Medical coding is a clear example of how administrative inefficiencies drive up healthcare costs. For behavioral health practices, inaccurate or inconsistent coding can lead to backlogs and denied claims, adding strain to already busy teams. The result? Slower reimbursements, longer days in A/R, and increased write-offs—all of which can quietly chip away at revenue.
Just as patient care requires individual attention, coding behavioral health records demands careful, accurate documentation tailored to each case. When coding isn’t done right, the consequences can include denied claims, delayed payments, and even repayment demands. Providers and RCM teams who understand these risks are in a better position to avoid common mistakes and improve claim success rates.
By addressing common coding issues upfront, your team can support smoother claim submissions, reduce financial stress, and help maintain the long-term financial health of your practice.
The critical role of accurate coding in behavioral health
Unlike other specialties, behavioral health services often involve nuanced diagnoses, evolving treatment plans, and diverse therapy formats. Coding errors here don’t just delay payments—they risk misrepresenting patient needs, disrupting continuity of care, and creating compliance gaps. From maintaining financial viability to improving patient outcomes and meeting regulatory demands, accurate coding is essential to every aspect of behavioral health operations. The sections below break down the key areas where precision in coding makes a measurable difference.
Ensuring proper reimbursement and financial viability
Accurate coding is central to financial health in behavioral settings. When ICD-10-CM and CPT codes are applied correctly, claims move through the system smoothly, reducing denials and minimizing revenue loss. Given the diversity of services—like individual, group, or family therapy—precise coding ensures providers are reimbursed appropriately for the type and duration of care delivered.
Maintaining regulatory compliance and reducing legal risk
Behavioral health coding must meet federal and state regulatory standards, including HIPAA. Thorough documentation and correct coding support medical necessity and payer requirements. Errors can lead to audits, claim rejections, or reputational issues—all of which drain time and resources. Strong coding practices help avoid these pitfalls and keep operations on track.
Enhancing quality of patient care
Accurate coding drives better documentation, which in turn supports care coordination, treatment planning, and clinical decision-making. When records clearly reflect a patient’s condition and progress, it strengthens continuity of care and enables better outcomes. It also supports integrated care models where behavioral health and medical services work in tandem.
Supporting data-driven decision making and healthcare management
Reliable coding data powers insights into utilization, outcomes, and resource needs. This is critical for audits, quality improvement, and strategic planning. It also ensures providers meet mental health parity standards, reinforcing equal access to behavioral health services.
Top 6 common coding mistakes in behavioral health
Here are the top 6 behavioral health coding mistakes and practical tips to help your team avoid them—so you can get paid accurately, stay compliant, and focus on what matters most: patient care.
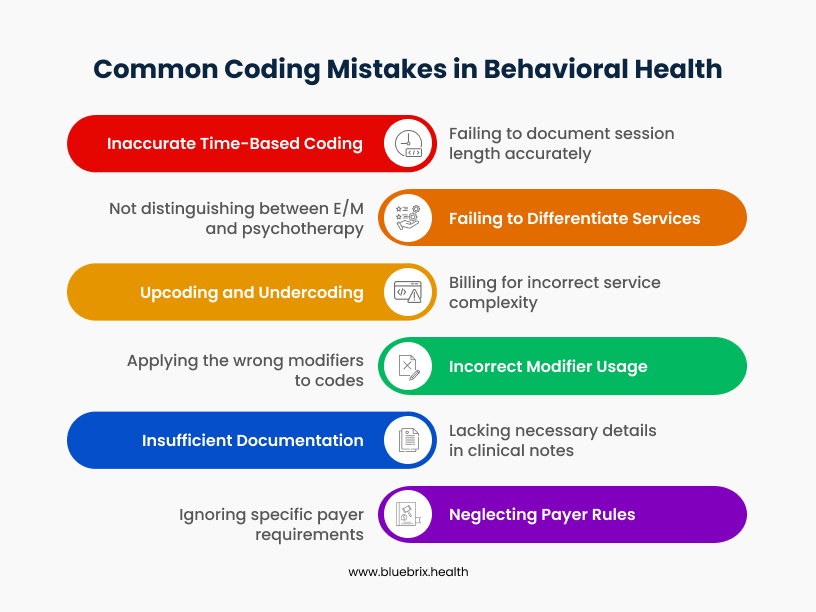
Mistake 1: inaccurate time-based coding and documentation
Many behavioral health services, particularly psychotherapy, are billed based on the precise duration of time spent directly with the patient. Inaccurate time-based coding and documentation occurs when a provider fails to meticulously document the exact session length, rounds up session times improperly, or selects a billing code that simply doesn’t match the actual time rendered.
