Picture this: You’re a CFO watching your organization’s financial performance, and despite delivering excellent patient care, your revenue keeps falling short of projections. Your practice managers are working overtime, your clinical staff is performing admirably, yet somewhere in the complex maze of value-based care contracts, millions of dollars are simply vanishing into thin air. Welcome to what we call “The VBC Black Hole” – a phenomenon draining healthcare organizations across America of rightfully earned revenue.
If you’re feeling the financial squeeze, you’re not alone. Recent industry data reveals that healthcare organizations are hemorrhaging revenue at an unprecedented rate, with 40% of providers losing more than 10% of their annual revenue to leakage, and some losing over 20%. The culprit? A perfect storm of inaccurate HCC coding, inefficient care coordination, and fragmented systems that create revenue gaps large enough to drive your CFO to sleepless nights.

The revenue hemorrhage crisis: what independent data shows
Let’s examine the hard numbers from authoritative sources that should concern every CFO.
- Government data on denial patterns: According to CMS data and independent healthcare research organizations, Medicare Advantage has significantly higher administrative complexity and denial rates compared to traditional Medicare. The Medicare Payment Advisory Commission (MedPAC) has documented these growing challenges in their official reports to Congress.
- Academic research findings: Research published in peer-reviewed healthcare journals indicates that medical coding errors represent a substantial source of revenue leakage across the industry. Studies from major academic medical centers consistently identify documentation and coding gaps as primary drivers of lost revenue.
- Industry analyst reports: Major consulting firms like McKinsey have documented the growing challenges in Medicare Advantage revenue optimization, noting that health systems struggle with the complexity of risk adjustment and value-based care requirements.
- Healthcare executive survey data: Independent surveys of healthcare CFOs and financial executives consistently show that revenue leakage is a top concern, with organizations reporting significant challenges in capturing appropriate reimbursement for the complexity of care they deliver.
- CMS performance data: Official CMS reports show wide variation in risk adjustment performance across healthcare organizations, indicating that many providers are not optimizing their revenue capture in value-based care arrangements.
- The documentation challenge: Healthcare industry associations consistently report that inadequate clinical documentation and care coordination represent major barriers to appropriate reimbursement, particularly in complex chronic disease management scenarios.
These findings paint a clear picture: healthcare organizations across the country are struggling with revenue optimization challenges, particularly in the evolving value-based care landscape where proper documentation and care coordination directly impact financial performance.
The hidden costs that CFOs miss
Revenue leakage isn’t just about the obvious denied claims. It’s the insidious collection of inefficiencies that compound over time:
- Administrative burden explosion: Healthcare organizations paid an estimated $25.7 billion for claims adjudication in 2023, with Medicare Advantage appeals representing a disproportionate share of these costs. The average cost of appealing one Medicare Advantage denial? A staggering $63.76, compared to just $0.79 for traditional Medicare.
- Cash flow strangulation: Reimbursement delays are driving liquidity crises industry-wide. Hospitals had 196.8 days in cash available on hand in 2023 – a 10-year low, directly related to increased payment lag due to growing appeal cycles.
- The documentation gap: Studies show that 25-30% of medical practice income disappears due to wrong coding, underpricing, and poor follow-up. Primary care physicians alone lose close to a quarter million annually when they fail to bill for preventive and coordination services.
Real-world examples: how HCC revenue vanishes and gets recovered
Let’s examine concrete examples of how HCC-related revenue disappears and the massive financial impact on organizations:
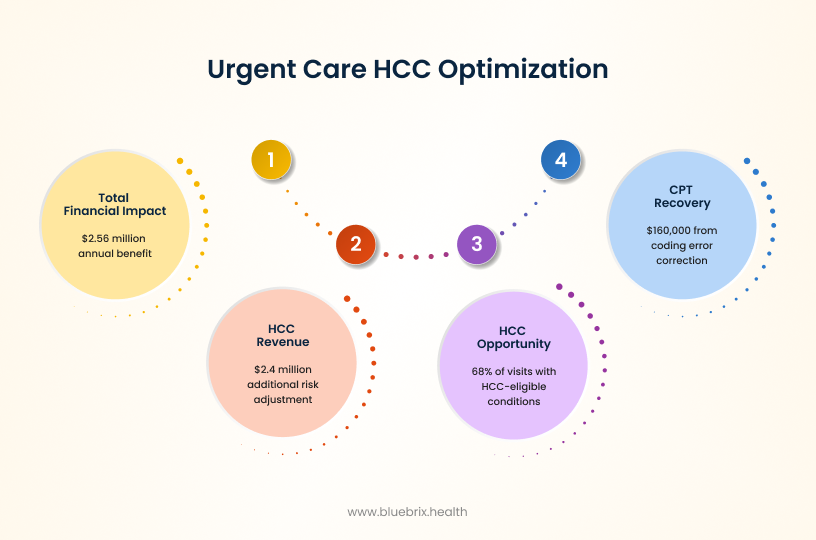
Use case 1: The urgent care HCC goldmine – $160,000 recovery plus hidden HCC millions
- Organization: Multi-state urgent care network with 290 providers across 7 states
- Challenge: Systematic revenue leakage from coding errors masking massive HCC opportunities
- Timeline: 3-month initial recovery, 12-month HCC optimization
The Problem:
This urgent care organization initially discovered that a single CPT code error was costing them hundreds of thousands in revenue. However, the deeper analysis revealed something far more significant: urgent care settings are HCC goldmines because they see patients with acute exacerbations of chronic conditions, but these valuable diagnosis opportunities were going completely undocumented.
