As often cited by our healthcare clients and prospects, navigating the intricate web of multi-program, multi-payer realities within value-based care is a major challenge. Fragmented data, reimbursement bottlenecks, and administrative burden are common pain points. blueBriX offers a robust, highly customizable program management tool designed specifically to unify patient programs and streamline payer management, empowering your organization to thrive in the VBC landscape.
This article dives deep into the inherent complexities you face, demonstrating how a purpose-built solution like blueBriX transforms these challenges into opportunities for efficient, patient-centered care and sustained financial health.
What makes patient program & payer management so complex in value-based care?
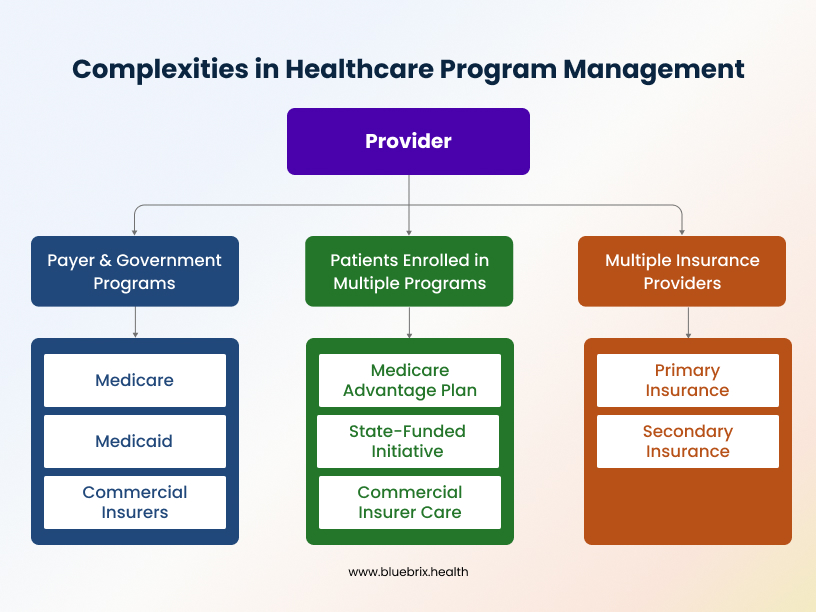
The shift to value-based care (VBC) introduces significant complexity, particularly for healthcare providers managing diverse patient programs and payer requirements. It’s no longer just about fee-for-service; it’s about outcomes and efficiency across multiple, often overlapping, mandates.
- Navigating Payer & Government-Defined Programs: Providers must comply with numerous programs set by Medicare (e.g., Chronic Care Management, Bundled Payments), Medicaid, and commercial insurers (e.g., patient-centered medical homes, disease management). Each program has unique protocols, documentation needs, and reporting standards.
- Patients Enrolled in Multiple Programs Simultaneously: A single patient might be managing type 2 diabetes through a Medicare Advantage plan, participating in a state-funded medication adherence initiative, and receiving specialized care covered by a different commercial insurer. Tracking progress and compliance across these disparate programs without duplication is a major hurdle.
- The Layer of Multiple Insurance Providers: Beyond program requirements, patients often have primary and secondary insurance from different carriers, each with distinct eligibility criteria, billing rules, and reimbursement schedules. This creates a tangled financial web.
Where do traditional EHRs fall short?
Traditional Electronic Health Records (EHRs) and manual processes struggle with this complexity. They often result in:
- Siloed Data: Information about a patient’s involvement in one program isn’t easily shared or visible to those managing another.
- Inconsistent Care: Lack of a unified view can lead to duplicated tests, conflicting instructions, and missed opportunities for coordinated care.
- Revenue Cycle Bottlenecks: Mismatched billing, missed compliance, and manual claims cause increased denials and significant reimbursement delays.
- Provider Burnout: The immense administrative burden diverts providers from patient care, contributing to stress and dissatisfaction.
What are the hidden challenges of disconnected program & payer management for healthcare providers?