Common examples of inaccuracy
- Avoiding misuse in initial evaluations: CPT codes 90791 and 90792 are used for initial psychiatric evaluations and should only be billed when conducting a comprehensive assessment of a patient’s mental status, history, and treatment needs. 90791 is for non-medical providers, while 90792 includes medical services and is limited to psychiatrists or qualified medical professionals. Though typically lasting around 60 minutes, there’s no fixed time requirement—but documentation must justify the complexity. Using these codes for routine visits or without proper documentation can result in denials or audits.
- Rounding up session times: A common error is rounding up when the documented time doesn’t meet the threshold for a higher-level CPT code. For example, if a session lasts 37 minutes, billing 90834 (which requires at least 38 minutes) instead of the correct 90832 would be inaccurate and may be flagged as upcoding.
- Failing to record exact start and stop times: Simply noting “45-minute session” in documentation, without providing explicit start and end times (e.g., “Session began at 10:00 AM and concluded at 10:45 AM”), creates a documentation gap that can lead to errors and compliance vulnerabilities.
- Selecting codes without supporting documentation: Choosing a CPT code based on its minimum time requirement yet lacking clear documentation that this time was actually spent directly with the patient on billable services, is a significant red flag.
- Including non-billable time: Providers sometimes mistakenly include time spent on activities that are not billable under a psychotherapy code, such as administrative tasks, scheduling, or unrelated casual conversation, in the total session duration.
Best practices to avoid this mistake
- Document exact start and stop times: Always record the precise minute a session begins and the exact minute it concludes, rather than just the total duration. This provides irrefutable evidence for the billed time.
- Match code to actual time: Always select the CPT code that aligns with the documented session duration. For example, to bill 90834 (psychotherapy, 45 minutes), at least 38 minutes of face-to-face psychotherapy must be provided and documented. Similarly, 90837 (60-minute session) requires at least 53 minutes. Be sure to exclude non-billable time (e.g., scheduling, casual conversation) and clearly document start/end times and therapeutic interventions.
- Detail clinical content: Beyond just time, include a concise but comprehensive summary of the clinical interventions performed and the content discussed during the session. This narrative helps justify the time billed and demonstrates medical necessity.
- Separate notes for multiple services: If a patient receives both medication management and psychotherapy during the same visit, document the time spent on each service separately. Crucially, do not double-count time for both services.
Mistake 2: failing to differentiate between E/M and psychotherapy services (and improper use of add-on codes)
When a patient visit includes both medical management (E/M) and structured therapeutic interventions (psychotherapy), it’s crucial for billing accuracy that these two distinct service types are clearly differentiated in the documentation and coding. Without this separation, payers often assume that psychotherapy is implicitly included within the E/M service, leading to denied reimbursement for the psychotherapy itself.
Common mistakes
- Undocumented separation: Failing to document the medical management and psychotherapy portions as distinct activities within the clinical note.
- Incorrect standalone use: Using only a standalone psychotherapy code (e.g., 90832, 90834, 90837) when an E/M service was also performed, or conversely, only billing an E/M code when psychotherapy was also delivered.
- Neglecting add-on codes: Failing to append the correct psychotherapy add-on code when psychotherapy is delivered alongside an E/M service.
These errors lead to the payer’s assumption that the psychotherapy was part of the E/M, resulting in denial of the psychotherapy claim.
How to avoid failing to differentiate between E/M and psychotherapy services
Preventing this common behavioral health coding mistake requires deliberate effort and structured practices.
- Clearly document both services separately – Within your progress notes, create distinct sections or clear delineations for the medical Evaluation and Management (E/M) activities (e.g., medication review, symptom assessment, treatment plan adjustments) and the specific psychotherapy interventions (e.g., use of CBT techniques, motivational interviewing, psychoeducation) provided during the same encounter.
- Select E/M codes based on medical decision making (MDM) – A critical point: when billing an E/M service with a psychotherapy add-on, the E/M code must be chosen based on the complexity of the medical decision making involved, not on the total time spent.
- Document time accurately and separately – For the psychotherapy add-on codes, precisely record the exact time dedicated solely to psychotherapy, keeping it separate from the time spent on E/M services.
- Apply modifier 25 when required – When a significant, separately identifiable E/M service is performed on the same day as psychotherapy, always append Modifier 25 to the E/M code. This modifier signals to the payer that the E/M service was distinct and warranted, separate from the psychotherapy provided.