The HCC discovery:
- Initial CPT recovery: $160,000 in the first three months from correcting the coding error.
- The real problem: Urgent care visits were capturing acute symptoms but missing the underlying chronic conditions that drive HCC revenue.
- Hidden HCC opportunity: Analysis revealed that 68% of visits involved patients with diabetes, COPD, cardiovascular disease, or other HCC-eligible conditions.
The HCC revenue multiplier:
When the organization implemented integrated HCC documentation workflows:
- Immediate HCC capture: $2.4 million in additional annual risk adjustment revenue
- Per-Patient impact: Average risk score increased from 0.85 to 1.12 per patient
- Documentation improvement: HCC-eligible diagnoses captured increased by 340%
The Care coordination connection:
The breakthrough came when they integrated care coordination alerts that prompted providers to:
- Document chronic conditions during acute visits
- Capture medication reconciliation HCC opportunities
- Link urgent care findings to ongoing chronic disease management
- Generate proper referrals that maintained HCC continuity
Total financial impact: $160,000 CPT recovery + $2.4M annual HCC revenue = $2.56 million total annual impact.
Use case 2: Radiology’s hidden HCC goldmine – $1.1 million discovery reveals $4.2 million HCC gap
- Organization: Radiology Imaging Associates – Regional radiology practice
- Challenge: Payer underpayments masking systematic HCC documentation failures
- Discovery method: Healthcare contract management software revealing HCC gaps
The surface problem:
Radiology Imaging Associates discovered $1.1 million in systematic underpayments from a major payer. But the contract management analysis uncovered something bigger: radiology reports are HCC treasure troves that were being completely ignored for revenue optimization.
The HCC reality:
- Radiology findings often confirm chronic conditions but weren’t triggering proper HCC documentation.
- Diabetic complications, cardiovascular disease, chronic kidney disease were visible in imaging but not captured for risk adjustment.
- Secondary diagnosis opportunities were systematically missed.
The HCC revenue recovery process:
Phase 1: Systematic review of radiology findings vs. HCC documentation
- Found that 78% of studies showed evidence of chronic conditions
- Only 23% of these chronic conditions were being captured as HCC codes
- Average of 2.3 HCC opportunities per study were being missed
Phase 2: Implementation of structured HCC reporting
- Radiologists trained to flag HCC-eligible findings
- EHR integration to prompt referring physicians about HCC opportunities
- Care coordination alerts when imaging confirms chronic conditions
The HCC financial recovery:
- Original underpayment recovery: $1.1 million from payer corrections
- HCC revenue recovery: $4.2 million annually from improved chronic disease documentation
- Risk score impact: Average patient risk scores increased by 0.28 points
- Care coordination revenue: Additional $800,000 from improved referral documentation
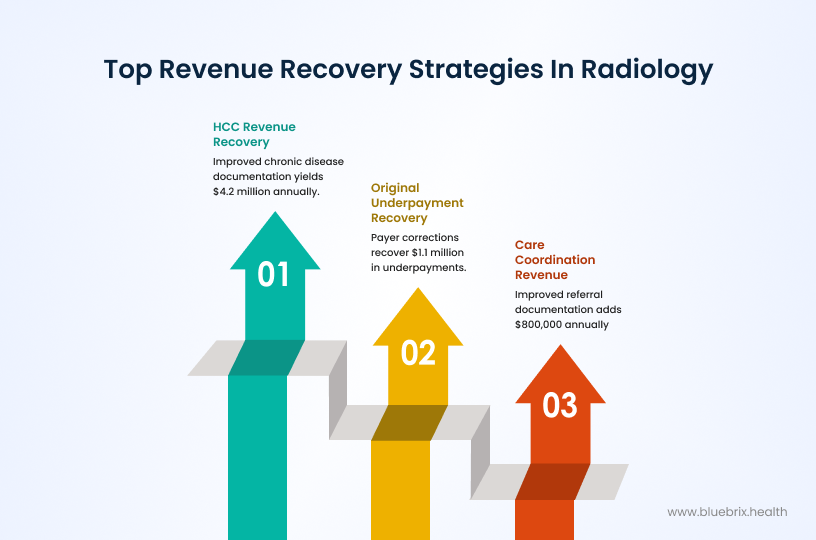
Key insight: Radiology practices are sitting on HCC gold mines – every imaging study that shows chronic disease complications should trigger risk adjustment revenue, but most organizations never make this connection.
