The hidden cost of managing by retrospective metrics
Managing healthcare operations using retrospective metrics does more than slow decision-making. It quietly erodes patient access, revenue stability, staff morale, and leadership confidence, often without anyone noticing until the impact is hard to reverse.
When teams only see problems weeks or months later, every delay compounds across clinical, operational, and financial workflows.

Access delays and patient dissatisfaction
When insights arrive 30 to 90 days late, scheduling and care coordination teams are operating without visibility into what is actually happening on the ground.
For example, a primary care practice may overbook appointments based on last month’s no-show rates. Meanwhile, prior authorizations are taking longer under updated CMS rules. The result is predictable chaos. Appointments run late, patients wait longer, and care teams scramble to adjust schedules that were never realistic to begin with.
Patients feel this immediately. Longer wait times, delayed referrals, and fragmented handoffs all show up as lower satisfaction scores. When real-time barriers like bed availability, specialist capacity, or authorization delays are invisible, patient experience suffers first.
Unrecoverable revenue leakage
Retrospective reporting also hides revenue risk until it is too late to fix.
Monthly denial summaries often surface trends weeks after claims were submitted. By then, coding errors, eligibility gaps, or payer rule changes have already impacted a full billing cycle. Once timely filing or appeal windows close, that revenue is gone for good.
For multi-site practices and health systems, this creates silent leakage. Undercoded encounters, missed modifiers, or documentation gaps may only be detected during quarterly audits. What could have been corrected at the point of care turns into permanent revenue loss.
Staff burnout from reactive firefighting
Lagging indicators force teams into constant cleanup mode.
Revenue cycle staff spend most of their time working aged denials, chasing expired authorizations, and reprocessing claims that should have been clean the first time. Clinical teams face similar pressure, rushing to address discharge delays or readmission risks that were flagged long after the opportunity to intervene.
This reactive work environment takes a toll. Month-end crunches become routine. Overtime increases. Burnout rises across billing, coding, nursing, and care coordination roles. Instead of improving processes, teams are stuck fixing yesterday’s problems.
Flawed executive decision-making
For executives, retrospective dashboards create a false sense of confidence.
Metrics may look healthy until remittance data tells a different story weeks later. Length-of-stay trends appear stable while underlying case mix shifts go unnoticed. Leaders make investment and growth decisions based on incomplete information.
This disconnect often leads to misaligned priorities. Organizations invest in surface-level improvements while deeper operational gaps continue to drain margins. Over time, these blind spots force reactive course corrections that quietly erode financial performance year after year.
Understanding lagging indicators in healthcare
Lagging indicators are still the backbone of healthcare reporting today. They help organizations understand what already happened, but they offer very little help when teams need to act in the moment. To understand why real-time operational reporting matters, it helps to first look at how lagging indicators work and where they fall short.
Defining lagging indicators
Lagging indicators measure outcomes after the fact. They confirm results once clinical, operational, or financial activity is already complete.
In healthcare, these metrics became standard because legacy systems were built around episodic care, delayed billing cycles, and limited provider accountability for outcomes. Documentation happened first. Coding followed. Claims were submitted. Payments arrived weeks later. Reporting naturally came at the end of that chain.
These indicators are useful for validating performance, but they provide no visibility into what is unfolding right now. They cannot warn teams about authorization issues in progress, documentation gaps during the visit, or operational bottlenecks forming mid-day.
In simple terms, lagging indicators explain the past. They do not protect the present.
Common examples in practice
Most healthcare organizations rely heavily on delayed metrics such as:
- Monthly productivity reports that reflect work completed weeks earlier
- Denial summaries compiled after claims are adjudicated
- Length-of-stay reports generated post-discharge
- Quality scorecards released quarterly or annually
These reports are familiar and widely accepted. They help leadership understand trends, but they rarely support timely intervention.
Why they are structurally backward-looking?
The problem is not the metric itself. It is the way healthcare data flows.
Operational events move through a long sequence. An encounter occurs. Documentation follows. Coding happens later. Claims are submitted. Adjudication and remittance come last. Reporting is triggered only once the cycle closes.
