Picture this: it’s 8 a.m. in the ICU and you’re with a patient with respiratory failure. Twenty minutes in, you get pulled away by a central line in another room. Later, you circle back for another half hour of critical care. At the end of the day, the care is obvious — but the billing isn’t. How do you count all that time?
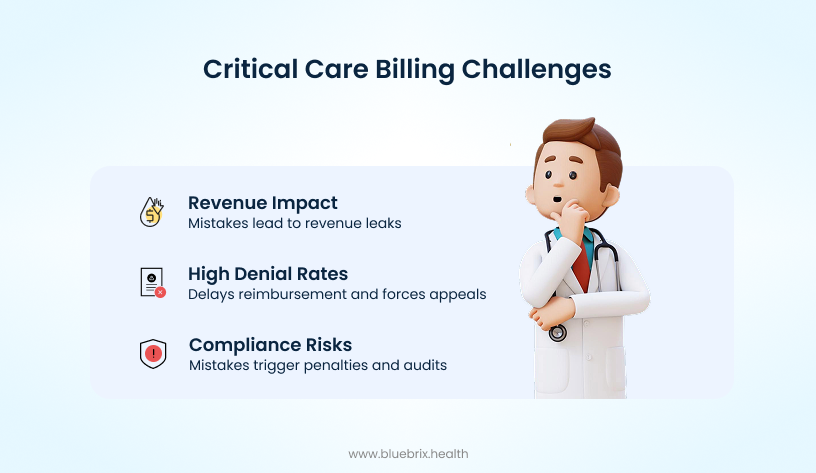
That’s the daily headache of critical care billing. Unlike routine visits, these services live under a microscope — every minute, every note, every code is questioned. The stakes are high: one slip in documentation or misapplied rule can mean denied claims, lost revenue, and unwanted attention from auditors.
This blog breaks down why not aggregating non-continuous time becomes the biggest compliance trap to watch for, and strategies that can help your team get it accounted for right — every time.
Why critical care billing is so complex — and so risky
Let’s be honest: critical care billing isn’t complicated just because the rules are technical. It’s complicated because it sits at the intersection of time, documentation, and compliance — three areas where even small errors can cost thousands.
Here’s where most providers and hospitals run into trouble:
- Time-based coding rules: Unlike most other services, critical care is billed almost entirely on time. That means every minute matters — and it must be tracked with precise start and stop times. The complication is that CPT and CMS don’t measure that time the same way. For example, under CPT rules, a 75-minute visit qualifies for 99291 + 99292, but Medicare (CMS) requires the full 104 minutes before you can bill 99292. That single discrepancy explains why denials are so common when teams aren’t clear on which standard applies.
- Documentation pressure: Critical care isn’t about just noting that a patient was “critical.” Payers expect every detail to be spelled out: the organ system at risk, the life-threatening nature of the condition, and the interventions performed. If the documentation doesn’t clearly justify the care, the claim won’t stand.
- Regulatory scrutiny: Critical care codes carry high Relative Value Units(RVU), making them prime targets for audits. Payers know this is where mistakes happen — whether it’s missed minutes, overlapping provider time, or the wrong code. What was compliant last year may not be today, and staying ahead of the changes is a full-time job.
So, how do you manage all of this? The answer lies in mastering the fundamentals of time and documentation.
Mastering critical care billing: getting the basics right
Critical care billing has no room for guesswork. The rules are built on three pillars — definitions, time, and documentation — and unless each one is nailed down, the claim won’t hold up.
