In a value-based care model, success isn’t just about providers working together—it’s about ensuring the patient’s voice is central to the care journey.
Take a patient with chronic back pain. Instead of a top-down approach where doctors prescribe treatments in isolation, collaborative care planning ensures the patient is actively involved in shaping their care plan. The patient might prefer acupuncture over medication or want to explore physical therapy before considering surgery. By aligning the care plan with their goals, lifestyle, and preferences, engagement increases, leading to better adherence and improved outcomes.
When patients feel heard, they take ownership of their health—reducing hospitalizations, improving satisfaction, and driving the success of value-based care.
What is collaborative care planning?
Collaborative care planning is a patient-centered approach where healthcare providers, patients, and sometimes caregivers work together to design a personalized care plan. It’s not just about treating symptoms; it’s about creating a roadmap for better health outcomes, improved communication, and seamless coordination across different healthcare providers.
And here’s why it matters:
- Patients who actively participate in their care plans are 20% more likely to adhere to treatment recommendations.
- Collaborative care reduces hospital readmission rates by up to 25%.
- When care teams work together, patient satisfaction increases by nearly 30%.
It requires cooperation among diverse teams comprising specialists, doctors, and nurses to ensure that care aligns with patient objectives.
How does it work in real life?
Let’s say Sarah, a 55-year-old woman with diabetes, struggles with managing her condition. Traditionally, she would see different specialists who might not always be on the same page. But with collaborative care planning:
- Her primary care doctor, endocrinologist, and dietitian work together, sharing real-time updates.
- A care coordinator ensures she follows through with appointments and medication.
- Sarah herself is empowered with digital tools and a clear plan that helps her track her progress.
The result? Fewer complications, better blood sugar control, and a more engaged patient.
For healthcare organizations, collaborative care isn’t just about better patient outcomes—it’s also a financial win. Value-based care models reward providers for efficiency and improved results, and hospitals implementing collaborative care strategies have seen a 15-20% reduction in operational costs. With real-time data sharing, secure messaging, and AI-driven insights, providers can coordinate seamlessly. Telehealth-based collaborative care has led to a 35% increase in timely interventions. In this article, we will explore collaborative care planning in detail. We’ll see how blueBriX care management solutions make collaboration even easier.
Key components of collaborative care planning (and why they matter!)
Ever felt like your healthcare providers weren’t on the same page? You’re not alone. Up to 50% of treatment plans fail due to poor communication and lack of coordination. That’s where collaborative care planning comes in—it’s designed to bring all stakeholders together to improve patient outcomes.
So, what makes collaborative care planning truly effective? Let’s break it down into its key components—with real-world impact and numbers that back it up!
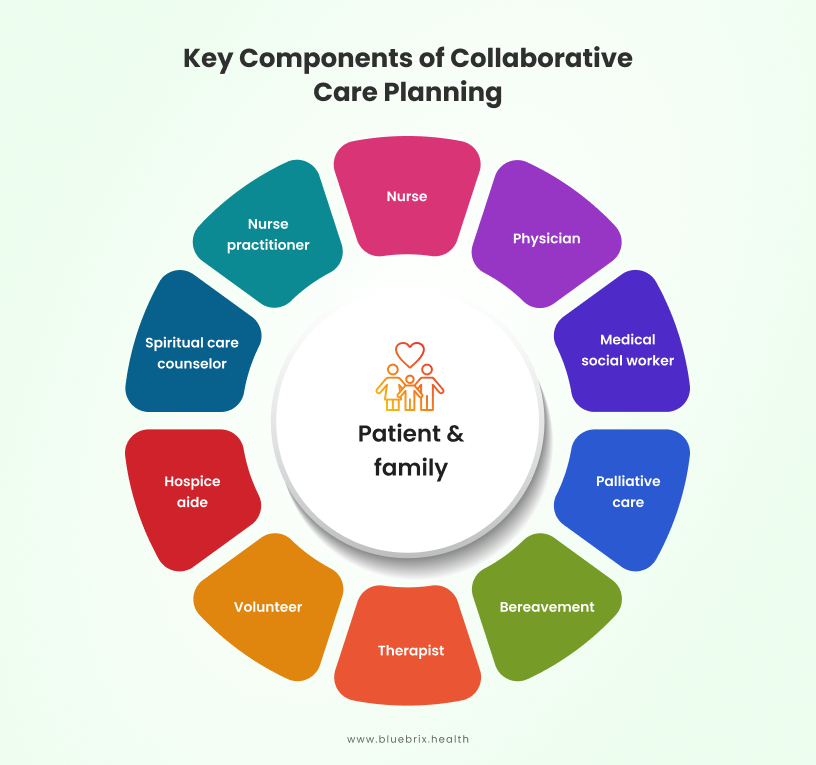
Team-based approach: Bringing everyone to the table
Healthcare isn’t a solo act. According to American Journal of Managed Care, patients with chronic conditions see an average of 16 different healthcare providers a year, yet without proper coordination, critical information can get lost in the shuffle. That’s why collaborative care planning relies on a structured, team-based approach—ensuring that every provider is on the same page. Collaborative care relies on a well-coordinated team that may include:
- Primary care providers – The main point of contact for overall health.