On top of that, data lives in separate systems. EHRs, billing platforms, scheduling tools, and payer portals often exchange information in batches rather than continuously. Even when APIs exist, many organizations still rely on flat files or scheduled exports, which introduces delays measured in weeks.
As a result, insight always arrives after the window to act has closed.
When lagging indicators work and when they do not?
Lagging indicators still have a role.
They work well for:
- Long-term trend analysis
- Regulatory audits and compliance validation
- Annual planning and executive reporting
They break down in environments where timing matters. In value-based care, where denials must be prevented before submission, readmissions must be avoided before discharge, and care coordination happens across multiple touchpoints daily, delayed insight becomes a liability.
When revenue leakage, care gaps, or operational breakdowns are only visible after the fact, organizations are left explaining outcomes instead of shaping them.
What real-time operational reporting actually means?
Real-time operational reporting shifts healthcare organizations from reacting to problems after they occur to preventing them while they are still forming. It is not just about faster reports. It is about seeing meaningful operational signals early enough to act.
Real-time vs. near-real-time, explained simply
Real-time reporting reflects events within seconds or minutes of when they happen.
For example, a claim submission triggers an immediate status update. A bed becomes available and the system reflects it instantly. An authorization delay is flagged the moment it occurs.
Near-real-time reporting introduces short delays, often 15 to 60 minutes, due to polling cycles or batch processing. This is common in many modern EHR environments. While near-real-time is useful for monitoring, it can still miss critical intervention windows during busy clinical or operational periods.
The difference matters. True real-time supports same-shift decisions. Near-real-time mostly supports awareness.
Faster reporting is not the same as actionable intelligence
Many organizations try to fix lagging insight by accelerating existing reports. Monthly dashboards become weekly. Weekly reports become daily.
This feels like progress, but it does not change outcomes.
Faster reports still describe what already happened. Actionable intelligence goes a step further. It interprets events as they occur and connects them directly to decisions.
Instead of reviewing denial trends after the fact, teams see payer rule changes as claims are created. Instead of analyzing length-of-stay outliers later, care managers are alerted while discharge barriers are forming.
Speed alone reduces delay. Intelligence changes behavior.
Timing beats volume every time
Real-time success is not about collecting more data. It is about delivering the right information at the right moment.
Overloaded dashboards filled with raw data overwhelm users and reduce adoption. Event-driven insights focus attention on what actually needs action. A single alert about a delayed authorization at check-in can prevent a chain of denials downstream.
In value-based care, many revenue and care gaps exist purely because of timing. When insight arrives early, small interventions prevent large downstream losses.
Core capabilities that enable real-time operational visibility
Real-time operational visibility means being able to see what is happening across a healthcare organization right now, not yesterday or last week. To do this, systems need a few core capabilities that work together to turn raw data into timely, useful information.
Event-driven data ingestion
Instead of collecting data once a day in large batches, modern healthcare systems listen for changes as they happen.
For example:
- A patient is discharged.
- A claim is submitted.
- An appointment is confirmed.
The moment these events occur, the system captures them and updates dashboards or alerts immediately. This removes delays and ensures leaders and staff always have the latest information, even in busy health systems handling thousands of updates every minute.
In simple terms: the system updates itself instantly whenever something changes.
Interoperability standards and APIs
Healthcare data lives in many systems such as EHRs, billing software, scheduling tools, and payer portals. For real-time visibility, these systems must talk to each other smoothly.
Standards like FHIR and HL7 define how data is shared, while APIs act as secure connectors between systems. This makes it possible to:
- Check insurance eligibility in real time
- Track referral status instantly
- Pull patient information from multiple sources without delays
In simple terms: common rules and connectors allow different systems to share information quickly and safely.
Data normalization across workflows
Each system records data in its own way. One system may use different codes or formats than another. If this data is not standardized, reports become unreliable.
Normalization means converting all incoming data into a common structure so that:
- Patient records match across systems
- Billing and clinical data align
- Reports reflect the true picture of operations
In simple terms: messy data is cleaned and organized so everything matches and makes sense.
Role-based operational views
Not everyone needs to see the same information.
- Revenue teams need to see claims and denials.
- Care teams need to see patient risks and follow-ups.
- Nursing teams need to see bed availability and patient flow.