Here’s what that looks like in practice:
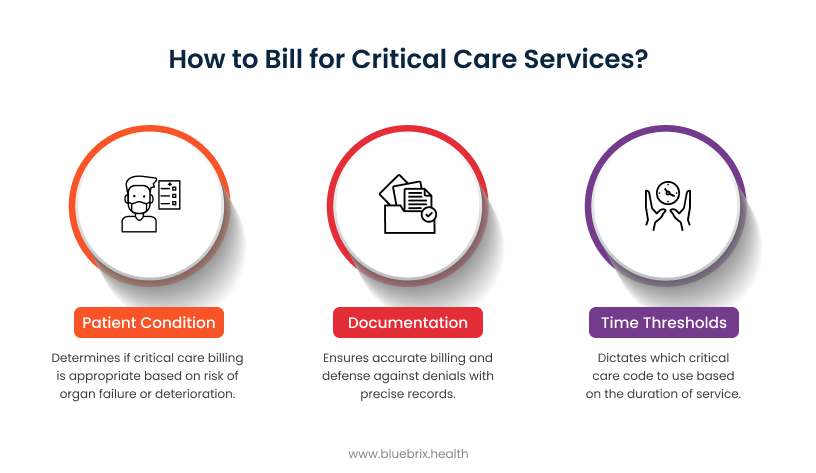
In short, getting these three basics right is the foundation for accurate billing and revenue protection. Everything else — from handling non-continuous time to dealing with payer variations — builds on this.
What qualifies for critical care?
A patient qualifies as critical care when:
- They have acute impairment of one or more vital organ systems.
- There’s a high risk of imminent or life-threatening deterioration.
- The provider’s interventions are aimed at preventing that outcome and sustaining life.
That’s the lens auditors and payers apply. If the documentation doesn’t clearly establish this, everything else — time, codes, modifiers — becomes irrelevant.
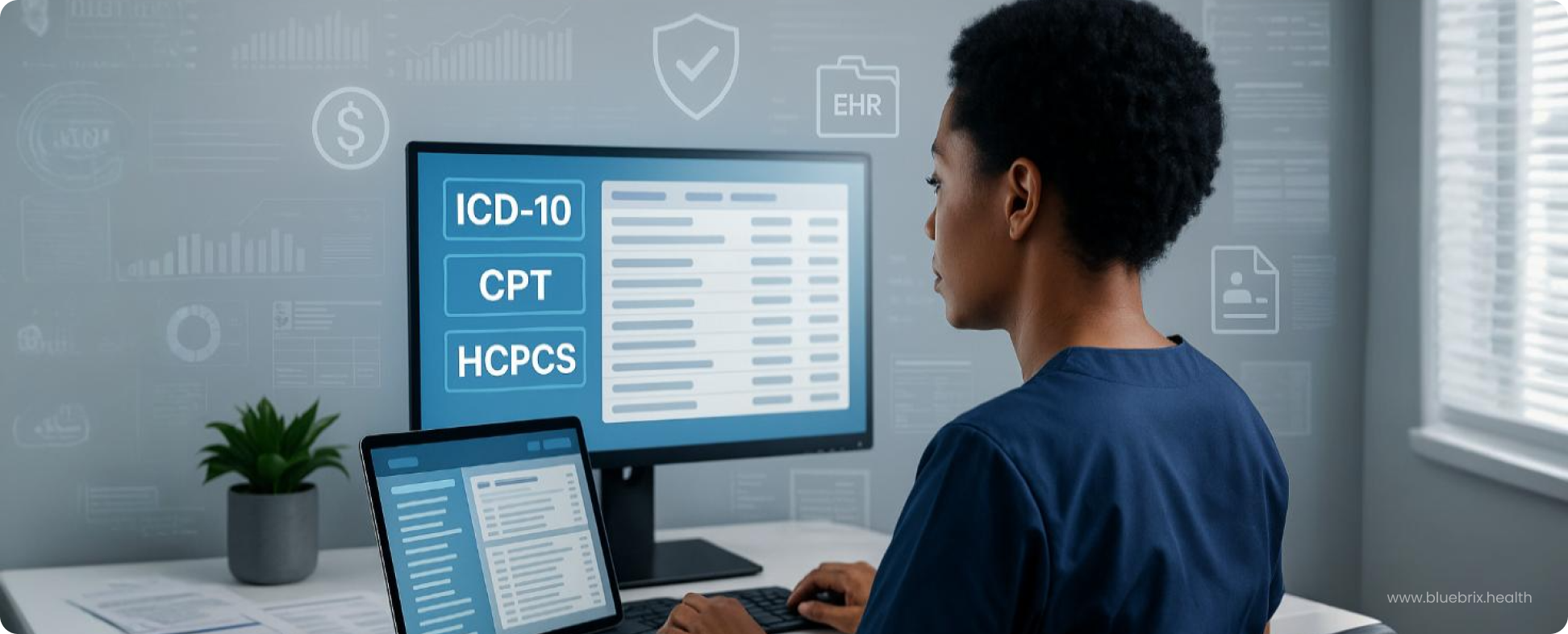
Decoding the CPT Codes: 99291 and 99292
Critical care billing starts with two core codes — and knowing exactly when to use them:
- 99291 → Covers the first 30–74 minutes of critical care provided by a single provider or group on a calendar day. If care is less than 30 minutes, it doesn’t qualify as critical care — you’ll need to bill a standard E/M code instead.
