In the world of value-based care, the acronym “CMS” is often synonymous with regulatory hurdles. However, the launch of the CMS ACCESS Model signals something different: an opportunity. Short for Advancing Chronic Care with Effective, Scalable Solutions, ACCESS isn’t just another pilot program.
By moving away from fee-for-service and toward Outcome-Aligned Payments (OAPs), CMS is finally putting a price tag on what matters most: patient health. But for providers and digital health innovators, this shift comes with a massive question of readiness. To succeed, organizations must move past static data and fragmented systems. They need a tech stack that doesn’t just store information but orchestrates it.
In this blog, we’ll explore why your current data infrastructure might be your biggest bottleneck and how the building blocks of blueBriX can help you turn these new regulatory requirements into a competitive advantage.
Why CMS ACCESS matters now, not later?
ACCESS is no longer a future-facing CMS concept that organizations can afford to track from a distance. It is already shaping how access, coverage, and coordination are evaluated across the healthcare system. The expectations are live, enforcement is emerging, and the operational impact is real.
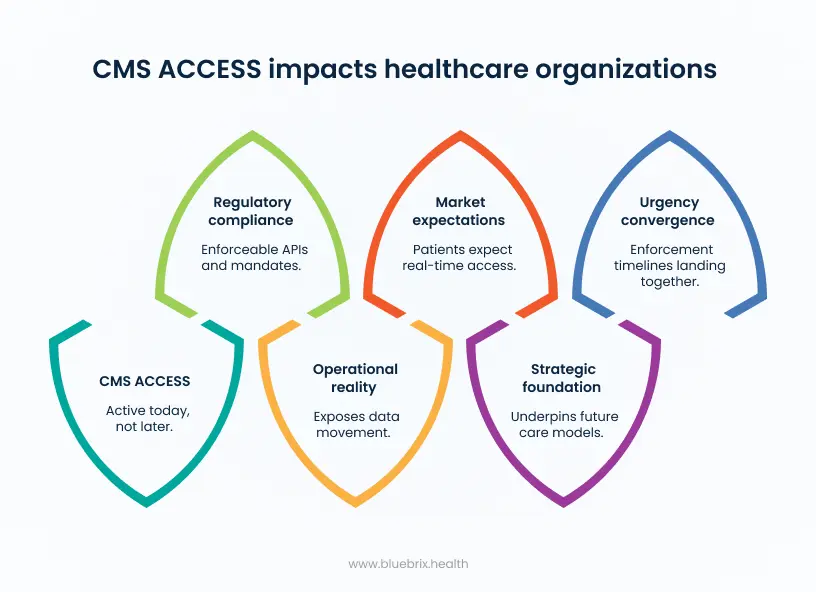
From a regulatory standpoint, ACCESS is active today. Patient Access APIs, Provider Directory APIs, and existing interoperability mandates are already enforceable, with additional API and prior authorization requirements finalized and on a fixed timeline. That makes 2025 and 2026 execution years, not planning years. Organizations that treat this period as exploratory risk compressing years of infrastructure and workflow change into a short, high-risk compliance window.
Operationally, ACCESS exposes reality. It shows how data actually moves inside an organization, not how leadership assumes it does. When claims, clinical records, and prior authorization data arrive late or only partially, care teams rely on manual workarounds to keep operations moving. The result is fragmented care, higher administrative burden, delayed decisions, and growing clinician frustration. Waiting does not pause these failures. It amplifies them.
ACCESS is also reshaping expectations in the market. Patients increasingly expect real-time, app-based access to their health information, independent of payer portals or provider systems. Organizations that meet this expectation build trust and engagement. Those that do not appear opaque and outdated. CMS is deliberately reinforcing this shift by treating data access as a baseline requirement rather than a differentiator.
Strategically, ACCESS is foundational to what comes next. Interoperable, standardized data underpins value-based care, advanced analytics, AI-driven decision support, and new payment structures. Organizations that delay ACCESS readiness are not just taking on compliance risk. They are limiting their ability to participate meaningfully in future care and reimbursement models.
The urgency comes from convergence. ACCESS enforcement timelines, ONC FHIR and USCDI expansions, and prior authorization reforms are all landing in the same window. This convergence removes the illusion of “later.” What looks like optional modernization today becomes forced remediation tomorrow, often under audit pressure, financial penalties, or operational disruption.