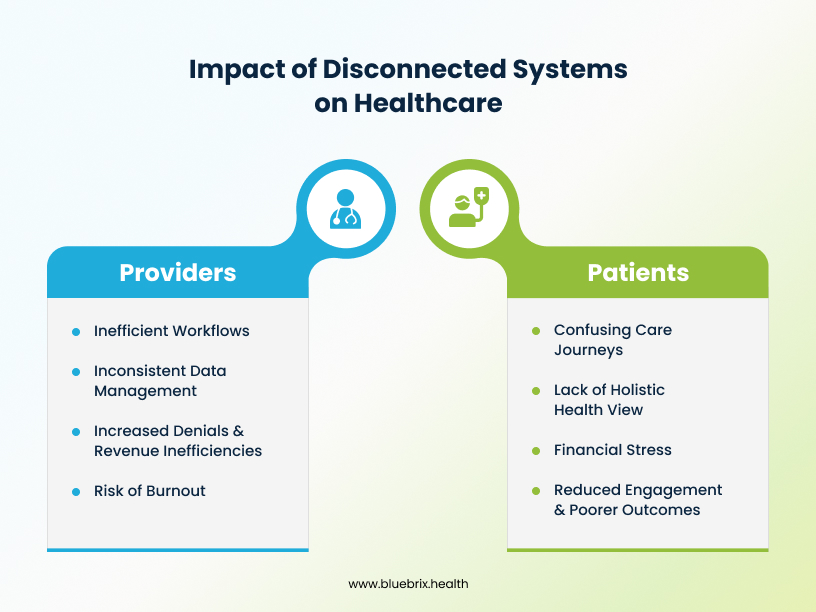
Disconnected systems and manual processes create significant operational and financial pain points for healthcare organizations and negatively impact patient experience.
For Providers:
- Manual Tracking & Siloed Data: Relying on spreadsheets and disparate software for each program and payer leads to inefficient workflows and an incomplete patient view. For instance, a large medical group in Houston, Texas, without integrated systems, could face hours of manual data entry for hundreds of patients in various chronic care management (CCM) programs, increasing errors and reducing staff productivity.
- Inconsistent Care Pathways: Different programs often have unique clinical guidelines or documentation requirements. This forces providers to toggle between various templates, increasing oversight risk and hindering standardized, high-quality care.
- Difficulty Demonstrating Program Compliance: Value-based care ties reimbursement to performance and adherence. Scattered, inconsistent data makes proving compliance for each patient in every program an arduous, error-prone task, directly impacting revenue.
- Increased Denials & Revenue Cycle Inefficiencies: Billing for complex, multi-program care is challenging. Data from Experian suggests that prior authorizations and accurate patient information are major pain points. Disconnected systems exacerbate these, leading to higher denial rates and slower cash flow.
- Risk of Burnout and Reduced Provider Satisfaction: The overwhelming administrative load associated with fragmented systems detracts from patient care and significantly contributes to clinician and staff burnout.
For Patients:
- Confusing Care Journeys: Patients often repeat information, undergo unnecessary tests, and navigate a confusing array of appointments due to uncoordinated care, leading to frustration.
- Lack of Holistic Health View: Patients rarely receive a clear, consolidated picture of their various programs and how they contribute to overall health, hindering their active engagement.
- Financial Stress: Billing errors from disconnected systems can result in unexpected out-of-pocket costs and confusion about coverage, adding significant financial burden.
- Reduced Engagement & Poorer Outcomes: A disjointed care experience lowers patient engagement, making them less likely to adhere to treatment plans and achieve optimal health outcomes.
How can a customizable EHR address complex program needs in value-based care?
At blueBriX, we know that generic EHRs fall short in value-based care. We offer an integrated, customizable program management tool that redefines EHR functionality to support the intricate realities of multi-program, multi-payer environments. It’s not just an EHR; it’s a central nervous system for your value-based care initiatives.