Use case 3: The systematic HCC transformation – 12% performance improvement worth $3.25 million
- Organization: Regional Accountable Care Organization (ACO) with 45,000 covered lives
- Challenge: 10% decline in HCC recapture rates threatening VBC contract performance
- Solution: Comprehensive care coordination platform with integrated HCC optimization
The critical challenge:
This ACO was facing financial crisis as CMS model changes resulted in a 10% decline in their HCC recapture rates. With value-based care contracts representing 60% of their revenue, this decline threatened their survival in VBC arrangements.
The comprehensive HCC strategy:
Technology integration (Months 1-3):
- Implementation of AI-driven HCC opportunity identification
- Real-time care coordination workflows with embedded HCC prompts
- Predictive analytics for prospective chronic disease management
Care coordination optimization (Months 4-8):
- Systematic care gap closure with HCC documentation requirements
- Medication reconciliation protocols that capture treated conditions
- Care management visits designed to maximize HCC capture opportunities
Provider education and workflow integration (Months 9-12):
- Point-of-care HCC alerts during patient encounters
- Documentation improvement training focused on chronic disease specificity
- Care coordination protocols that create multiple HCC touch points per patient
The HCC performance results:
- HCC recapture rate: 12% improvement over baseline (from 78% to 87.4%)
- Average risk scores: 2.5% improvement across patient population
- Care coordination impact: 89% of chronic disease patients had documented care coordination encounters
- Documentation quality: 35% increase in diagnosis specificity and chronic disease complexity capture
The financial transformation:
- Annual Risk Adjustment Revenue: $3.25 million increase
- Quality Bonus Improvements: Additional $450,000 in performance-based payments
- Care Coordination Fees: $680,000 in additional care management revenue
- Total Annual Impact: $4.38 million in recovered and new revenue
The care coordination multiplier effect:
The key breakthrough was recognizing that care coordination visits are HCC revenue opportunities:
- Each care coordination encounter generated an average of 1.8 additional HCC codes
- Comprehensive health assessments revealed previously undocumented conditions
- Care transitions management ensured HCC continuity across settings
- Population health management identified and closed systematic HCC gaps
Sustainability results:
- Year 2 performance: 14.5% improvement in HCC recapture (continued growth)
- Provider engagement: 94% of providers actively using integrated HCC workflows
- Process integration: HCC optimization became standard care coordination practice
The unified HCC revenue recovery theme
All three cases reveal the same fundamental truth: Healthcare organizations are hemorrhaging HCC revenue because their care coordination and clinical documentation systems aren’t designed for value-based care optimization.
The pattern across all cases
- Surface problem: Obvious revenue leaks (coding errors, payer underpayments, declining performance)
- Hidden reality: Massive HCC documentation and capture failures
- Root cause: Lack of integrated care coordination that connects clinical activities to revenue optimization
- Solution: Systematic care coordination platforms that embed HCC optimization into clinical workflows
The root cause: fragmented care coordination
Here’s what most CFOs and practice managers don’t realize: The revenue leakage problem isn’t just about coding errors or claim denials. It’s fundamentally about fragmented care coordination that prevents accurate capture of patient complexity and clinical activities.
Traditional healthcare systems operate in silos. Your EHR talks to your practice management system, which talks to your billing platform, but none of them effectively communicate with your care coordination processes. The result? Critical patient conditions go undocumented, care gaps remain unclosed, and risk adjustment opportunities slip through the cracks.