ACCESS matters now because the cost of waiting is already visible. It shows up as compliance exposure, operational drag, lost strategic flexibility, and reduced competitiveness. Organizations that act early control the pace and shape of their transformation. Organizations that wait inherit urgency without leverage.
What CMS ACCESS exposes inside healthcare organizations?
CMS ACCESS acts as a stress test for how healthcare organizations actually operate once data exchange becomes standardized, time-bound, and measurable. When APIs replace informal workarounds and metrics become public, long-standing inefficiencies that were easy to explain away are suddenly visible to regulators, providers, members, and partners.
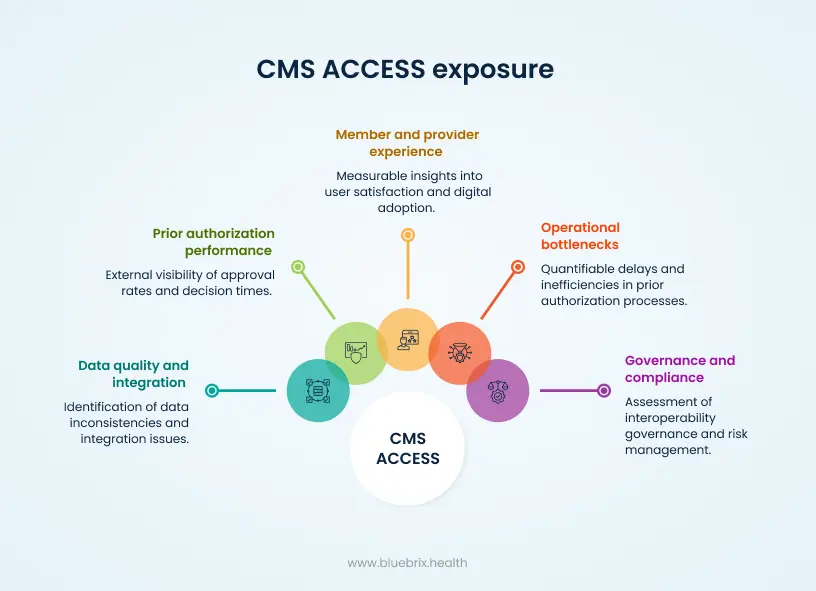
Operational bottlenecks that can no longer be hidden
Once prior authorization timelines are enforced and timestamped through APIs, delays become quantifiable. Manual routing, staffing gaps, and backlog management issues show up immediately when urgent requests exceed 72 hours or standard requests exceed seven days.
When decisions, extensions, and denials must move through a Prior Authorization API and be included in required reporting, operational friction stops being anecdotal. It becomes a documented performance issue that leadership must explain and address.
Actual prior authorization performance, not perceived performance
CMS ACCESS reporting exposes the full prior authorization picture. Total request volumes, approval and denial rates, average decision times, and structured denial reasons are no longer internal data points. They become externally visible indicators of how restrictive, inconsistent, or inefficient authorization policies really are.
Because prior authorization history must be retained and shareable for multiple years, patterns also emerge over time. Repeated denials for the same services or codes across different plans or transitions in coverage become easier to identify, removing the ability to treat each case as isolated.
Data quality and integration debt across systems
Patient Access, Provider Access, and payer-to-payer APIs surface data quality issues that were previously buried inside systems. Incorrect primary care provider attribution, outdated provider directories, incomplete clinical histories, and mismatched identifiers become obvious when data must be consumed by external applications.
Patient Access API usage metrics add another layer of exposure. Low adoption, frequent errors, or failed data transfers indicate whether core systems can actually deliver complete and accurate FHIR data. Mapping gaps, inconsistent source systems, and brittle integrations become visible through real usage rather than internal testing.
Member and provider experience in measurable terms
CMS-mandated metrics make it clear which organizations still rely on fax, portals, and manual follow-ups, and which support streamlined digital workflows. Provider friction is no longer a subjective complaint. It is reflected in turnaround times, denial patterns, and electronic transaction success rates.
On the member side, low Patient Access API usage or high timeout and error rates reveal confusing app experiences, weak onboarding, or lack of trust in how data sharing is presented. CMS ACCESS turns experience issues into data points that can be compared across plans.
Governance, risk, and compliance maturity
CMS ACCESS also exposes whether an organization has mature governance around interoperability. Required logging, telemetry, consent management, and audit trails show whether APIs are actively monitored and managed or simply deployed to meet a deadline.