Key capabilities for unified program and payer oversight include:
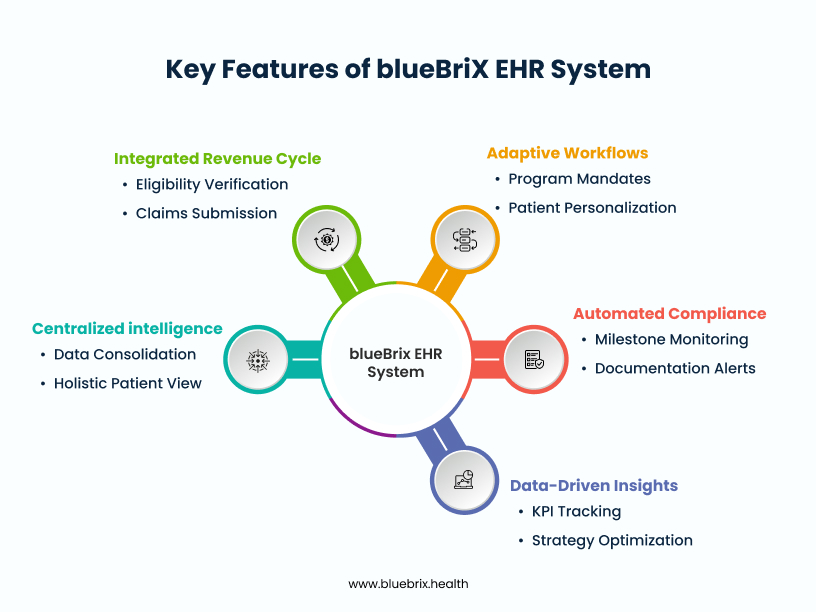
- Centralized Intelligence: A single source of truth consolidates all patient data, program enrollment, progress, and payer information. This eliminates data silos, providing a holistic, 360-degree view of each patient, enabling better decision-making and seamless care coordination.
- Adaptive Workflows: The system allows providers to dynamically tailor care pathways based on specific program mandates while personalizing them to individual patient needs. This ensures compliance without sacrificing patient-centered care.
- Automated Compliance: It automates the monitoring of critical program milestones, required documentation, and performance metrics, alerting providers to potential compliance gaps proactively. This means less paperwork and more direct patient care.
- Integrated Revenue Cycle: Our solution seamlessly connects clinical activities with billing processes. It automates eligibility verification across multiple payers, applies program-specific billing rules, and streamlines claims submission and remittance, significantly reducing denials and accelerating cash flow.
- Data-Driven Insights: Robust analytics and reporting capabilities track key performance indicators (KPIs) for each program, identify trends, and optimize strategies for better outcomes and higher reimbursement. This transforms raw data into actionable intelligence.
How does blueBriX's program management capabilities address complex needs?
blueBriX’s program management system demonstrates sophisticated capabilities specifically designed for managing multiple healthcare programs within a single organization, allowing for complex program hierarchies with main programs and subprograms, each maintaining their own specific configurations and requirements.
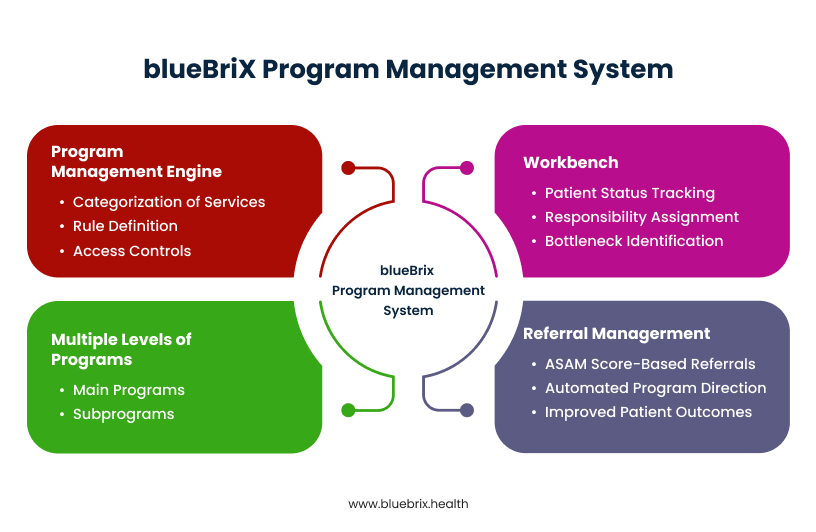
The Program Management Engine
At the core, the Program Management Engine is a module within blueBriX platform specifically designed to manage healthcare programs, which include services or procedures provided to patients. It allows for the categorization of services or procedures based on certain criteria. This engine enables organizations to define rules for including or excluding providers, patients, CPT codes, and other criteria within a program. Crucially, it manages billing strategies, enrollment strategies, care teams, and referrals, all defining the rules for patient inclusion in a program. The program management engine allows you to configure access controls/permissions and program settings, add and manage programs, add and manage features/fields related to programs.