Consider the typical scenario: A patient with multiple chronic conditions receives care from various providers within your network. Each interaction generates valuable HCC-eligible diagnoses, but without integrated care coordination:
- Documentation inconsistencies across providers lead to missed HCC opportunities
- Care gaps remain unidentified until it’s too late for intervention
- Risk stratification relies on incomplete data, underestimating patient complexity
- Quality measures suffer due to poor care coordination, impacting bonus payments
The blueBriX solution: plugging the revenue leak
This is where blueBriX’s care coordination orchestration platform transforms the revenue equation. Unlike traditional solutions that treat symptoms, blueBriX addresses the root cause of revenue leakage by creating a unified ecosystem where clinical care, documentation, and revenue optimization work in perfect harmony.
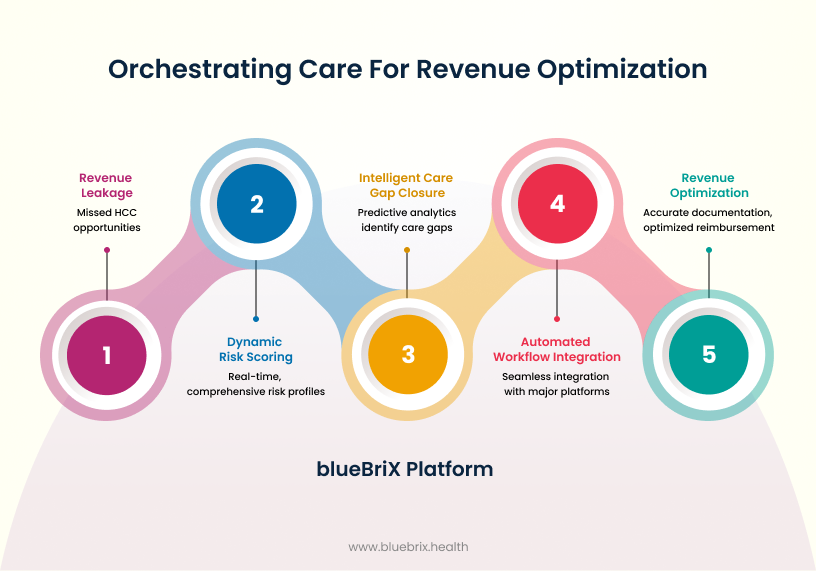
Dynamic risk scoring and prioritization
blueBriX combines EHR data, claims information, social determinants, and behavioral data to create real-time, comprehensive risk profiles. This enables your teams to:
- Identify high-value HCC opportunities before they’re missed
- Prioritize patients based on both clinical needs and revenue potential
- Ensure accurate documentation that reflects true patient complexity
Intelligent care gap closure
The platform’s predictive analytics identify care gaps, hospitalization risks, and overdue tasks before they become crises. More importantly, it ensures these interventions are properly documented and coded, turning clinical excellence into revenue optimization.
Automated workflow integration
blueBriX integrates seamlessly with Epic, Salesforce, athenahealth, and other major platforms without disrupting existing workflows. This means your providers can focus on patient care while the system automatically:
- Captures HCC-eligible diagnoses
- Ensures proper documentation specificity
- Tracks quality measures and compliance requirements
- Optimizes reimbursement through accurate coding guidance
Quantifying the ROI: real numbers for CFOs
Let’s translate this into language every CFO understands – return on investment:
- Immediate revenue recovery: Organizations implementing comprehensive care coordination platforms typically see revenue improvements of 8-15% within the first year. For a $50 million annual revenue organization, that’s $4-7.5 million in recovered revenue.
- Reduced administrative costs: By automating workflows and reducing claim denials, organizations can reduce administrative overhead by 20-30%, freeing up resources for patient care and growth initiatives.
- Improved contract performance: Enhanced care coordination leads to better performance on value-based care contracts, with organizations reporting 10-25% improvements in shared savings and quality bonus payments.
- Use case validation: Our three detailed examples above show combined revenue recovery of $10.34 million annually across organizations of different sizes and specialties.
Implementation strategy for practice managers
For practice managers ready to tackle revenue leakage, here’s a strategic approach:
Phase 1: Assessment and integration
- Conduct comprehensive revenue cycle analysis to identify specific leak sources
- Implement blueBriX’s care coordination platform with existing EHR systems
- Train staff on integrated workflows that capture clinical and financial data simultaneously
Phase 2: Process optimization
- Establish real-time monitoring of HCC opportunities and care gaps
- Create automated workflows for documentation improvement and coding accuracy
- Implement patient engagement tools that support both clinical outcomes and revenue capture
Phase 3: Performance management
- Track key performance indicators including RAF scores, care gap closure rates, and revenue per patient
- Use predictive analytics to identify at-risk revenue opportunities
- Continuously optimize based on data-driven insights