Once metrics are public and comparable, weak governance becomes a broader risk. Poor performance can affect reputation, STAR ratings, network negotiations, and regulatory scrutiny. Organizations that treated CMS ACCESS as a one-time IT task are differentiated from those that built it as a sustained operating capability.
In effect, CMS ACCESS removes opacity. It reveals how well data, workflows, and accountability actually function when transparency is enforced by design rather than by intent.
The execution gap between CMS policy and day-to-day reality
The execution gap exists because CMS has moved decisively on policy, while payers and providers are still operating within the constraints of legacy technology, limited funding, and deeply embedded manual workflows. On paper, CMS ACCESS assumes a healthcare system that is already API-native and operationally aligned. On the ground, many organizations are still working through foundational modernization.
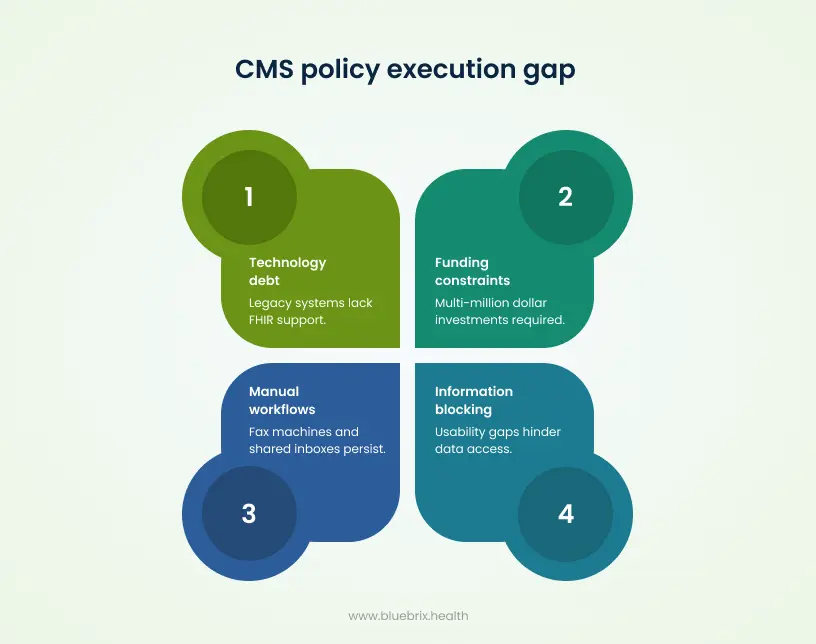
Policy expectations outpace operational readiness
CMS rules are written with the assumption that data flows through FHIR-based APIs, that prior authorization can move in near real time, and that ACCESS performance can be measured and reported consistently. In reality, a significant share of payer and provider systems still rely on batch processing, custom integrations, and non-FHIR data models.
Recent survey data highlights the scale of this disconnect. Nearly half of payers and more than half of providers had not begun meaningful work on CMS-0057-F API requirements, despite firm deadlines approaching in 2026 and 2027. This lag is not about awareness. It reflects the gap between regulatory ambition and the operational starting point of many organizations.
Technology debt creates friction policy cannot eliminate
Legacy EHRs, utilization management platforms, and claims systems often lack native FHIR support. To meet CMS expectations, organizations are forced to layer middleware, build custom mappings, and maintain parallel workflows. These stopgap solutions increase complexity and fragility rather than simplifying data exchange.
Even when APIs are technically available, maintaining them accurately in real time introduces ongoing challenges. Changes in provider affiliations, member coverage, and care relationships must be reflected immediately across payer-to-payer and provider access exchanges. Policy language defines the requirement but does not reduce the operational burden of keeping those connections current and reliable.
Funding and capacity constraints slow execution
The cost of compliance is material. Many payers estimate multi-million-dollar investments to implement and operate the required APIs, while providers often lack clarity on total costs for technology upgrades, integration work, and staff training. These financial realities compete with other strategic priorities and thin operating margins.
Organizations also report shortages in internal expertise. Defining an enterprise interoperability strategy, hiring or training staff with FHIR and API experience, and coordinating across IT, compliance, operations, and clinical teams all take time. Smaller and rural organizations face these constraints most acutely, widening the readiness gap further.