Multiple Levels of Programs (Programs and Subprograms)
blueBriX supports complex program hierarchies.
For example, if you’re managing care for patients with diabetes, with blueBriX, your main “Diabetes Management Program” covers everything. When you have diabetic patients with unique needs, that’s where “Subprograms” come in handy.
For instance, you could have a “Type 2 Diabetes Education Subprogram” specifically for patients needing lifestyle coaching and group sessions. Or maybe a “Gestational Diabetes Care Subprogram” just for your pregnant patients. And for those on complex insulin regimens, an “Advanced Insulin Management Subprogram” could offer specialized support.
See how it works? You get one big program, then easily create tailored sub-programs to give each patient exactly the care they need, all within your blueBriX system. It helps you deliver targeted, efficient care.
Our adaptable framework allows for custom rule-setting and criteria definition at all program levels, optimizing critical aspects like user access controls, comprehensive reporting, and operational efficiency. Providers can effortlessly manage program visibility for diverse users and seamlessly integrate subprograms to align with evolving healthcare demands and enhance overall service delivery.
Workbench
The Workbench feature is a vital dashboard that offers real-time information on patients and the programs they are enrolled in. It helps in managing patient status within a program, showing how a patient’s details move from one section or status to the next level.
For example, when you’re managing a busy “Opioid Use Disorder Treatment Program” in your clinic, keeping track of every patient’s journey, from initial contact to successful recovery, can be a huge challenge, right?
That’s where the blueBriX Workbench comes in.
Think of it like your program’s mission control dashboard.
For instance, let’s say a new patient, Sarah, calls for help. Her initial status in the Workbench might be “Intake Scheduled.” Once your front desk team completes her intake, the system automatically updates Sarah’s status to “Assessment Pending.” At the same time, it automatically assigns your clinical lead, Dr. Miller, as the team member responsible for that next assessment step.
Now, if Sarah’s assessment doesn’t happen within, say, three days, the Workbench can automatically flag it with a warning. This means your team instantly sees that Sarah needs follow-up, preventing anyone from falling through the cracks.
You can quickly glance at the Workbench to see:
- Who’s where: Is John in “Treatment Phase 1”? Is Emily in “Aftercare Planning”?
- Who’s responsible: Which care team member is overseeing their current step?
- Any bottlenecks: Are there patients stuck at a certain status?
Plus, your team members with program access can pull up Workbench reports to get all the details—like the program name, patient ID, their current status, who’s on their care team, and even authorization info.
Basically, the Workbench gives you real-time visibility and control, making patient management smoother and ensuring no one gets left behind in their care journey.
Referral Management
In the evolving value-based care landscape, ensuring patients get the right care, at the right time, is crucial for both outcomes and cost efficiency. Manual referrals can create delays and care gaps, impacting your quality metrics.
blueBriX’s program management allows for robust referral management, offering options to enable, disable, or allow referrals with warnings. Notably, referrals can be set for programs based on the patient’s ASAM (American Society of Addiction Medicine) scores. The system can be configured to automatically direct patients with a specific ASAM score to appropriate programs for referral.
Let’s say a patient, Sarah, completes an initial screening. Her assessment, perhaps an ASAM score for substance use, clearly indicates she needs a specific level of care to prevent readmission or escalation of her condition – a key value-based care outcome.
Instead of a time-consuming manual process, blueBriX allows you to configure your system. Based on Sarah’s assessment results, the platform can automatically direct her to the most appropriate program for referral, like your “Intensive Outpatient Program” or a specialized “Chronic Disease Management Program.”
This seamless automation means:
- Improved patient outcomes: Patients get to the right care faster, reducing delays that can worsen conditions.
- Cost efficiency: You avoid unnecessary ER visits or higher-acuity care by intervening effectively.
- Enhanced care coordination: Referrals are standardized and tracked, boosting your ability to demonstrate coordinated care, which is vital for payer contracts and quality incentives.