- 99292 → An add-on code for each additional 30 minutes of critical care beyond that first block.
Here’s a quick way to think about it:
- 30–74 minutes → 99291
- 75–104 minutes → 99291 + 1 unit of 99292
- 105–134 minutes → 99291 + 2 units of 99292
And so on…
It sounds straightforward, but the real complexity comes when you factor in the differences between CPT vs. CMS rules — which we’ll unpack next.
CMS vs. CPT: a critical distinction
Here’s where things get tricky. CPT and CMS don’t always agree on when you can bill that extra time.
- CPT (AMA rules): Once you hit the midpoint of the next 30-minute block (75 minutes total), you can add 99292.
- CMS (Medicare rules): Stricter. You need the full 30 minutes beyond 74. That means you can’t bill 99292 until you reach 104 minutes.
Why it matters: A claim billed at 75 minutes may pass with a commercial payer following CPT rules, but Medicare will flag it as an error. That single difference is one of the most common audit triggers in critical care billing.
The takeaway: Always know whose rules you’re playing by — because CMS won’t cut you slack.
What activities count as billable critical care time?
Not every minute with a patient in the ICU counts toward critical care billing. Only time spent directly managing the life-threatening condition qualifies.
Billable activities include:
- Direct bedside care and evaluation.
- Reviewing labs or imaging while actively managing the patient.
- Family/surrogate discussions when decisions impact immediate care.
- Documenting critical care services in the chart.
- Bundled services (like ventilator management or blood pressure monitoring).
Not billable:
- Time on separately billable procedures (e.g., intubation, central line).
- Routine rounds, discussions about other patients, or admin tasks.
- Periods when the provider isn’t immediately available to the patient.
The rule of thumb: If the time doesn’t show undivided attention on keeping the patient alive, it shouldn’t be in the critical care total.
Time aggregation and the “crossing midnight” challenge
Critical care isn’t always a straight, uninterrupted block of time — providers often step in and out throughout the day. That’s why time aggregation is allowed:
- Non-continuous time: If you spend 20 minutes in the morning and 30 minutes later in the day, you can add those together (50 minutes total) for billing.
- Crossing midnight: This is where it gets tricky.
- If care is continuous across midnight (say, 11 p.m. to 1 a.m.), bill all of it on the date you started.
- If care is split (say, 10 p.m. one day and 2 a.m. the next), each day is billed separately.
How non-continuous time adds up: a worked example
Let’s walk through a typical ICU day:
- 8:00–8:20 a.m. → 20 minutes of critical care provided
- 9:30–10:00 a.m. → 30 minutes of critical care provided
- 10:15–10:25 a.m. → 10 minutes on a central line procedure (not billable under critical care and must be excluded)
Final calculation:
- Total billable time = 20 + 30 = 50 minutes
- Correct CPT code = 99291 (30–74 minutes)
This illustrates how non-continuous episodes can be aggregated — but only after subtracting separately billable procedures. Documentation must show clear start/stop times for each episode to stand up under audit.
Why it matters: Missing these distinctions is a common reason claims get denied or flagged for audit. Every minute must be tied to the right day — with the right code.
Crossing midnight: a worked example
Let’s break down a real scenario that often trips up billing teams:
- 11:00 p.m.–11:45 p.m. → 45 minutes of critical care provided.
- 12:15 a.m.–12:45 a.m. → 30 minutes of additional critical care provided.
Here’s how it plays out:
- Same calendar day rule applies. The 45 minutes before midnight belong to Day 1.
- The 30 minutes after midnight belong to Day 2.
- You cannot combine them into one total of 75 minutes.