- Specialists – Experts in specific conditions (e.g., cardiologists, endocrinologists).
- Nurses & care coordinators – The glue that holds the care plan together.
- Mental health professionals – Address emotional and psychological well-being.
- Patients & caregivers – The most important members of the team!
And the impact? Studies show that team-based care can reduce hospital readmissions by 30% and improve chronic disease management by 40%.
For example, imagine a stroke survivor needing physical therapy, speech therapy, and mental health support. A coordinated team ensures each specialist shares updates in real time, preventing redundant tests and conflicting advice.
Shared decision-making: Empowering patients
A care plan is only effective if patients are actively involved. That’s why healthcare teams need to engage patients proactively—through education, shared decision-making, and transparent communication. Healthcare decisions should be made with the patient, not for the patient. Shared decision-making ensures that patients understand their options and actively participate in their care.
And the impact?
- Patients involved in decision-making are 20% more likely to stick to their treatment plans.
- Trust between patients and providers increases by 25% when shared decision-making is prioritized.
A patient with chronic back pain might have options like surgery, physical therapy, or medication. Instead of a doctor prescribing a default treatment, a collaborative care model presents the pros and cons of each, considering the patient’s lifestyle and preferences.
Data-driven care coordination
Without real-time data sharing, collaborative care falls apart. Electronic Health Records (EHRs) and interoperable care platforms ensure that every provider is on the same page.
And the impact?
Healthcare providers using EHR-integrated collaboration see a 20-25% reduction in medical errors.
Automated alerts for at-risk patients can reduce hospitalizations by 15%.
Example: A patient with heart failure sees both a cardiologist and a primary care doctor. With data-driven collaboration, their health data (blood pressure, medication adherence, lab results) is shared instantly, enabling proactive interventions before a crisis occurs.
Personalized & goal-oriented care plans
No two patients are the same, so cookie-cutter care plans don’t work. Instead, collaborative care creates individualized treatment strategies with clear goals.
And the impact?
- Patients with personalized care plans report 35% higher satisfaction.
- Tailored care plans improve medication adherence by 50%.
Example: A patient with diabetes and hypertension may need:
- A nutrition plan developed by a dietitian
- Medication monitoring by a pharmacist
- Regular check-ins via a telehealth app
By setting personalized goals (e.g., lowering A1C by 1% in 3 months), care teams can track and adjust the plan in real time.
Continuous monitoring & feedback loops
A care plan isn’t set in stone—it should evolve based on patient progress and real-time feedback. This requires remote monitoring tools, follow-ups, and patient-reported outcomes.
- Remote monitoring reduces hospital visits by 38%.
- AI-driven predictive analytics can identify high-risk patients 30% faster.
For example, a COPD patient using a smart inhaler gets alerts when usage patterns change, signaling a potential flare-up. The care team adjusts medication before the condition worsens—preventing ER visits.
Collaborative care planning isn’t just nice to have—it’s essential for better health outcomes, lower costs, and happier patients. Healthcare organizations embracing these five components are leading the way in value-based care, reducing unnecessary hospitalizations, and enhancing the patient experience.