Mistake 3: upcoding and undercoding
Upcoding occurs when a behavioral health provider assigns a higher-level, more complex, or more expensive CPT (Current Procedural Terminology) code than what the documented services actually support.
Common examples of upcoding in behavioral health:
- Time-based service mismatch: A therapist might conduct a standard 30-minute psychotherapy session but erroneously bill for a 60-minute session (e.g., using CPT 90837 instead of 90834 or 90832).
- Exaggerated evaluation: Billing for a comprehensive psychiatric diagnostic evaluation when only a limited or follow-up assessment was genuinely performed.
Conversely, undercoding happens when a behavioral health provider bills for a less complex or lower-level service than what was actually delivered and documented.
Common examples of undercoding in behavioral health:
- Underbilling session time: A provider performs a full 60-minute therapy session but, due to oversight or a conservative approach, bills for only 30 minutes. Similarly, some sessions may legitimately exceed 60 minutes, particularly for complex cases or crisis interventions. Failing to use add-on codes (e.g., 99354 for prolonged services) when applicable means the provider isn’t fully compensated for their time and effort.
- Omitting additional services: Failing to bill for all legitimate, separately billable services provided during a session, such as brief interventions or specific assessments.
How to prevent upcoding and undercoding?
Proactive measures are essential to mitigate these pervasive coding errors:
- Regular training and education: Implement continuous, mandatory training programs for all clinical and billing staff on the latest coding standards, modifier usage, and documentation requirements specific to behavioral health.
- Thorough and accurate clinical documentation: Emphasize the importance of clear, concise, and comprehensive documentation that precisely reflects the services rendered, the patient’s condition, and the medical necessity.
- Routine internal audits: Conduct regular internal audits of your coding practices to proactively identify and correct upcoding or undercoding errors before they lead to external scrutiny or denials.
- Leverage electronic health records (EHR) with built-in checks: Utilize EHR systems that offer integrated coding assistance, claim scrubbing features, and alerts for potential coding discrepancies, which can significantly reduce human error.
Mistake 4: incorrect modifier usage
Incorrect modifier usage is a remarkably frequent and costly error within behavioral health coding. This seemingly minor oversight often precipitates claim denials, leads to delayed payments, heightens compliance risks, and ultimately results in significant lost revenue for practices.
Common scenarios of incorrect modifier usage
Misapplication of modifiers can occur in several ways, often leading to billing complications:
- Using the wrong modifier: This happens when an incorrect modifier is appended to a code. For example, applying a telehealth modifier (like 95) to an in-person session, or using a license-level modifier that does not accurately reflect the credentials of the rendering provider.
- Omitting necessary modifiers: A critical error is simply forgetting to append a required modifier. A common instance in behavioral health is failing to use Modifier 25 when a significant, separately identifiable Evaluation and Management (E/M) service is performed on the same day as psychotherapy. Such omissions almost always lead to claim denials or underpayment.
- Overusing or misusing modifier 59: Modifier 59 is specifically designed to indicate a “distinct procedural service.” However, it is frequently misused when a more specific and appropriate modifier should have been applied, or when the services billed are not, in fact, truly distinct as defined by coding guidelines.
- Inconsistent modifier use: Applying modifiers inconsistently across similar types of claims or encounters can raise red flags with payers, often triggering audits and subsequent denials.
Best practices to avoid incorrect modifier usage
Mitigating modifier errors requires a proactive and systematic approach:
- Regular training and education: Ensure all staff involved in coding and billing receive continuous, up-to-date training specifically on modifier rules, their appropriate application, and payer-specific policies related to modifiers in behavioral health.
- Leverage electronic health record (EHR) systems with built-in assistance: Utilize modern EHR systems like blueBriX that offer integrated coding assistance, claim scrubbing features, and real-time alerts for potential modifier errors. These tools can significantly reduce manual mistakes.
- Conduct regular audits: Implement routine internal audits specifically focused on claims involving modifiers. This proactive review helps identify patterns of error and allows for corrective action before major issues arise.
Mistake 5: insufficient or inaccurate documentation
Insufficient or inaccurate documentation is another costly mistake in behavioral health coding. This critical error occurs when clinical notes and patient records fail to fully or correctly capture the essential details of a patient encounter, which is absolutely fundamental for accurate coding, appropriate billing, and proper reimbursement.
How documentation mistakes occur
Documentation errors in behavioral health can stem from various sources:
- Missing required elements: Notes may lack critical details specifically mandated for behavioral health services, such as precise start and stop times for psychotherapy sessions, confirmation of patient consent for telehealth, results of mental status exams, or clear identification of the specific service provided (e.g., individual versus group therapy).
