together under one roof.
These platforms don’t ask you to choose between efficiency and control. They give you both. They keep billing as close to the clinical source as possible, eliminate redundant work, and give leadership the one thing every growing practice need, that is visibility into everything that drives performance.
With a unified platform, your clinicians, billers, and administrators work from the same truth, the same data, the same insights, and the same mission. That’s not just better operations. That’s smarter care.