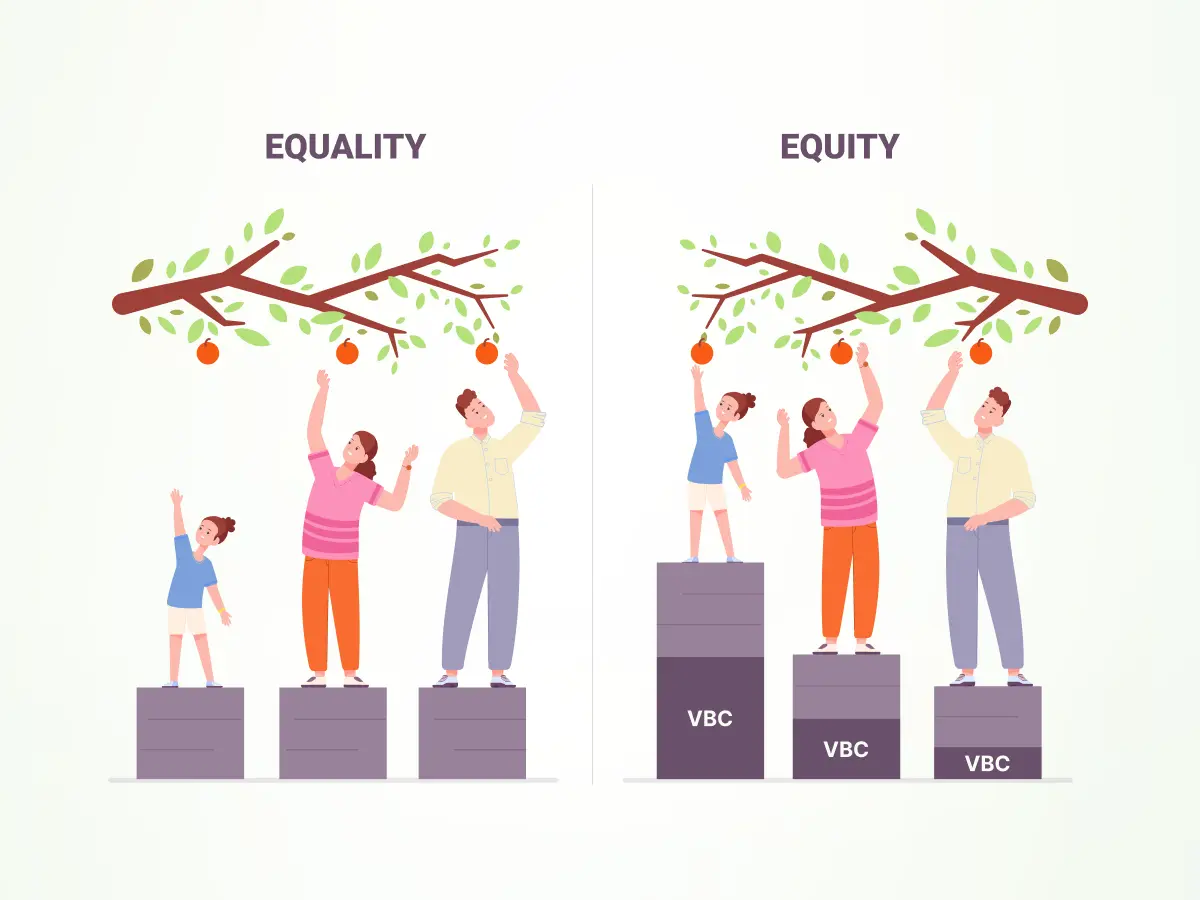
The patient’s side of collaborative care
Collaborative care planning involves tailoring treatment programs to each patient’s specific needs, considering not only clinical factors but also their personal preferences and social determinants of health (SDOH). By prioritizing both personalization and health equity, the approach ensures that care is well-rounded and relevant to the patient’s unique circumstances. Open communication fosters trust between patients and caregivers, empowering patients to feel more confident in the process.
