Clinical Documentation Improvement (CDI) plays a crucial role in healthcare by enhancing the accuracy and completeness of patient records. As the demand for precise and detailed documentation grows with changing regulatory requirements, CDI ensures that medical records accurately represent the care provided. This article examines the purpose of CDI, its advantages, and its influence on healthcare providers, patients, and financial processes.
CDI is a collaborative effort involving physicians, nurses, and coding specialists, all working together to improve documentation quality. Its primary objective is to ensure that patient care is thoroughly recorded, supporting informed decision-making and better health outcomes, both aligning with the value-based care principles. By focusing on comprehensive documentation of diagnoses and treatments, CDI strengthens the connection between clinical care and medical coding, and in the end improving healthcare delivery. As more healthcare organizations are adopting value-based care, CDI will prove to be a crucial investment that cannot be ignored.
Why is CDI Essential in Healthcare?
Ensuring the accuracy of patient records and treatment details is crucial in healthcare. Proper documentation directly impacts patient safety, regulatory compliance, and reimbursement. Without well-structured and precise records, healthcare providers may face challenges such as downcoding, claim denials, and even legal disputes.
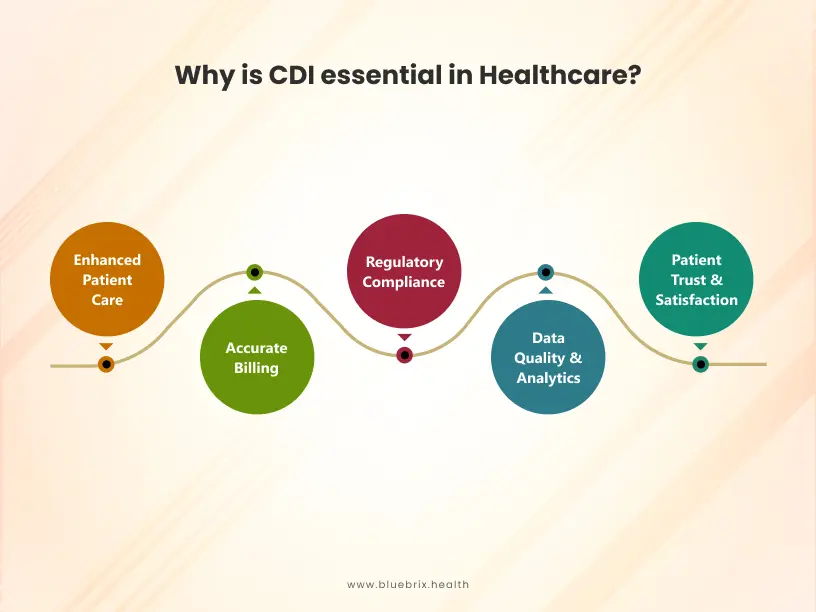
This process influences multiple areas, including patient treatment, billing accuracy, and regulatory adherence. Here’s why CDI is vital:
Enhanced Patient Care
Well-documented records enable physicians to assess a patient’s condition accurately. Clarity in medical notes reduces the risk of errors in diagnosis and treatment decisions, particularly when multiple healthcare professionals are involved in a patient’s care.
Accurate Billing
Precise documentation is fundamental in determining the appropriate charges for medical services. Proper billing practices help healthcare facilities maintain financial stability, ensuring continued delivery of high-quality care.
Regulatory Compliance
Strict documentation standards are mandated by regulatory authorities. Implementing CDI helps healthcare providers comply with these requirements, reducing the risk of legal penalties and maintaining industry standards.
Data Quality and Analytics
Accurate documentation enhances data collection and analysis. Detailed medical records allow healthcare organizations to track trends, measure performance, and identify areas for improvement. This data-driven approach also supports medical research and the development of innovative treatment methods.
Patient Trust and Satisfaction
Building patient trust is key to patient engagement and improving outcomes. Maintaining precise medical histories contributes to effective treatment planning. Having access to accurate and comprehensive records enhances care quality, leading to greater patient satisfaction and confidence in their healthcare providers.