You maintain full control, of course. You can choose to enable, disable, or flag referrals for specific review, ensuring flexibility while upholding your value-based care goals. It’s all about intelligent, automated pathways that support better patient health and your organization’s success.

How does blueBriX’s program management module work in a real-word scenario?
Let’s walk through a real-world scenario where blueBriX’s program management features become absolutely critical for your clinic’s success in a value-based care model.
Imagine this: Your clinic has just launched a vital new Behavioral Health Program for At-Risk Youth. The core aim isn’t just to treat, but to significantly reduce costly emergency room visits and dramatically improve long-term mental health outcomes for these young people. These are the measurable outcomes that drive success in value-based contracts. You’re getting referrals, but how do you ensure every step is seamless, compliant, and contributes to those crucial outcomes?
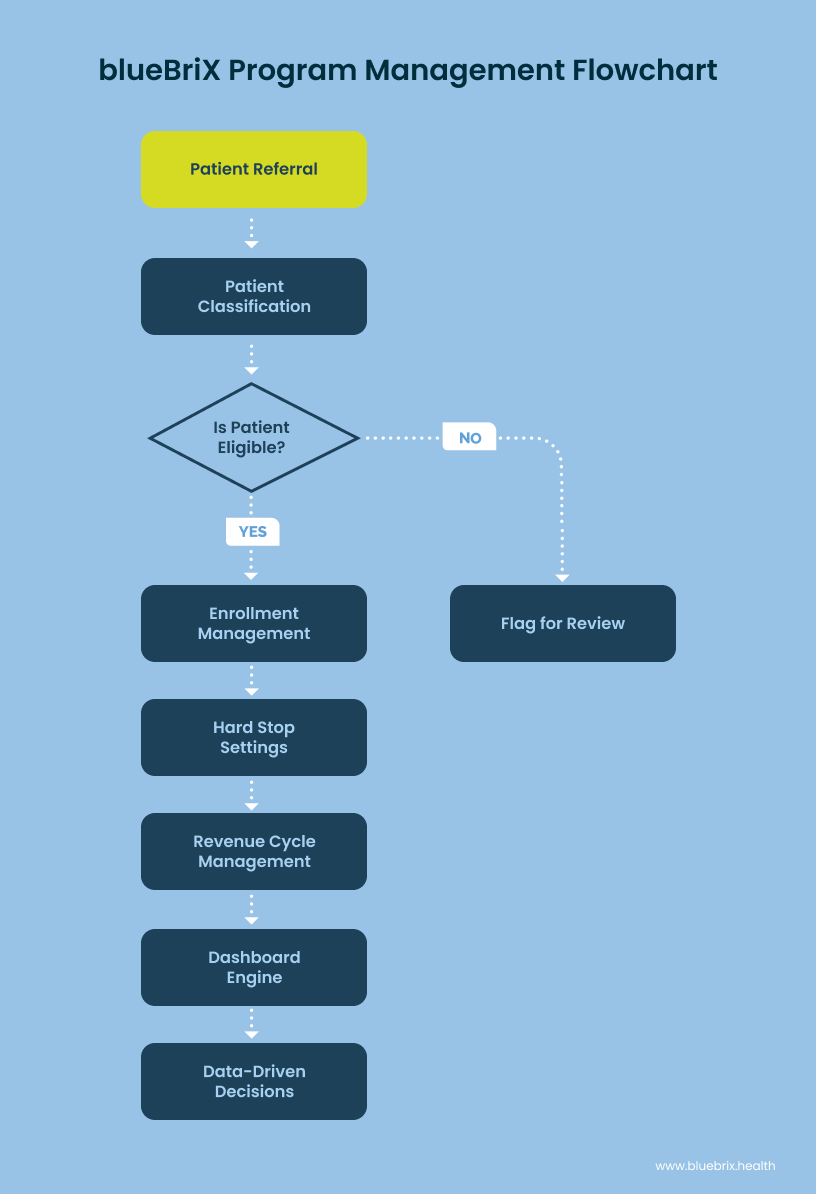
Bringing Patients In Smartly: Driving Engagement & Appropriate Care with Patient Classification and Enrollment Management
Let’s say a local school refers a teenager, Alex, who’s showing signs of severe anxiety. In value-based care, quickly identifying and engaging the right patients in the right programs prevents conditions from escalating, saving downstream costs. Before Alex even sets foot in your clinic, our Patient Classification feature activates. You’ve pre-defined criteria—perhaps specific diagnosis codes, age ranges, or social determinants of health indicators – to automatically identify if Alex is the ideal candidate for this specific high-impact youth program. This isn’t just about efficiency; it ensures you’re targeting interventions where they’ll have the greatest impact on population health and outcome metrics.