From the patient’s perspective, collaborative care enhances empowerment by involving them in a coordinated, multidisciplinary team. This collaborative effort improves understanding and management of their treatment, supporting a two-way decision-making process that aligns with the patient’s goals and values. Such involvement reduces anxiety, encouraging patients to take a more active role in their care.
For example, setting specific, measurable, and time-bound goals for treatment, combined with ongoing, open communication between patients and caregivers, not only strengthens understanding but also promotes better health outcomes. Patients become active facilitators in their care, making informed decisions with greater independence and confidence.
The provider team collaboration
The effectiveness of collaborative care planning also relies on seamless coordination among diverse healthcare teams. A strong provider network and referral management system in place will help providers manage care coordination more efficiently. By fostering strong communication between specialists, primary care providers, and support staff, healthcare delivery becomes more holistic and patient centered. This alignment ensures that each team member understands the patient’s goals and treatment plan, leading to improved care continuity and better outcomes. When healthcare professionals work together in an integrated manner, they can provide more comprehensive, personalized care that addresses both clinical needs and patient preferences, ultimately enhancing the overall patient experience.
Social determinants of health (SDOH) in collaborative care

We have already discussed how health outcomes are significantly influenced by social determinants of health (SDOH) in our earlier write-ups. In collaborative care, the patient’s needs, wants and preferences are influenced by Social Determinants of Health. It is a part of the patient records which is used for charting out the treatment path in EHRs. With this, the patient data can be analyzed in real time and the healthcare teams can address clinical related factors as well as other social factors related to health and design effective treatments for them. Incorporating Social Determinants of Health into care planning leads to effective care management and better outcomes as providers will be able to address both clinical and social needs.
Measuring success in collaborative care planning: Key metrics to track
Implementing collaborative care planning is a significant step toward enhancing patient outcomes and optimizing healthcare delivery. But how do we know if it’s truly working? One way to assess success is through patient feedback, which provides direct insights into the patient’s experience, satisfaction, and areas for improvement. Feedback can be gathered via surveys, online ratings, or direct communication, allowing healthcare teams to refine care processes and foster a more engaging, personalized experience. Additionally, a data-driven approach to evaluate the effectiveness of care interventions is also key. By combining both feedback and outcomes, healthcare providers can create a holistic understanding of the impact of their collaborative care efforts. Let’s explore how to measure success in this approach, focusing on key performance indicators (KPIs) relevant to value-based care.
-
-
Patient Health Outcomes
Why It Matters: The primary goal of collaborative care is to improve patient health. Monitoring health outcomes provides direct insight into the effectiveness of care plans.
KPIs to Track:
- Readmission Rates: A lower rate indicates better initial treatment and effective follow-up care.
- Management of Chronic Diseases: Metrics like controlled blood pressure in hypertensive patients or stabilized blood sugar levels in diabetics reflect successful ongoing care.
-
Patient Engagement and Satisfaction
Why It Matters: Engaged and satisfied patients are more likely to adhere to treatment plans, leading to better health outcomes.
KPIs to Track:
- Patient Satisfaction Scores: Tools like the Net Promoter Score (NPS) measure patients’ willingness to recommend the service to others.
- Patient Activation Measures: Assessments that gauge a patient’s knowledge, skills, and confidence in managing their health.
-
Care Coordination Efficiency
Why It Matters: Effective coordination among healthcare providers ensures that patients receive comprehensive and timely care.
KPIs to Track:
- Referral Completion Rates: The percentage of patients who follow through with specialist referrals.
- Timeliness of Care Transitions: How quickly and smoothly patients move between different care settings or providers.
-
Preventive Care Compliance
Why It Matters: Preventive measures can reduce the incidence of diseases and associated healthcare costs.
KPIs to Track:
- Screening Rates: The percentage of eligible patients receiving recommended screenings (e.g., mammograms, colonoscopies).
- Vaccination Rates: Uptake of recommended vaccines among target populations.
-
Cost Management
Why It Matters: Efficient care reduces unnecessary expenses, benefiting both providers and patients.
KPIs to Track:
- Total Cost of Care per Patient: Monitoring overall expenses to identify areas for cost reduction.
- Emergency Department (ED) Visit Rates: High rates may indicate gaps in primary or preventive care.