How CDI Can Help Maximize Revenue
As healthcare continues its shift toward value-based care, ensuring accuracy in clinical documentation and coding has become essential for both maximizing revenue and enhancing the quality of care. The expertise that outsourced CDI professionals bring to this process is invaluable. CDI plays a pivotal role in helping healthcare organizations optimize reimbursements and is growing as an industry, particularly as healthcare focuses on:
- Regulatory compliance
- Managed care frameworks
- Proper reimbursement for services provided
- Quality improvement initiatives
- Mitigating liability risks
Diagnosis Grouping in an Inpatient Facility
One key advantage of inpatient CDI programs is preventing unsupported diagnoses from being included on claims. However, it is just as important to ensure that all clinically supported conditions are reported, given how inpatient facility reimbursement operates. To understand the financial impact of a successful CDI program in an inpatient setting, it is essential to grasp Medicare’s DRG payment model, which many private insurers have adapted.
Diagnosis-related groups (DRGs) classify a patient’s diagnoses into categories that influence care and reimbursement during an inpatient stay. DRG assignment is determined by the principal diagnosis along with up to 24 secondary diagnoses, including comorbid conditions (CC) or major comorbid conditions (MCC). The following examples illustrates the link between diagnoses, DRGs, and reimbursement.
Example 1: A 65-year-old female patient was admitted due to an acute exacerbation of chronic obstructive pulmonary disease (COPD). She experienced worsening shortness of breath and required respiratory support. After five days of hospitalization, she was discharged.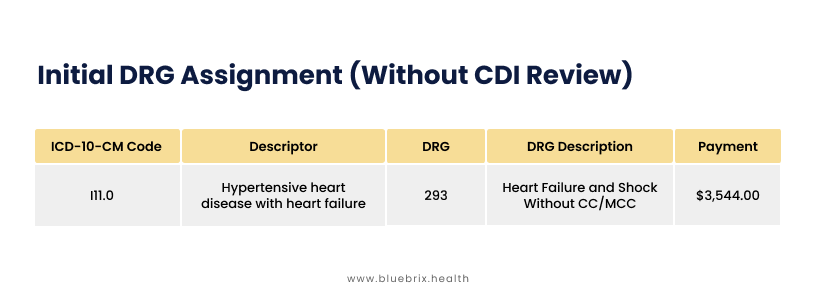
Upon review, a CDI specialist identified that the patient had acute respiratory failure with hypoxia, which was initially undocumented. Following a physician query, the documentation was revised, leading to a more precise DRG classification.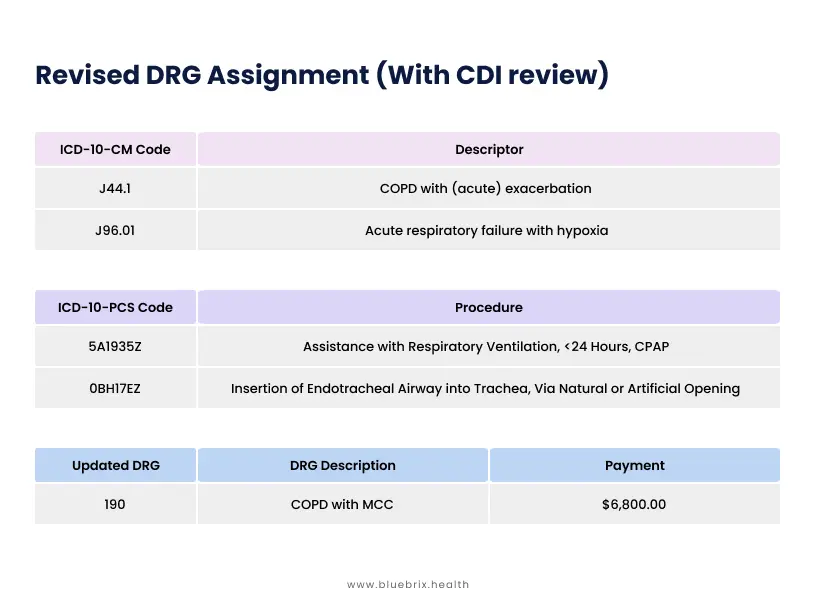
Impact of CDI
- Improved documentation accuracy reflecting the severity of illness
- Increased reimbursement ($6,800.00 vs. $4,200.00)
- Compliance with coding and billing regulations maintained
Example 2: A 65-year-old female patient was admitted due to shortness of breath with visible accessory muscle use. She has a history of hypertension and obesity. A chest X-ray revealed bilateral pleural effusions. She was started on oxygen at 2L via nasal cannula and received IV Lasix in the emergency department before being admitted to the floor. While hospitalized, her breathing improved, and a cardiology consult was ordered. She had no home cardiac medications at the time of admission. An echocardiogram from two weeks prior showed an ejection fraction (EF) of 45%. The patient was admitted with a likely newly found congestive heart failure (CHF) exacerbation.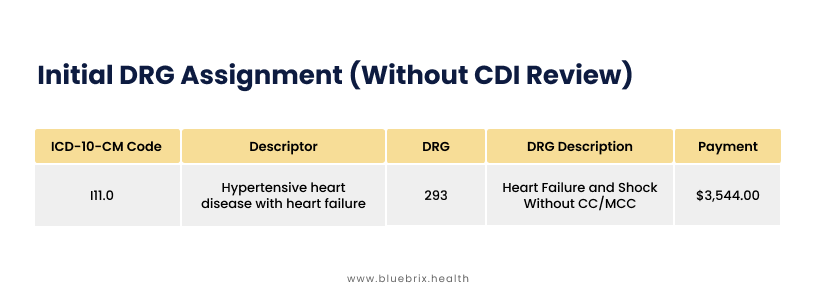
