Billions are lost every year—not to fraud or malpractice, but to missed referrals and fragmented follow-up care. CMS’s recent proposal for a centralized provider directory isn’t just another policy update—it’s the turning point for how healthcare systems manage referrals, coordinate care, and protect their revenue.
On May 16, 2025, the Centers for Medicare & Medicaid Services (CMS) and the Office of the National Coordinator for Health IT (ONC) issued a Request for Information (RFI) titled “Health Technology Ecosystem.” This RFI solicited public input on building a modern digital health infrastructure, including centralized provider directories, interoperability standards, and digital care-navigation tools. With over 1,300 responses submitted by June 16, the signal is clear: healthcare is ready for change.
But the question isn’t whether this shift is coming. It’s how prepared your organization is to lead in this new, connected era.
The referral crisis: broken loops, lost revenue
Referrals should act like a relay baton—smoothly handed off from one provider to another. But today’s reality is messier.
- 46% of referrals sent via fax never result in an appointment.
- 50% of referring physicians don’t know if the patient ever saw the specialist.
- 65% of all referrals may be clinically unnecessary, creating waitlist bottlenecks.
- $1 million per physician per year is lost to referral leakage—when patients drift outside your network because of delays or confusion.
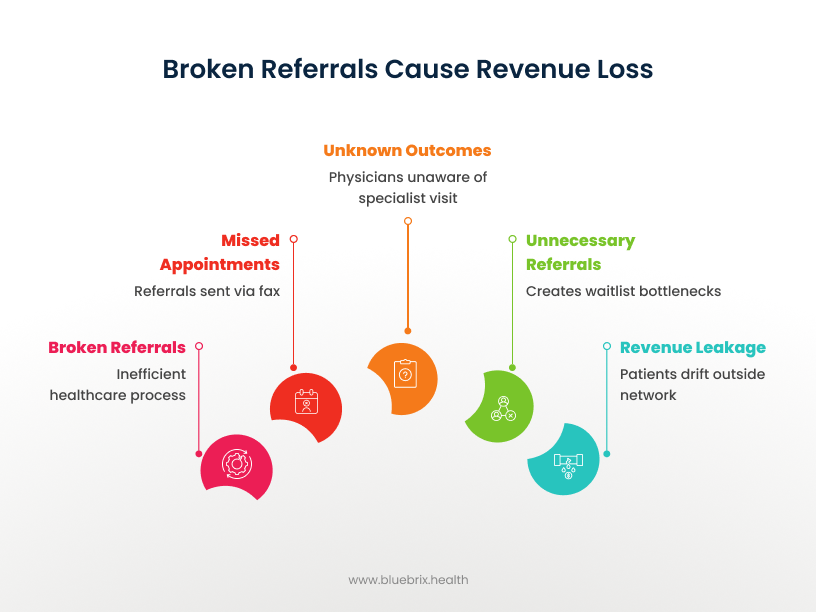
That’s not just inefficiency—it’s patient safety, satisfaction, and financial stability all at risk.
CMS’s vision: a connected, interoperable healthcare network
The proposed CMS framework centers on centralized provider directories—dynamic databases that list all credentialed providers, their FHIR endpoints, and their digital identities. Instead of relying on outdated spreadsheets, phone calls, or faxes, providers can seamlessly send referrals, track them in real time, and close the loop—all within an interoperable system.
This is not just about compliance—it’s about building digital trust and fluid care coordination.
How will centralized referral databases transform your organization?