-
Provider Engagement and Well-being
Why It Matters: Engaged and satisfied healthcare providers are crucial for delivering high-quality care.
KPIs to Track:
- Provider Satisfaction Surveys: Assessing job satisfaction and identifying areas for improvement.
- Burnout Rates: Monitoring signs of burnout to implement supportive measures timely.
-
By diligently tracking these KPIs, healthcare organizations can assess the effectiveness of their collaborative care planning efforts, make informed adjustments, and ultimately achieve better patient outcomes in a value-based care environment. Our earlier published blog gives you more detailed information on key metrices.
How does blueBriX value-based care solutions support collaborative care planning?
Effective collaborative care hinges on smooth coordination, open communication, and efficient data sharing among healthcare providers, patients, and support staff. The blueBriX Collaborative Care Planning Toolkit offers a comprehensive suite of tools designed to facilitate multi-professional care, boost patient engagement, and monitor health outcomes. Let’s delve into the key features of this toolkit and see how it’s transforming patient-centered care.
Coordinated, multi-professional care management
In a healthcare ecosystem where doctors, nurses, and specialists can easily share and access patient information, everyone is on the same page, leading to efficient and effective care. But it’s not just about the internal team; working hand-in-hand with external partners—like those providing food, shelter, transportation, and rehabilitation services—is crucial for comprehensive patient support, especially in value-based care.
To make treatments more effective, it’s important to create specific care plans tailored to different patient groups. Whether it’s managing chronic illnesses or addressing social factors affecting health, each group gets the attention they need. Secure messaging and information sharing are vital here, protecting patient privacy while keeping communication smooth between healthcare providers and external partners. Real-time access to essential information is key to better coordination and patient outcomes.
Enter blueBriX—a platform designed to streamline all your care collaboration needs. Here’s how blueBriX enhances care coordination:
- Integrated electronic health records: blueBriX allows healthcare providers to easily share and access up-to-date patient records, ensuring everyone has the latest information.
- Clinical workflow management: Customize workflows for specific patient groups, keeping the care team aligned and processes efficient.
- Telemedicine capabilities: blueBriX supports remote consultations and team discussions, breaking down geographical barriers to continuous care.
- Medical device integration: Integrate data from various clinical devices in real-time, aiding in monitoring and quick decision-making.
- Clinical decision-making tools: Access evidence-based tools within blueBriX to make informed decisions swiftly.
- Referral management: Simplify patient referrals to specialists or other services, ensuring smooth transitions and follow-ups.
- Cloud infrastructure & interoperability: With cloud-based solutions, blueBriX ensures consistent and accessible data across platforms and devices.
- Coordinated care planning: Develop personalized treatment plans, facilitate seamless team collaboration, and provide real-time updates through device integration and insights into social determinants of health.
By bringing these features together, blueBriX promotes comprehensive and well-coordinated care, leading to better patient outcomes.
Proactive patient engagement & communication
Engaging patients is crucial for successful collaborative care. blueBriX enhances patient-provider communication through real-time monitoring and feedback, encouraging active patient participation in health management. Key features include:
- Integrated medical device connectivity: Continuous monitoring and feedback are enabled through connected medical devices, fostering proactive communication between patients and providers.
- Remote patient monitoring: Ongoing engagement with patients is facilitated by tracking their health metrics remotely, helping healthcare teams stay on top of patient conditions.
- Telemedicine features: Patients can access care conveniently through virtual visits, enhancing communication and access to healthcare professionals when needed.
- Automated scheduling: Efficient scheduling tools make it easier for patients to book appointments and receive reminders, ensuring timely care.
- Consent management: Obtaining patient consent is a critical step in collaborative care. blueBriX simplifies this process with digital consent management tools that allow patients to review and sign consent forms electronically, ensuring compliance and building trust.
- Intake forms: Electronic intake forms streamline the initial patient data collection process, reducing administrative workload and ensuring providers have accurate information for effective diagnosis and treatment planning.
- Self-management tools: blueBriX offers tools like the Diabetic Patient Companion App and Telemedicine Apps, empowering patients to manage their conditions and engage in their care journey.