- Vague or incomplete descriptions: Providers sometimes use ambiguous language or do not describe the patient’s symptoms, diagnosis, treatment interventions, or progress with sufficient specificity. This lack of detail makes it challenging for coders to assign the most accurate codes.
- Inconsistent documentation practices: Within an organization, different clinicians may employ varying methods or levels of detail in their notes. This inconsistency results in fragmented or incomplete patient records and is particularly problematic in practices that lack standardized documentation processes.
Best practices to avoid documentation mistakes
To ensure robust and accurate documentation, behavioral health providers should adopt the following best practices:
- Follow payer and CMS guidelines: Adhere strictly to all documentation guidelines issued by payers and the Centers for Medicare & Medicaid Services (CMS). Ensure that all required elements for each service type are consistently included in your notes.
- Use clear, specific, and consistent language: Employ unambiguous, precise, and consistent language when describing the patient’s status, the interventions provided, and the outcomes achieved. Avoid vague generalizations.
- Document changes promptly: Make it a standard practice to document all changes in the patient’s condition, modifications to their treatment plan, or their response to therapy as soon as they occur.
- Standardize documentation processes: Implement standardized documentation templates and protocols across your entire organization. This ensures consistency, completeness, and accuracy regardless of which clinician is charting.
- Always include time spent on time-based services: For time-based CPT codes such as 90834 (38–52 minutes) and 90837 (53+ minutes), documentation must clearly reflect the actual time spent with the patient. Also use EHR-integrated time-stamp fields or template prompts to ensure this detail is never overlooked.
- Distinguish the type of therapy provided: Clearly document whether the session was for individual, group, family, or crisis therapy.
Mistake 6: neglecting payer-specific rules and timely filing limits
This mistake typically occurs when providers submit claims without carefully considering each payer’s unique requirements or by missing crucial timeframes for filing, leading directly to denials, delayed payments, and substantial lost revenue.
How this neglect occurs
Neglecting payer-specific rules and timely filing limits is a two-pronged problem:
- Ignoring payer-specific rules: Each insurance payer—be it Medicare, Medicaid, or private insurers—operates under its own distinct set of billing guidelines, documentation standards, authorization requirements, and coding preferences. For instance, one payer might mandate pre-authorization for specific therapy sessions or limit which CPT codes are reimbursable for certain diagnoses. If a behavioral health provider adopts a “one-size-fits-all” approach to claim submission without tailoring to each payer’s unique demands, claims are highly likely to be rejected or denied.
- Neglecting timely filing limits: Insurance companies enforce deadlines for submitting claims, known as timely filing limits. These deadlines can vary significantly, ranging from as short as 30 days to over a year, depending on the specific payer and policy. If a claim is submitted even one day after this deadline, it is almost invariably denied outright, making it impossible for the provider to collect payment for the services already rendered.
How to avoid neglection
Preventing these costly errors requires a systematic approach:
- Develop payer-specific checklists: Create and maintain detailed checklists for each major insurer you work with, outlining their unique billing guidelines, documentation requirements, and authorization processes. Regularly review and update these checklists.
- Implement systematic timely filing tracking: Establish robust internal processes for tracking and meeting all timely filing deadlines. This could involve automated alerts from your billing software, dedicated staff responsibilities for submission, and regular review of claims aging reports.
Best practices for proactive coding compliance in behavioral health
In behavioral health, coding is rarely black-and-white. Services are highly personalized, time-based, and heavily scrutinized for medical necessity. Proactive compliance ensures not only proper reimbursement but also ethical care delivery, audit readiness, and alignment with mental health parity laws. The strategies below are designed specifically for behavioral health providers, RCM teams, and administrators who want to move beyond reactive fixes and embed a culture of precision and accountability.