Role-based views ensure each user sees only what is relevant to their job. This avoids clutter and helps people focus on what needs action right now.
In simple terms: everyone gets a dashboard designed for their role, not a one-size-fits-all screen.
Alerting, thresholds, and exception reporting
Real-time visibility is only useful if people know when something needs attention.
Instead of reviewing long reports, the system:
- Watches for problems automatically
- Sends alerts when metrics cross set limits
- Highlights only unusual or risky cases
For example, it may alert staff if authorization is delayed or if claims are likely to be denied. Over time, smarter rules reduce unnecessary alerts so staff are not overwhelmed.
In simple terms: the system flags problems early and tells the right people, instead of making them hunt for issues.
Together, these capabilities help healthcare organizations:
- Identify issues as they occur
- Act faster on operational and financial risks
- Reduce manual work and guesswork
- Improve patient care and revenue outcomes
Real-time operational visibility is less about having more data and more about delivering the right information to the right people at the right time
Real-time reporting through the lens of each healthcare function
Real-time operational reporting looks different depending on who is using it. The value comes from tailoring insight to the decisions each team needs to make during the day, not at the end of the month.

Clinical leadership perspective
Clinical leaders rely on timely visibility into patient flow, staffing, and care quality risks.
With real-time reporting, they can see live census levels, bottlenecks in patient movement, and early signs of staffing strain. If patient volume spikes or discharge delays begin to form, leaders can reallocate staff, escalate support, or adjust protocols immediately.
Instead of reviewing yesterday’s discharge summaries, clinical leaders act on what is happening right now. This helps protect quality metrics, reduce avoidable delays, and keep care teams aligned throughout the shift.
Operations and administrative teams
Operations teams live in a world of constant coordination. Schedules, rooms, staff availability, and patient movement all change throughout the day.
Real-time reporting brings these signals together. Teams can spot underutilized rooms, delayed turnovers, or growing queues before they cascade into missed appointments or overtime. When issues surface early, interventions are faster and less disruptive.
Shared operational views also reduce manual coordination. Fewer phone calls, fewer spreadsheets, and fewer handoffs mean smoother daily throughput across locations.
Revenue cycle management teams
For revenue cycle teams, timing is everything.
Real-time insight allows eligibility issues, authorization gaps, and documentation problems to be identified at registration or charge capture, not weeks later during denial review. Claims can be validated against current payer rules before submission, reducing rework and write-offs.
Instead of chasing aged denials, teams focus on prevention. This improves clean claim rates, stabilizes cash flow, and reduces burnout across billing and coding teams.
Executives and system-level leaders
Executives need a clear, current view of operational health across the enterprise.
Real-time reporting gives leadership situational awareness into capacity strain, financial risk, and performance against value-based targets. Issues surface early, while there is still time to adjust strategy, staffing, or investment priorities.
Decisions move from quarterly reviews to informed, in-the-moment course corrections. Leadership shifts from reacting to surprises to steering with confidence.
Regulatory and value-based care implications
As healthcare continues to shift toward value-based care, real-time operational reporting is no longer optional. Regulatory programs increasingly reward organizations that can see risks early and act before outcomes are locked in.
- Organizations that operate this way are better positioned to capture shared savings, avoid penalties, and meet performance thresholds across value-based programs administered by Centers for Medicare & Medicaid Services.
- Real-time operational visibility connects inpatient, outpatient, and post-acute settings. Discharges, referrals, medication changes, and follow-ups trigger immediate updates that care teams can act on without delay. This level of coordination improves follow-up rates, reduces fragmented handoffs, and directly supports quality measures tied to continuity of care. It also reduces the manual tracking that often overwhelms care coordinators.
- Programs focused on bundled payments, advanced primary care, and performance-based reporting require accurate attribution, risk adjustment, and timely documentation. Real-time reporting helps teams monitor readiness continuously rather than scrambling at reporting deadlines. It supports faster response to rule changes, tighter control over quality measures, and stronger alignment between care delivery and reimbursement.
- Traditional compliance models rely on periodic audits and retrospective validation. This leaves organizations exposed between reporting cycles. Continuous readiness flips the model. Performance is monitored as care is delivered. Gaps are addressed before they become penalties. Reporting becomes a live feedback loop rather than a post-mortem.