Manual workflows collide with automated expectations
CMS envisions an environment where prior authorization is automated, trackable, and auditable, with clear decision timelines and structured responses. Day-to-day operations still rely heavily on fax machines, portals, shared inboxes, and manual routing between teams.
These workarounds persist because they are familiar and functional in the short term. However, once turnaround times, denial reasons, and status visibility become reportable metrics, manual processes stop being operational quirks and start becoming compliance and experience risks. What once felt manageable becomes measurable exposure.
Information blocking rules expose usability gaps
ONC’s information blocking regulations prohibit artificial delays or barriers to data access, yet patients and providers continue to struggle to obtain and use health information effectively. This highlights another dimension of the execution gap. Legal permission to share data does not automatically translate into practical usability.
Organizations are often caught between strict anti-blocking expectations and legitimate concerns about security, liability, and workload. This tension can lead to conservative behaviors that slow access and appear obstructive, even when there is no intent to block. CMS policy addresses the right to access, but daily operations determine whether that access is meaningful.
In short, the execution gap is not rooted in resistance to CMS goals. It reflects the reality that policy has leapt ahead of infrastructure, workflows, and capacity. Closing this gap requires more than compliance planning. It demands deliberate investment in technology modernization, workflow redesign, and cross-functional ownership that bridges regulation and reality.
What CMS ACCESS actually expects from healthcare organizations?
ACCESS expectations are not abstract or interpretive. They are specific, technical, and enforceable. CMS defines who must act, what must be built, how data must be exposed, and how performance will be judged. This is not a push for better intentions around interoperability. It is a prescriptive operating requirement.
At its core, ACCESS requires regulated healthcare organizations, especially payers, to deliver standardized, API-based access to defined data sets on fixed timelines. That access must be reliable, fast, secure, and measurable. CMS is not evaluating plans based on effort. It is evaluating outcomes.
CMS clearly defines who is accountable
Primary accountability sits with CMS-regulated payers. This includes Medicare Advantage plans, Medicaid and CHIP programs across fee-for-service and managed care, and Qualified Health Plan issuers on the Federally Facilitated Exchanges. These organizations are responsible for hosting the required APIs and ensuring mandated data is available when and how CMS specifies.
Providers are part of the accountability chain. While they do not host most ACCESS APIs, CMS expects contracted providers to be ready to consume payer data, participate in electronic prior authorization, and comply with information blocking requirements. ACCESS is enforced payer-first, but it functions across the payer provider boundary.
CMS expects a defined set of FHIR APIs, not workarounds
CMS does not accept portals, PDFs, flat files, or batch feeds as substitutes. ACCESS requires live FHIR R4 APIs that external applications, providers, and other payers can securely connect to.
At a minimum, organizations must support Patient Access APIs that expose all maintained claims, encounter, and clinical data to members through applications of their choice. Provider Directory APIs must publish accurate, public, and continuously updated network data in FHIR format.
Under CMS 0057 F, additional APIs become mandatory. Provider Access APIs must allow in-network providers to retrieve claims, clinical, and prior authorization data within one business day. Payer-to-Payer APIs must support seamless exchange when members change or hold concurrent coverage. Prior Authorization APIs must expose coverage rules, accept electronic requests, and return structured decisions, denial reasons, and validity periods through FHIR.
CMS specifies both the data and the technical standards
ACCESS leaves little room for interpretation. CMS specifies exactly what data must be shared, including adjudicated claims, encounter data, USCDI-aligned clinical data, and defined prior authorization information for non-drug services. Partial exposure or delayed availability once data exists internally is not acceptable.
Technical standards are equally explicit. APIs must align with FHIR R4, ONC USCDI requirements, and the 21st Century Cures Act. Secure access must use OAuth 2.0 and SMART on FHIR, with reliable patient matching, consent management, audit logging, and traceability built in.
Performance, timeliness, and reporting are mandatory
ACCESS compliance is not achieved by standing up endpoints. Systems must be stable, responsive, and observable. Most APIs are required to deliver data within one business day of availability or request. Slow responses, outages, and unreliable performance directly undermine compliance.
CMS also requires measurement. Payers must report Patient Access API usage annually, including unique users and data transfer volumes. As prior authorization APIs come online, organizations must report request volumes, turnaround times, approval and denial rates, and API reliability. Compliance is judged on real-world use, not technical existence.