- Medical record access: Providers can view comprehensive patient information, ensuring all healthcare professionals involved are aligned regarding medical history, current medications, and treatment plans.
- Personalized patient education & communication: blueBriX provides customized educational resources based on specific health conditions and treatment plans, empowering patients with the knowledge to manage their care.
- Specialized apps: blueBriX offers personalized apps that provide easy access to treatment information, helping patients stay on top of their care pathways.
By integrating these features, blueBriX fosters a patient-centered approach, enhancing engagement and improving healthcare delivery.
Outcome tracking and monitoring
Keeping track of patient outcomes is vital in collaborative care to ensure treatments are working and to make necessary adjustments. blueBriX offers a range of tools to monitor patient engagement and health metrics effectively.
Adherence and engagement monitoring: blueBriX tracks how well patients follow their treatment plans, providing insights into their engagement levels.
Remote monitoring capabilities: By continuously observing health metrics like blood pressure and glucose levels, healthcare teams can detect changes and intervene promptly.
Vitals and symptoms monitoring: blueBriX enables real-time tracking of critical health parameters, offering immediate insights into patient conditions.
Clinical data visualization tools: These tools help healthcare teams visualize patient progress and outcomes, facilitating data-driven decisions.
Wearables integration: Data from wearable devices seamlessly integrates into the blueBriX platform, enhancing accurate health monitoring and patient management.
Custom dashboards: blueBriX allows the creation of customizable applications to boost patient engagement. Features include reminders, user-friendly patient portals for managing health information, and customizable app templates, all designed to improve patient interaction and adherence to care plans.
The blueBriX Collaborative Care Planning Toolkit provides the technological foundation needed to enhance patient outcomes, boost engagement, and streamline care processes. What sets us apart from other technology vendors is that you can create your unique care pathways using blueBriX.
The future of collaborative care
As healthcare decision-makers, you’re navigating the shift toward value-based care—a model that rewards quality over quantity.Central to this evolution is collaborative care, where technology plays a pivotal role in enhancing patient outcomes and operational efficiency.
Artificial intelligence (AI): Transforming collaborative care
AI is significantly impacting healthcare by automating tasks and providing actionable insights. For instance, AI can analyze vast amounts of patient data to identify patterns, predict health risks, and suggest personalized treatment plans. A recent study demonstrated that AI-generated post-operative reports were more accurate than those written by surgeons, reducing discrepancies and enhancing patient safety.
Remote patient monitoring (RPM): Extending care beyond clinics
Remote patient monitoring technologies enable continuous monitoring of patients’ health metrics, such as blood pressure and glucose levels, from their homes. This proactive approach allows healthcare teams to detect changes early and intervene promptly, reducing hospital admissions and improving patient satisfaction. The integration of wearables and mobile health apps has further empowered patients to engage actively in their health management.
Telemedicine: Bridging gaps in access to care
Telemedicine has become a cornerstone of modern healthcare, especially in value-based models. It facilitates virtual consultations, making healthcare more accessible and convenient. This technology not only reduces the burden on physical healthcare facilities but also ensures that patients receive timely care, regardless of their location.
Data integration and interoperability: Building a cohesive care network
Seamless data exchange is crucial for effective collaborative care. Interoperable systems allow healthcare providers to access comprehensive patient data, leading to informed decision-making and coordinated care plans. Efforts are underway to standardize data-sharing practices, enhancing the efficiency of value-based care models.
Virtual wards: Hospital-level care at home
Virtual wards represent an innovative approach, allowing patients to receive hospital-level treatment in the comfort of their homes. This model leverages technology to monitor patients remotely, reducing the strain on hospital resources and improving patient satisfaction. During the COVID-19 pandemic, virtual wards were instrumental in managing patient care, demonstrating their potential in the broader healthcare landscape.
The path forward
Embracing these technological advancements is essential for healthcare organizations aiming to thrive in a value-based care environment. Investing in AI-driven tools, RPM, telemedicine, and interoperable systems will enhance care coordination, improve patient outcomes, and optimize operational efficiency. As decision-makers, your leadership in adopting these innovations will be pivotal in shaping the future of collaborative, value-based healthcare.