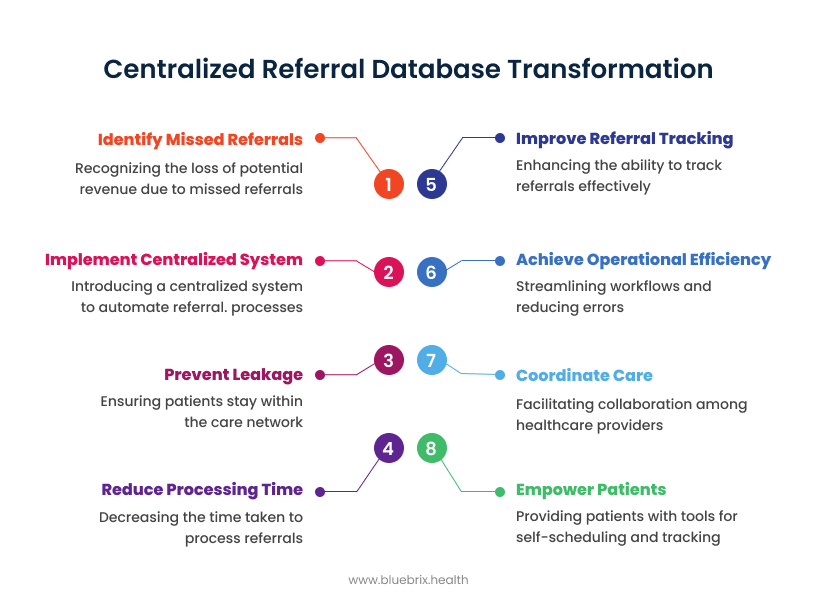
1. Revenue Protection Through Network Integrity
Missed referrals aren’t just missed appointments—they’re missed revenue.
By automating referral processes and tracking follow-ups, centralized systems:
- Prevent leakage by keeping patients within your care network.
- Reduce processing time by up to 81%.
- Improve referral tracking by 72%, according to recent studies.
And considering that admin costs account for 25% of total hospital spend, this isn’t a marginal gain—it’s a strategic financial lever.
2. Operational Efficiency at Scale
Manual referral processes are labor-intensive and error-prone.
A centralized infrastructure means:
- Real-time referral routing
- Automated patient updates and reminders
- Elimination of back-and-forth phone calls
The result? Lower staffing overhead, fewer patient no-shows, and streamlined day-to-day workflows for care teams.
3. Closed-Loop Care Coordination
When every stakeholder has access to the same referral information, care becomes truly collaborative.
- PCPs, specialists, care coordinators, and even social workers operate with a single source of truth.
- Clinical decisions improve due to more complete patient histories.
- Referral fatigue decreases, with reduced duplication and confusion.
This isn’t just workflow improvement—it’s better clinical outcomes.
4. Empowered Patient Experience
Patients today expect visibility, responsiveness, and convenience.
Centralized referral systems unlock:
- Self-scheduling through patient portals
- Real-time referral status tracking
- Automated reminders and digital forms
Organizations using these systems report a drop from days to minutes in scheduling turnaround—and a measurable boost in patient satisfaction scores.
What powers this transformation? FHIR + smart APIs
At the core of CMS’s proposal lies FHIR (Fast Healthcare Interoperability Resources)—the modern standard for healthcare data exchange.
With FHIR-enabled APIs, provider directories aren’t just static lists—they’re dynamic engines that:
- Share provider credentials and network status
- Automate referral acceptance and triage
- Integrate directly into EHRs, CRMs, and care navigation tools
This is the leap from portals and faxes to a truly digital front door for care navigation.
Addressing provider concerns: yes, it’s doable—and worth it
It’s natural to hesitate before any tech overhaul. But the evidence is reassuring.
- Organizations that implemented centralized referral management systems report better communication, lower admin workload, and faster appointment access.
- CMS is not asking providers to start from scratch. Instead, the proposal encourages leveraging existing best-of-breed data feeds and platforms—minimizing disruption.
Think of this shift not as a rebuild, but as a plug-in upgrade to the way you already work.
A new era of collaboration, powered by shared infrastructure

This isn’t just about interoperability—it’s about rethinking healthcare as a collaborative ecosystem.
CMS’s plan lays the foundation for:
- Nationwide provider directories with real-time availability
- Modern digital identity verification
- Expanded patient API functionality
- Trusted data exchange networks, reducing silos and improving speed
As HHS leadership frames it: “This is the foundational infrastructure to Make America Healthy Again.”