Providers are expected to operationalize ACCESS, not ignore it
Providers are expected to use certified EHR technology that supports FHIR APIs and electronic prior authorization. By 2027, at least one electronic prior authorization transaction via API is required for certain quality reporting programs.
CMS also expects providers to maintain accurate digital contact information, support ADT notifications, and adapt workflows so payer data delivered through APIs is usable at the point of care. ACCESS that exists but is ignored operationally still represents failure.
In short, ACCESS requires healthcare organizations to move from intent to execution. It defines specific APIs, specific data, fixed timelines, and measurable outcomes. Organizations that treat ACCESS as an IT project miss the point. It is an operating model requirement that cuts across technology, compliance, workflows, and accountability.
Who actually owns CMS ACCESS inside the organization?
CMS ACCESS does not sit cleanly within a single department. Legally, accountability rests with the payer’s executive leadership and compliance function. Operationally, ownership is distributed across multiple teams whose workflows and decisions are now exposed through APIs and public metrics. Organizations that fail to reconcile this split ownership tend to struggle the most.
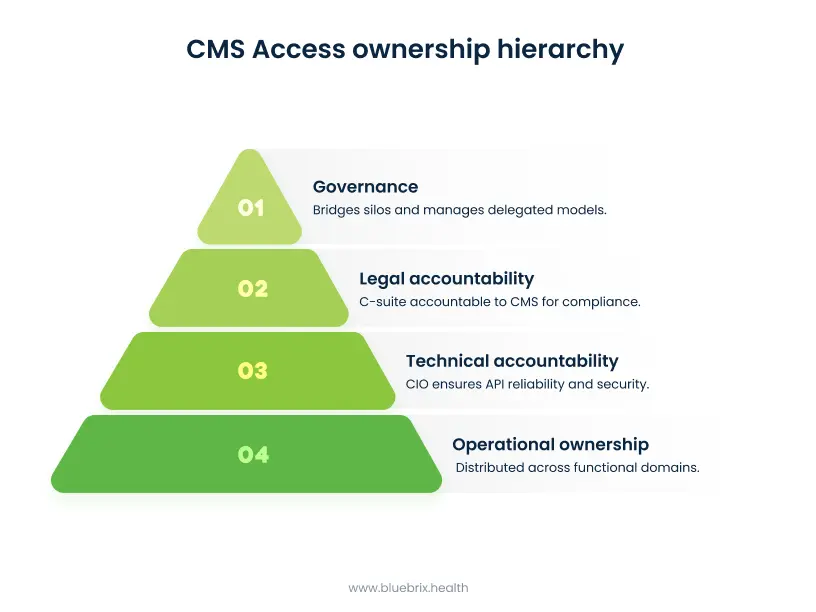
Legal and regulatory accountability sits at the top
Ultimate responsibility for CMS ACCESS lies with the C-suite of CMS-regulated payers. The Chief Compliance Officer or General Counsel is accountable to CMS for meeting regulatory requirements, submitting accurate performance reports, and responding to audits, penalties, or corrective action plans. From a regulatory standpoint, CMS does not recognize internal handoffs. Non-compliance remains an enterprise risk.
The Chief Information Officer carries parallel accountability for technical execution. CMS holds payers responsible for the reliability, security, and accuracy of their APIs. Uptime, error rates, and data integrity are not IT best practices. They are compliance obligations tied directly to CMS enforcement.
Operational ownership is distributed by function
While legal accountability is centralized, day-to-day ownership is fragmented across operational domains.
Utilization management and prior authorization leaders own the Prior Authorization API in practice. They control medical policies, decision criteria, turnaround times, denial rationales, and the metrics CMS now requires to be reported publicly. CMS ACCESS exposes utilization management performance directly, making this function a critical operational owner.
Provider network and contracting teams are responsible for the accuracy of Provider Directory APIs and the effectiveness of Provider Access APIs. These teams ensure that network affiliations, contract status, and provider data reflect reality, and that in-network clinicians can actually retrieve payer data as intended.
Member services and digital experience teams own patient-facing adoption. Consent flows, app onboarding, education, and ongoing usage of the Patient Access API sit squarely within their remit. CMS measures not just whether access exists, but whether members are using it, making this function visible through reported metrics.