Upon review, a CDI specialist identified that the patient had acute on chronic systolic (congestive) heart failure, which was initially undocumented. A physician query led to revised documentation, resulting in a more accurate DRG classification.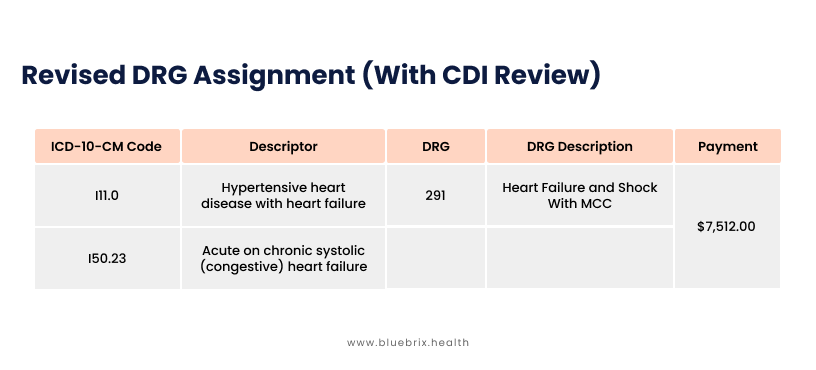 Impact of CDI
Impact of CDI
- Identified and captured the acute on chronic systolic heart failure, providing a clearer clinical picture.
- Increased payment from $3,544.00 to $7,512.00, reflecting the true complexity of the patient’s condition.
- Ensured accurate DRG assignment while meeting documentation and billing requirements.
Impact of a CDI Program in the Outpatient Setting
A CDI program in the outpatient setting can be just as financially impactful as it is in inpatient care. Physician clinics depend on a stable revenue cycle to cover operational costs, including staff salaries. Errors in coding that lead to claim denials or necessary revisions can disrupt the timely flow of payments. In an outpatient or office-based practice, the primary goal of a CDI program is to reduce these denials and revisions while ensuring documentation is comprehensive for both clinical and billing purposes.
Precise and detailed clinical documentation is critical in demonstrating medical necessity for the CPT codes included on a claim. CDI specialists help educate providers and coders on evolving coding and coverage guidelines that influence documentation requirements. Following updates, CDI specialists continue to provide support by reviewing records and claims to ensure that diagnosis codes accurately reflect what was documented and substantiate the level of E/M service billed (AMA: CPT Advice for Physician Practices). If a payer conducts an audit, a well-documented process reassures the practice that they have upheld accuracy and can confidently demonstrate compliance.
Comparison of Inpatient vs. Outpatient CDI Processes
| CDI Component | Inpatient | Outpatient(VBC) |
|---|---|---|
| CDI Specialist | Nurse with medical coding training | Medical coder with CDI training |
| Review Process | Concurrent (real-time during hospitalization) | Retrospective (after patient visit) |
| Communication | Query to provider for clarification | Provider education to improve future documentation |
| Claim Submission | After CDI review, ensuring accurate documentation before claim filing | Prior to CDI review, with education to refine documentation for future claims |
| Provider Action | Immediate improvements to documentation during hospitalization | Documentation improves at next patient visit based on CDI feedback |
Steps to Implement a Successful CDI Program
The impact of Clinical Documentation Improvement varies between hospitals and physician offices, influencing both financial outcomes and patient care. However, the core objective remains the same—ensuring accurate, complete, and compliant clinical documentation.