Correct billing:
- Day 1 (11:00–11:45 p.m.) → 45 minutes = 99291
- Day 2 (12:15–12:45 a.m.) → 30 minutes = 99291
Why it matters: Even though the care feels continuous to the provider, the calendar boundary creates two distinct billing days. Missing this distinction is a common audit trigger. Documentation must clearly show the dates, start and stop times, and that each day independently meets the threshold for 99291.
Regulatory and payer nuances: staying compliant in a shifting landscape
Here’s the reality: critical care billing isn’t governed by a single playbook. CMS, commercial payers, and CPT guidelines don’t always line up — and that’s where practices get burned.
A few compliance anchors to keep in mind:
- CMS is always stricter. Commercial payers may allow midpoint billing at 75 minutes, but Medicare won’t. For them, it’s 104 minutes or nothing.
- Aggregation rules apply, but with limits. Non-continuous time can be added up, but only if it’s medically necessary, excludes separately billable procedures, and comes from providers in the same group and specialty.
- Modifiers matter. Miss the right one — like -FS for split/shared care or -25 for a separate E/M service — and you’ve just handed payers a reason to deny.
- Prolonged services ≠ critical care. Mixing them up is a compliance landmine. Prolonged care doesn’t apply when organ failure or life-threatening deterioration is involved.
Each payer sets the rules differently, and yesterday’s “compliant” claim can be today’s denial. The safest path is staying current and building payer-specific workflows that catch errors before the claim goes out. Think of CMS as setting the “gold standard” for compliance. If your billing process holds up under Medicare rules, you’re far less likely to run into trouble with commercial payers.
Key audit triggers and administrator monitoring
Critical care billing is a favorite audit target. Why? Because high-value codes mean higher stakes — and more mistakes to find.
Administrators and compliance teams should keep a close eye on these common red flags:
- Thin documentation → Missing total time, excluded procedures, or justification of medical necessity = easy audit flag.
- Improper use of 99292 (billed at 75 minutes for Medicare) → High RVU codes are prime audit targets, and Medicare requires 104 minutes.
- Overlapping provider time → If two providers document the same minutes, payers treat it as double billing.
- Missing or incorrect modifiers → Skipping required ones like -FS (split/shared) or -25 for unrelated E/M services almost guarantees denial.
The fix isn’t complicated: build internal monitoring that catches these errors before payers do. A proactive approach can mean the difference between smooth reimbursement and a full-scale audit.
Payer variations and compliance nuances
Medicare sets the tone, but commercial payers don’t always follow the same playbook. That’s where billing teams get tripped up.
Here’s what to watch for:
- Time thresholds differ. Many commercial payers stick to CPT’s midpoint rule (75 minutes for 99291 + 99292). But Medicare requires full 104 minutes. Knowing which rule applies is critical.
- Bundling rules vary. Medicare has a strict list of services (like ventilator management, blood pressure monitoring, and pulse oximetry) that are automatically bundled into critical care and cannot be billed separately. If you perform one of these, it’s included in the critical care time, not a standalone charge. Commercial payers may allow more flexibility, but you can’t assume — some may follow CPT’s broader rules, while others mirror Medicare’s stricter stance. The key is knowing your payer’s policy before submitting the claim.
- Modifiers aren’t universal. Some modifiers that are mandatory for Medicare claims (-FS, -25, -FT) may not even be on a commercial payer’s radar.
- Critical care vs. prolonged services. Some payers are quicker to deny if they see both billed for the same patient on the same day. Misuse here is a compliance landmine.
The takeaway: one-size-fits-all billing doesn’t work. Teams need payer-specific checklists and workflows if they want to stay compliant and avoid costly denials.
Navigating split/shared critical care billing (Post-2022 CMS Guidelines)
Since 2022, CMS has tightened the rules around how physicians and non-physician practitioners (NPPs) can share critical care time. The goal is clarity — but in practice, it’s another layer of complexity.
Here’s what matters most:
- Team-based aggregation is allowed. Physicians and NPPs in the same group and specialty can combine their time. But overlapping minutes can’t be double counted.
- The “substantive portion” rule applies. Whichever provider spends more than 50% of the total time is the one who bills for the service.