Governance must bridge silos
Because CMS ACCESS spans claims, clinical data, pharmacy, and delegated arrangements, cross-functional governance is essential. Many organizations establish an enterprise interoperability committee, typically under the CIO or CCO, to coordinate priorities, resolve ownership conflicts, and maintain consistent standards across teams.
Delegated models add another layer of complexity. Even when data is hosted or managed by subcontractors or third-party administrators, the primary payer retains full accountability to CMS. Governance must therefore extend beyond organizational boundaries to include vendors and partners.
Provider-side ownership mirrors the complexity
On the provider side, ownership also spans roles. The Chief Medical Informatics Officer or Chief Information Officer typically owns EHR integration and workflow changes needed to consume payer APIs effectively. Compliance teams ensure adherence to information blocking rules and regulatory expectations.
In practice, CMS ACCESS succeeds only when ownership is explicit, shared, and enforced. Organizations that clarify who owns what, and how those roles interact, are far better positioned to meet both the letter and the intent of CMS ACCESS requirements.
The CMS ACCESS and Value-Based Care connection
CMS ACCESS is not a parallel compliance initiative running alongside value-based care. It is the data plumbing that makes value-based care viable at scale. Without longitudinal, shareable, and near real-time data, most VBC contracts struggle to deliver on their promises, even when incentives are aligned.
Shared data is the foundation VBC depends on
Value-based care requires organizations to measure outcomes, manage risk, and coordinate care across settings and time. That work depends on complete clinical and claims data, not just what sits inside a single EHR or one health plan.
CMS interoperability rules force this foundation into place. By mandating standardized FHIR APIs for patients, providers, and payers, CMS ensures that a longitudinal record follows the member. This continuity enables accurate quality measurement, risk adjustment, and care gap detection, all of which are core to VBC performance but difficult to achieve in fragmented data environments.
CMS ACCESS APIs directly enable VBC workflows
The ACCESS APIs map directly to value-based workflows. The Provider Access API allows in-network clinicians to retrieve claims, USCDI clinical data, and prior authorization information at the point of care. This supports proactive care management, chronic disease programs, and accountable care organization workflows that depend on seeing beyond the local EHR.
The Payer-to-Payer API extends this capability across coverage changes. When members switch plans, years of historical claims and clinical data move with them, subject to consent. This allows new payers to stratify risk accurately, price contracts appropriately, and continue care plans without restarting assessments and interventions from scratch.
Better risk stratification and population health outcomes
CMS ACCESS also strengthens population health and risk management. Interoperability requirements create multi-year, multi-source datasets that plans can use to identify rising-risk members earlier and with greater precision.
When API-sourced data is integrated into population health platforms, organizations can close care gaps, target interventions more effectively, and monitor outcomes across episodes of care. This improves the return on investment for shared-savings, bundled payment, and other value-based arrangements by aligning data visibility with accountability.
Reducing fee-for-service friction to support collaboration
Administrative friction undermines value-based goals. Delays in prior authorization, incomplete information, and manual handoffs increase avoidable utilization and frustrate care teams. By standardizing prior authorization and data exchange, CMS ACCESS reduces these frictions and supports smoother coordination across the care continuum.
This shift reframes the payer-provider relationship. Instead of acting as gatekeepers through opaque processes, payers become data partners to ACOs and risk-bearing providers. CMS has explicitly positioned interoperability as a prerequisite for improved coordination and movement toward value-based payment models, not as an optional enhancement.
In practical terms, CMS ACCESS turns value-based care from a contractual aspiration into an operational possibility. It supplies the shared, trustworthy data layer that VBC models require to function as designed.
What readiness for CMS ACCESS actually looks like?
CMS ACCESS readiness is not defined by having an endpoint live or a project plan on file. It shows up as a fully funded, cross-functional program where APIs are operational, usage is measurable, documentation is audit-ready, and workflows actually change. Anything less tends to collapse under reporting, audit, or adoption pressure.

Strategy and governance are explicit and active
Ready organizations establish clear enterprise ownership, typically through a standing interoperability committee that includes the CIO, CCO, utilization management leadership, and clinical stakeholders. This group actively tracks progress against CMS deadlines and ties CMS ACCESS work to broader business objectives such as value-based care performance and STAR ratings.
Readiness also includes a completed gap analysis against CMS requirements. Tools like payer-to-payer readiness checklists are used to identify regulatory and operational gaps, with named owners and timelines. This shifts CMS ACCESS from abstract compliance into managed execution.