Regardless of the size or location of a CDI team, clarification of medical records is the foundation of a successful CDI program. While inpatient and outpatient CDI processes share common goals, their approaches differ. The table below highlights the key differences between inpatient and outpatient CDI processes.
Ensuring accurate claim submissions, successful audit outcomes, a stable revenue cycle, and improved patient health are key reasons to implement a CDI program. However, challenges can arise when key stakeholders—such as physicians, administrators, CDI specialists, and coding and billing teams—do not fully grasp the purpose of CDI or their role in the process. To establish an effective program, follow these essential steps:
1. Evaluate the Need for a CDI Program
Before launching a CDI initiative, it’s important to assess current documentation challenges and identify areas needing improvement. Consider these critical questions:
Claim Denial Trends: What proportion of claims face denials? What are the primary causes?
Quality of Care Indicators: Are there frequent hospital readmissions due to conditions such as diabetes complications or respiratory issues?
Regulatory Compliance: Are payer contract terms, MIPS benchmarks, and regulatory guidelines being met? Have audits highlighted deficiencies?
Social Determinants of Health (SDOH): Does the patient population face SDOH-related challenges that require enhanced documentation for better care coordination?
If any of these areas reveal gaps, a CDI program is necessary. Clearly define goals and implement processes that align with these objectives.
2. Set CDI Review Selection Criteria
The approach to CDI reviews depends on the facility type and program goals:
Inpatient CDI Programs: May use electronic health record (EHR) alerts to flag complex diagnoses at admission, facilitating real-time documentation improvements.
Outpatient CDI Programs: Often rely on randomized chart audits or targeted reviews based on diagnosis-related reports.
Establishing well-defined review criteria ensures efforts are focused on high-impact areas.
3. Develop Standardized Clinical Guidelines
Structured decision-making protocols streamline CDI queries and reduce provider fatigue.
Prioritize Important Queries: Not every missing detail requires a query. For example, if a patient’s diabetes appears controlled based on lab results, querying may be unnecessary. However, if HbA1C exceeds 9 and GFR is below 60, a query should be initiated to clarify severity and complications.
Ensure Consistency in Queries & Training: Standardized guidelines help avoid unnecessary interruptions while maintaining accuracy and compliance in documentation.
4. Perform Regular CDI Compliance Audits
Routine CDI audits drive continuous improvements and adherence to ethical guidelines. A structured assessment framework should analyze:
- The impact of CDI efforts on reducing denials and improving documentation
- Non-beneficial activities that may be wasting time or resources
- Proven strategies that yield measurable improvements
- Sustaining a CDI program requires ongoing data-driven adjustments to enhance efficiency and compliance.
5. Promote Collaboration Among Teams
Strong communication between CDI specialists, coders, and providers is critical for success. Effective collaboration ensures:
- Coders accurately translate clinical documentation into billable codes
- Physicians receive ongoing CDI training through targeted education sessions led by CDI specialists
- CDI specialists act as a bridge between clinical terminology and coding requirements, enhancing both claims accuracy and patient documentation
- By following these steps, organizations can establish a CDI program that improves reimbursement and compliance as well as strengthens the quality of patient care.
Conclusion
CDI professionals in healthcare are dedicated to enhancing the accuracy and completeness of clinical documentation, which plays a crucial role in medical billing. Effective CDI practices ensure that healthcare providers receive fair compensation for the services they deliver, minimizing claim denials and optimizing revenue cycles. While implementing a CDI program can present certain challenges, the long-term advantages far outweigh the initial hurdles.
This is especially relevant today, as the healthcare industry rapidly adopts new technologies and shifts toward value-based care models. As a result, the demand for CDI is expected to rise, enabling providers to deliver high-quality patient care while maintaining financial stability through the support of CDI initiatives and medical billing services. At blueBriX, we help you streamline documentation, enhance revenue, and stay compliant.
Let’s start to transform your documentation. Contact us today to get started.