From dashboards to operational readiness
Many healthcare organizations already have dashboards. The problem is that dashboards alone do not create action. Real-time operational reporting only delivers value when insight is directly tied to intervention and accountability.
Why dashboards alone fall short?
Dashboards are designed for observation, not execution.
They show trends in A/R aging, bed occupancy, denial rates, or utilization. Teams may review them during meetings, but daily work continues unchanged. Clinicians still rely on phone calls and manual follow-ups. Revenue teams still chase denials after submission. Operations teams still manage capacity through spreadsheets and workarounds.
Over time, dashboards create a false sense of control. The data looks organized, but outcomes do not improve because no one is guided on what to do next.
The shift from monitoring to intervention
Operational readiness begins when insight triggers action automatically.
Instead of simply flagging an issue, real-time systems route it to the right person with context and next steps. An authorization delay is escalated before the visit. A documentation gap is highlighted during the encounter. A length-of-stay outlier prompts a care coordination review while discharge is still possible.
This shift closes the gap between insight and action. Teams spend less time interpreting data and more time fixing problems while they are still preventable.
Embedding intelligence into daily workflows
Adoption improves when intelligence appears inside the tools teams already use.
Rather than logging into separate dashboards, staff see prompts, alerts, and recommendations within EHR screens, scheduling systems, and billing worklists. Documentation gaps surface during charting. Scheduling blocks adjust automatically when capacity limits are reached. Claims are prioritized based on real-time denial risk.
This embedded approach reduces friction, shortens training time, and makes real-time reporting part of daily work instead of an extra task.
Creating accountability through shared visibility
Operational readiness also depends on shared understanding.
When clinical, operational, and financial teams see the same data at the same time, accountability becomes clearer. Discharge delays connect to revenue impact. Documentation quality links directly to denial risk. Capacity constraints are visible across departments.
Shared visibility reduces finger-pointing and encourages ownership. Issues are addressed collaboratively rather than escalated after the fact. Over time, this alignment strengthens trust and improves performance across the organization.
Common barriers to real-time operational reporting
Even when the value of real-time operational reporting is clear, many healthcare organizations struggle to implement it. The barriers are rarely just technical. Most are rooted in how systems, teams, and habits have evolved over time.
Fragmented systems and siloed data ownership
Healthcare data is scattered across multiple platforms. Hospitals may run one EHR, ambulatory clinics another, and billing teams yet another system altogether. On top of that, payer portals and third-party tools hold critical operational signals.
Ownership of this data is often fragmented. Clinical teams manage clinical feeds. Revenue teams control claims data. IT acts as the gatekeeper between them. Each group optimizes for its own needs, which slows integration and limits shared visibility.
When systems do not talk to each other in real time, organizations are forced to piece together the story long after events occur.
Overreliance on manual reporting and spreadsheets
When centralized reporting tools feel slow or inflexible, teams create their own workarounds.
Revenue teams track denials in spreadsheets. Schedulers maintain manual capacity grids. Care coordinators log follow-ups in shared documents. These tools feel fast and familiar, but they do not scale.
Manual reporting introduces errors, breaks when staff change, and consumes hours that could be spent improving workflows. It also locks real-time insight behind disconnected, person-dependent processes.
Alert fatigue and poorly designed metrics
Not all real-time systems fail because they lack data. Many fail because they overwhelm users.
Early attempts at real-time reporting often generate too many alerts with too little context. When every small fluctuation triggers a notification, staff quickly tune them out. Important signals get buried in noise.
Metrics also matter. Alerts that ignore payer mix, patient acuity, or workflow context create mistrust. If teams do not believe the signal is meaningful, they will stop responding to it.
What high-performing healthcare organizations do differently
High-performing healthcare organizations approach real-time operational reporting differently. They do not treat it as a reporting upgrade or a short-term initiative. They treat it as core infrastructure that supports how decisions are made every day.