Technical capabilities are production-grade, not experimental
Technically ready organizations run live FHIR R4 APIs in production. Patient Access and Provider Directory APIs are already active, with Provider Access, Payer-to-Payer, and Prior Authorization APIs on a clear path to 2027 compliance.
These APIs pass external testing, maintain high uptime, and conform to US Core and USCDI requirements. Telemetry is in place to monitor performance in real time, including connectivity rates, time to first data, first-pull success, and payload validation against CMS specifications. Failures are detected and resolved before they surface externally.
Operational workflows are redesigned, not layered
Readiness requires operational change. Prior authorization is digitized end to end, with structured rules, timestamped decisions, and specific denial reasons delivered through APIs. Providers can submit and track requests electronically from within their EHRs, eliminating reliance on fax or portals.
On the member side, consent management and app onboarding flows are live and tested. Organizations rehearse public reporting internally by running dry audits of prior authorization volumes, turnaround times, and denial rates. Quarterly reviews ensure evidence is available for CMS inquiries.
Data and security foundations are in place
Ready organizations have reliable data pipelines that normalize claims, encounters, labs, and clinical notes into FHIR with consistent refresh cycles. Patient matching is accurate, data is retained for multi-year payer-to-payer exchange, and historical continuity is preserved.
Information security teams formally sign off on OAuth 2.0 and SMART on FHIR implementations, granular consent controls, audit logging, and incident response procedures. Security is treated as a compliance requirement, not an afterthought.
In practice, readiness looks like confidence. Confident data exchange, confident reporting, and confident responses to audits. Organizations that reach this state treat CMS ACCESS as a sustained operating capability rather than a one-time regulatory milestone.
Where blueBriX fits in the CMS ACCESS conversation?
blueBriX fits into the CMS ACCESS landscape as an API-first, interoperability-native platform built to work with CMS-mandated data flows rather than around them. Instead of acting as another closed system, it plugs directly into payer APIs and enables providers to operationalize CMS ACCESS in day-to-day care delivery.
Built for FHIR and CMS interoperability from day one
blueBriX is designed with native FHIR R4 support and open APIs, making it well aligned with CMS 9115 F and CMS 0057 F expectations. It can consume Provider Access and Payer-to-Payer data while contributing clinical data back through standards-based interfaces.
Because it was not retrofitted from a legacy EHR architecture, blueBriX supports real-time data exchange without heavy middleware or brittle integrations. This allows organizations to modernize workflows incrementally without a full rip-and-replace of existing systems.
Focused on behavioral health and care coordination realities
CMS ACCESS challenges are most visible in behavioral health, ABA, and care coordination, where prior authorization volume is high and data is highly fragmented. blueBriX is purpose-built for these domains, enabling closed-loop referrals, centralized provider directories, remote patient monitoring, and patient engagement on top of interoperable data.
By aligning these workflows with CMS ACCESS APIs, blueBriX helps organizations reduce authorization delays, improve continuity of care, and surface the data needed for coordination-heavy models that struggle under fragmented systems.
Connecting CMS ACCESS to value-based care execution
blueBriX extends beyond compliance by tying interoperable data to analytics, risk stratification, and multi-specialty coordination. This makes it easier for organizations participating in value-based arrangements such as ACO REACH to translate CMS ACCESS data into measurable outcomes and financial performance.
Rather than treating interoperability as a reporting obligation, blueBriX supports using shared data to drive proactive care management, reduce leakage, and improve quality performance.
Removing common modernization bottlenecks
blueBriX addresses common CMS ACCESS roadblocks through no-code application building, cloud-agnostic deployment, and built-in audit trails that support HIPAA and CMS expectations. This reduces reliance on custom integration work and shortens the path from compliance to operational use.
For providers, this means less time spent managing integration plumbing and more time focused on care delivery. For organizations under CMS scrutiny, it turns interoperability from a defensive requirement into an operational advantage.
Turning compliance into differentiation
By enabling faster referrals, smoother prior authorization workflows, and connected care journeys, blueBriX helps organizations use CMS ACCESS as a competitive differentiator. Improved data flow supports better provider experience, stronger member engagement, and downstream gains in STAR and HEDIS performance.
In the CMS ACCESS conversation, blueBriX sits at the intersection of regulation and execution. It helps organizations move from having it in theory to using it in practice.