- Modifier -FS is mandatory. Every split/shared claim must include it to flag that the visit was a joint effort.
The nuance here is simple: collaboration is fine, but billing must reflect the rules exactly. Miss the modifier or miscalculate the substantive portion, and the claim won’t hold up.
Documentation and time management strategies
Critical care billing is less about knowing the rules and more about applying them in the chaos of real practice. The two biggest hurdles? Tracking time accurately and backing it up with airtight documentation.
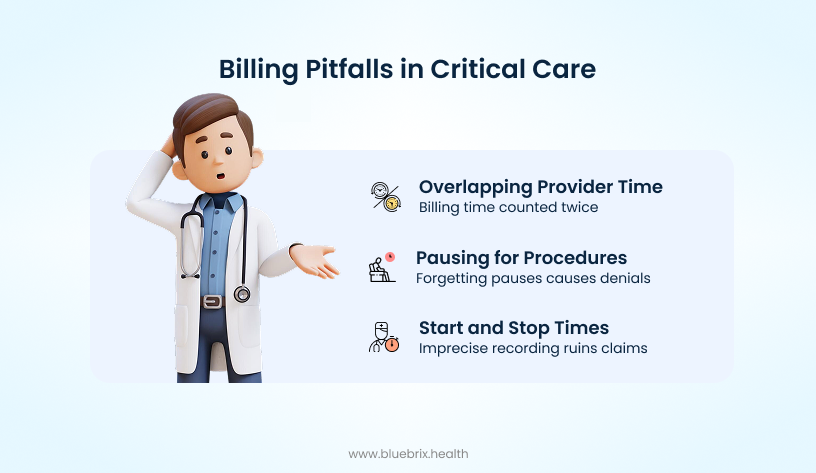
Here’s where providers and billing teams stumble most often:
The fix is consistency. Without a system for documenting every episode of care — and the discipline to subtract excluded minutes — providers risk losing legitimate revenue or inviting audits.
Time aggregation and provider collaboration
Time is the backbone of critical care billing — and also its biggest trap.
- Start-and-stop care: Providers may deliver 20 minutes in the morning, 15 minutes in the afternoon, and another 25 minutes at night. Unless each segment is documented with precise start and stop times, that day’s total can’t be validated.
- Procedural interruptions: Intubations, central lines, and other separately billable procedures require pausing the clock. Forgetting to subtract them leads directly to denials.
- Multi-provider overlap: In team-based care, only distinct time counts. If two clinicians from the same group are at the bedside simultaneously, the clock doesn’t double — it stays the same.
In other words, aggregation works in your favor only if the documentation proves it. Without accuracy, you’re not just underbilling — you’re creating audit risk.
Mastering critical care documentation
Strong documentation is your best defense against denials and audits. It’s not about writing more — it’s about writing clear, verifiable notes that connect time, necessity, and interventions.
At a minimum, every critical care note should include:
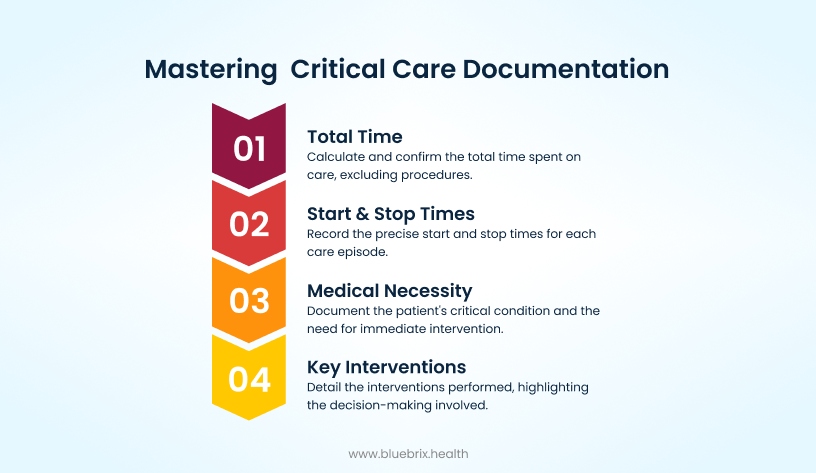
A standardized “critical care time” template can make this easier. It ensures every provider hits the same essentials: patient ID, date, start/stop times, total time, justification, interventions, and signature.