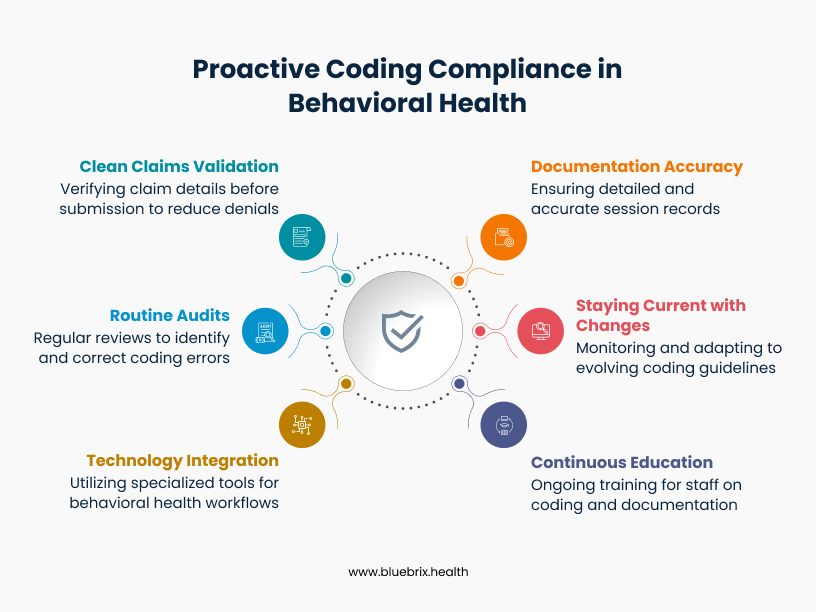
1. Behavioral health–aligned documentation
Coding accuracy starts with documentation that fully captures the complexity and clinical intent of each session. This is especially critical in behavioral health, where subjectivity is high and treatment spans multiple modalities.
Best practices include:
- Document session start and end times for all time-based services (e.g., 90832, 90834, 90837)
- Include specific therapeutic techniques used (e.g., CBT, DBT, EMDR, play therapy)
- Clearly note the client’s response to interventions and clinical progress
- Use evidence-based assessment tools, like PHQ-9, GAD-7, C-SSRS, or ASAM criteria
- Ensure diagnoses align with DSM-5 and are supported by narrative justifications
- For group therapy, include individualized notes—even within shared sessions
2. Stay ahead of behavioral health coding changes
Behavioral health coding guidelines are constantly evolving and often differ from physical health norms. Staying current means monitoring updates that impact your specific service lines and payers.
Focus areas include:
- CPT updates for psychotherapy (e.g., changes to interactive complexity or add-on codes for E/M)
- ICD-10 updates for behavioral health diagnoses, particularly under categories F01–F99
- Payer-specific rules around ABA therapy, MAT (e.g., Suboxone management), IOP, PHP, and telebehavioral health
- Changes in documentation requirements for therapy duration, scope of license, and consent policies
- Medicaid carve-out rules for behavioral health in your state
3. Continuous education for clinical and billing staff
Behavioral health compliance isn’t just a billing issue—it’s a clinical one too. Training must include both documentation and coding accuracy, tailored to your staff’s roles.
Key elements:
- Train clinicians (e.g., therapists, psychiatrists, LCSWs) on what their notes must include to support billing codes
- Educate billers/coders on payer-specific nuances like modifiers (e.g., 95 for telehealth), incident-to billing, and scope-of-license rules
- Cover common BH pitfalls: inaccurate time tracking, duplicate billing, unbundling services, and E/M + therapy code misuse
- Incorporate real claim denials into learning sessions to close the feedback loop
- Reinforce training quarterly or after any major regulatory update.
4. Leverage behavioral health–specific technology
Generic EHRs and billing systems often fall short in behavioral health. Invest in tools that are purpose-built for BH workflows, including:
- Integrated therapy note templates with fields for time tracking, interventions, MSE, and risk assessments
- Claim scrubbing engines configured for BH codes, modifiers, and payer rules
- Support for telehealth billing, including correct place-of-service codes and consent documentation
- Built-in PHQ-9/GAD-7 tracking for measurement-based care initiatives
5. Conduct routine, behavioral health–focused internal audits
Internal audits should be as nuanced as the services they review. Behavioral health audits should target:
- Time-based psychotherapy codes: Are the documented minutes accurate?
- E/M with psychotherapy: Is medical necessity documented for both components?
- Scope-of-license billing: Are services rendered by credentialed providers within their allowable scope?
- Telehealth claims: Are proper modifiers and documentation for virtual care used?
- Group therapy and IOP notes: Are individual progress documented even in shared settings?
Use mock audits and random samples. Look beyond compliance—track patterns that may point to workflow issues or staff needing support.
6. Prioritize clean claims with BH-specific validation
Reduce denials by verifying behavioral health details before claims are submitted:
- Confirm authorization requirements are met for high-cost services like ABA or IOP
- Match provider credentials to the services rendered (e.g., an LMSW cannot bill 90791 under some plans)
- Double-check telehealth place-of-service codes and proper modifiers
- Validate that the diagnosis supports the procedure, especially for short-term therapy