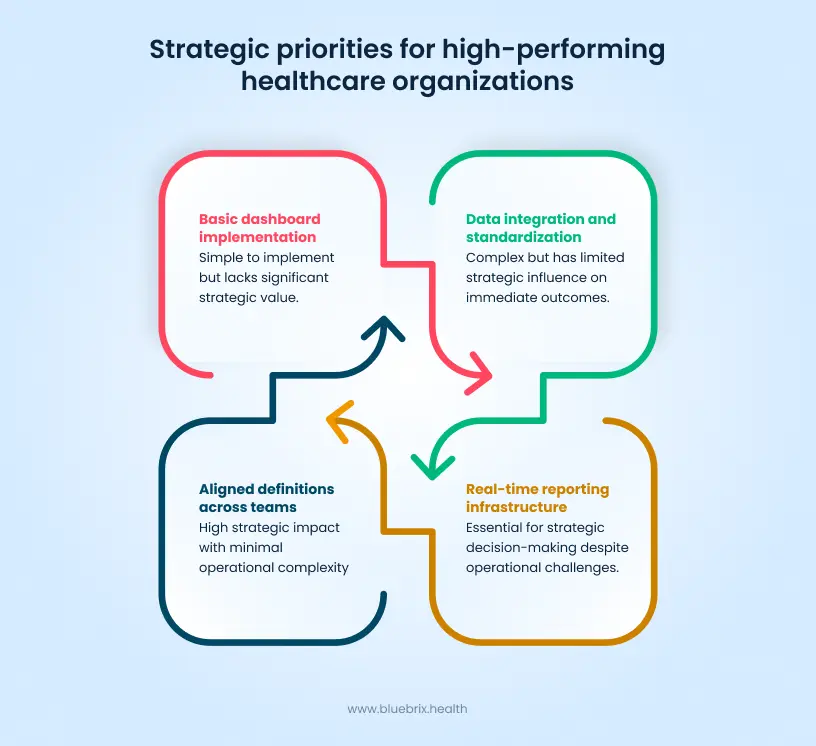
- Top-performing organizations start with decisions, not dashboards. This approach ensures reporting is practical. Leaders see staffing signals they can act on immediately. Revenue teams see denial risk tied to specific payer rules, not abstract percentages. Clinical teams see care gaps while patients are still in their care.
- They align definitions across teams so everyone measures success the same way. A clean claim means the same thing to revenue and clinical operations. Length of stay reflects downstream handoffs, not just inpatient days. Throughput targets account for both clinical quality and financial efficiency.
- These organizations focus on data foundations before building dashboards. Instead of rushing into visualization tools, they invest in integration, standardization, and data quality. Once data flows reliably across systems, reporting becomes faster, more trusted, and easier to scale.
- High-performing organizations do not view real-time reporting as a one-time rollout. They fund it like essential infrastructure, similar to network uptime or system security. Dedicated teams monitor data quality, tune alerts, and continuously refine workflows as needs evolve.
Why being proactive is becoming a strategic advantage?
In healthcare, timing compounds. Small interventions made early create outsized financial, operational, and competitive gains over time. Real-time operational reporting makes this possible by shifting action upstream, before problems harden into losses.
- When issues are caught early, the return is exponential. Fixing a documentation gap during the encounter prevents a denial altogether. Resolving an authorization issue at check-in avoids downstream scheduling disruption. These small actions scale across thousands of encounters. Over time, clean data improves forecasting accuracy, stabilizes cash flow, and reduces reliance on costly rework.
- Real-time insight reduces surprises. Predictability improves planning. Leaders can allocate resources with confidence, hit performance benchmarks more consistently, and reduce last-minute escalations that strain teams and budgets.
- Operational smoothness directly affects experience. When authorizations are resolved early and care transitions are coordinated in real time, patients wait less and experience fewer disruptions. Care teams spend less time scrambling and more time focused on patients. Staff benefit just as much. Prioritized work queues replace backlog firefighting. Clarity replaces chaos. Burnout decreases when teams feel in control of their workday instead of constantly reacting.
- Organizations that operate with real-time visibility deliver more predictable outcomes. They perform better on quality measures, maintain stronger payer relationships, and scale growth with less friction. Over time, this creates separation. High-performing systems attract patients, partners, and talent, while organizations stuck in retrospective cycles struggle to keep up.