Think of documentation as more than compliance — it’s the backbone of both revenue protection and audit resilience.
Optimizing the critical care billing workflow for compliance and revenue
In critical care billing, a strong workflow is the only way to stay compliant and protect revenue. The goal is simple: capture time accurately, code correctly, and get the claim out clean the first time.
Here’s what a solid workflow looks like:
- Real-time documentation: Providers log interventions, start/stop times, and medical necessity as care happens. Waiting until later risks errors or missing details.
- Immediate coding review: Certified coders review documentation before claims go out. They check time thresholds, modifiers, and payer-specific rules — scrubbing mistakes early.
- Charge capture and submission: Once validated, claims move forward without back-and-forth corrections. Clean data in means faster reimbursement out.
This proactive approach transforms billing from a constant firefight into a reliable, revenue-protecting system.
Proactive quality control and audit strategies
Waiting for payers to flag errors is the costliest way to manage critical care billing. A proactive quality control process catches problems before claims ever leave your system.
Key practices to build in:
- Routine internal audits → Regularly review critical care claims to spot gaps in documentation, coding, or modifier use.
- Monitor common audit triggers → Examples include billing 99292 at 75 minutes for a Medicare patient or double-counting provider time. Catching these early prevents escalations.
- Correct systemic issues → Don’t just fix individual claims. Use audit findings to tighten workflows and prevent repeated mistakes.
This approach shifts audits from being a threat to becoming a tool for continuous improvement.
The role of technology in revenue cycle management
Manual tracking and paper notes won’t cut it in critical care billing. Technology can close the gaps that lead to denials and revenue loss.
Here’s where it makes the biggest difference:
- Integrated EHR + billing systems → When documentation flows directly into charge capture, you eliminate re-entry errors and speed up submissions.
- Automated time tracking → Prompts in the EHR can remind providers to record start/stop times or even auto-capture them, solving the “start-and-stop” problem.
- Predictive analytics → AI can flag high-risk claims before they’re submitted, based on denial patterns and payer behavior. That means fewer denials and faster cash flow.
Technology doesn’t replace the workflow — it strengthens it. With the right tools, billing becomes less about chasing errors and more about protecting revenue.
The RCM team as strategic partners
In critical care billing, the revenue cycle management (RCM) team shouldn’t just push claims — they should act as strategic partners in protecting financial health.
That means shifting from reactive to proactive. That means shifting from reactive fixes to proactive management. Strong RCM teams don’t just resubmit denials — they own the entire process end to end. They monitor regulatory and payer updates in real time, maintain payer-specific playbooks, and adjust workflows before issues hit claims. They also drive continuous education for both clinical and billing staff, so everyone stays aligned as rules evolve. In short, they act less like a back-office function and more like a compliance and revenue intelligence unit — closing the loop between providers, coders, and administrators.
The most effective RCM teams close the loop between providers, coders, and administrators — turning billing into a coordinated effort rather than an afterthought.
The future of critical care billing: time, technology, and transformation
Critical care billing has always been about precision — every minute, every note, every code. But the future is pushing beyond manual accuracy toward tech-enabled efficiency and resilience. The future of critical care billing isn’t just about catching mistakes — it’s about creating a revenue cycle that’s smarter, faster, and harder to break.
The AI-driven RCM
Artificial intelligence is no longer a “nice-to-have” in revenue cycle management — it’s quickly becoming essential for critical care billing.
Here’s how AI is reshaping the landscape:
- Automation of coding tasks → NLP (natural language processing) can read provider notes and assign the right codes automatically, cutting down on human error and speeding up claims.
- Predictive denial prevention → Machine learning analyzes past claims to flag high-risk submissions before they’re sent. That means errors get fixed upfront instead of during appeals.
- Staying ahead of regulations → AI systems can update coding rules in real time as CMS and payers change their policies, keeping workflows compliant without constant manual oversight.
The bottom line: AI doesn’t replace the fundamentals of accurate documentation and time aggregation — it supercharges them. Organizations that adopt these tools early will see fewer denials, faster reimbursements, and stronger revenue protection.