Once identified, Alex moves into Enrollment Management. This is more than just tracking a start date; it’s about managing a patient’s journey towards better health within a structured program. blueBriX’s multi-tier status system (like ‘Referred’ to ‘Initial Assessment Scheduled’ to ‘Active Enrollment’) drives efficient progression. As Alex moves through these stages, the system precisely tracks his care team, required documentation, and maintains a complete history. Crucially, if Alex’s initial assessment reveals he doesn’t meet specific, evidence-based health or age criteria you’ve set for this outcome-focused program, the system can automatically flag or even prevent his enrollment. This ensures program integrity from day one, so you’re only enrolling patients who are likely to benefit most, thereby maximizing your per-member-per-month (PMPM) effectiveness and quality measure attainment.
Orchestrating Care Teams with Precision: Enhancing Care Coordination & Patient Outcomes
Alex is now enrolled. How do you ensure his care is coordinated, preventing fragmented services? With Care Team Configuration, you build dynamic, multidisciplinary teams right within blueBriX. You’ve got his therapist, social worker, case manager, perhaps even a school liaison – all assigned with clear roles and supervisory relationships. If Alex’s primary therapist is on vacation, our ‘delegation’ feature lets you temporarily reassign tasks to another team member effortlessly. Every team action, from documentation to review workflows, is automatically tracked, providing a complete audit trail. This means seamless hand-offs, enhanced communication, and truly coordinated care that directly contributes to Alex’s improved outcomes and your organization’s ability to demonstrate collaborative care models to payers.
Ensuring Compliance with Hard Stop Settings: Protecting Revenue & Maintaining Program Integrity
In value-based care, billing for services that don’t meet program requirements can lead to costly clawbacks and audits. What if a provider accidentally tries to schedule Alex for a therapy session that’s outside the scope of his current program phase, or for which he’s no longer eligible? This is where Hard Stop Settings are invaluable. You can configure rules that literally ‘stop’ a provider from scheduling an appointment or performing a service if the patient doesn’t meet the specific program requirements at that exact moment. It’s a powerful built-in safeguard that prevents errors, ensures you remain compliant with stringent payer requirements, and fundamentally protects your revenue by preventing non-billable or non-compliant services.
Optimizing Your Financial Health with Revenue Cycle Management: Maximizing Reimbursement for Value
Sustaining quality care, especially for complex populations, requires robust financial health. Our integrated Revenue Cycle Management (RCM) system allows you to define all billing criteria directly within the program management engine. Whether your specific program contract is ‘Per Diem,’ ‘Fee For Service,’ ‘Grant-funded,’ or uses ‘CPT Rollup’ for bundled services that demonstrate a comprehensive episode of care, blueBriX handles it. This means accurate billing, streamlined authorization workflows that align with value-based care reimbursement models, and intelligent handling of non-billable codes. It simplifies the complex billing landscape, ensuring you maximize reimbursement for the value you deliver.
Gaining Real-Time Insights with the Dashboard Engine: Driving Performance & Data-Driven Decision Making
Finally, how do you prove the value you’re delivering? The Dashboard Engine is your command center for performance measurement. You can pull up a ‘Trackerboard‘ to visually see Alex’s progress through his treatment stages, track your ‘Schedule‘ for upcoming interventions, or check the ‘Insurance Status Management Dashboard‘ for any financial holds. These real-time dashboards provide instant operational awareness and actionable insights. You can quickly identify bottlenecks impacting patient flow or outcomes, understand overall program performance, and make data-driven decisions that directly impact both patient health and your clinic’s financial sustainability within value-based care. This visibility is key for demonstrating success to payers and improving your quality scores.