
This one’s for the healthcare heroes, the front-liners, who make life-saving decisions and deliver critical care when it matters most. You’re focused on your patients, and rightly so. But we know that behind the scenes, there’s a complex world of medical coding and billing that ensures your incredible work gets properly recognized and reimbursed.
One question we hear a lot, especially when patients move quickly from the Emergency Department (ED) to the Intensive Care Unit (ICU), is this: “Can we bill critical care in both the ED and ICU for the same patient on the same day?”
It’s a really important question, and frankly, it’s one that can lead to a lot of confusion and even missed revenue if not handled correctly. In fact, healthcare providers in the US lose an estimated $125 billion annually due to inefficient revenue cycle management, a staggering figure that underscores the importance of getting critical care billing right. At blueBriX, we get it. We’re here to help you navigate these tricky waters, so your organization can confidently capture every dollar earned for the life-saving care you provide.
Let’s break it down, cut through the jargon, and make sure you’re armed with the knowledge you need.
Critical Care: It’s About the Patient, Not Just the Room
First off, let’s clear up a common misconception: critical care isn’t defined by the physical room the patient is in. While the ICU is in its name, critical care happens wherever a critically ill patient is – the ED, a hospital floor, even during transport. What truly defines it is the patient’s condition and the intensive services you provide.
So, what does “critical care” really mean in the billing world? It means you’re directly delivering medical care to a patient who is in an immediate, life-threatening situation due to an acute impairment of one or more vital organ systems. Think about patients facing:
- Acute respiratory failure needing ventilation right now
- Severe sepsis with organ shutdown
- Cardiogenic shock where every second counts
- Major trauma with unstable vitals
The care you provide in these moments demands your full, undivided attention. You’re making high-stakes decisions, constantly monitoring, and actively supporting vital organ functions. This isn’t your routine check-up; it’s intense, focused, and absolutely critical.
The Codes: 99291 and 99292 – Time is Everything!
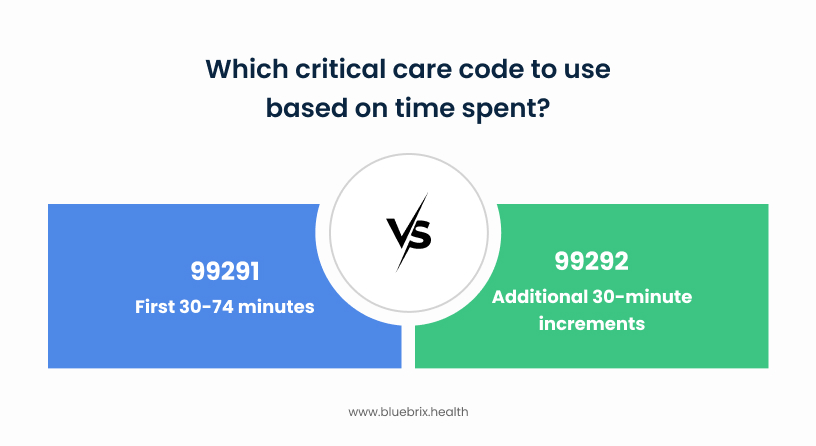
When it comes to billing for critical care, these are the primary codes you’ll see:
- 99291: This is for the first 30-74 minutes of critical care. This code can only be billed once per calendar day, per patient, per physician or same-specialty group.
- 99292: This is an “add-on” code, used for each additional 30 minutes of critical care after the initial 74 minutes. You’ll always see this linked to 99291.
The big takeaway here? Time, time, time! Critical care is all about the clock. The more precisely you document the time you spend, the better.
The ED and ICU Question: Yes, But With Rules!
Alright, the moment of truth. Imagine you’ve got a patient who rolls into the ED in crisis. You jump in, stabilize them, and then they’re quickly transferred to the ICU where the intensivists take over. Can both the ED doc and the ICU doc bill for critical care on the same day?
The straight answer is: YES, you can bill critical care services provided in both the ED and the ICU for the same patient on the same calendar day. However, it’s crucial to understand the rules. This isn’t a free-for-all, and adherence to guidelines is paramount to avoid denials and ensure compliance.
Here’s what you absolutely need to know:
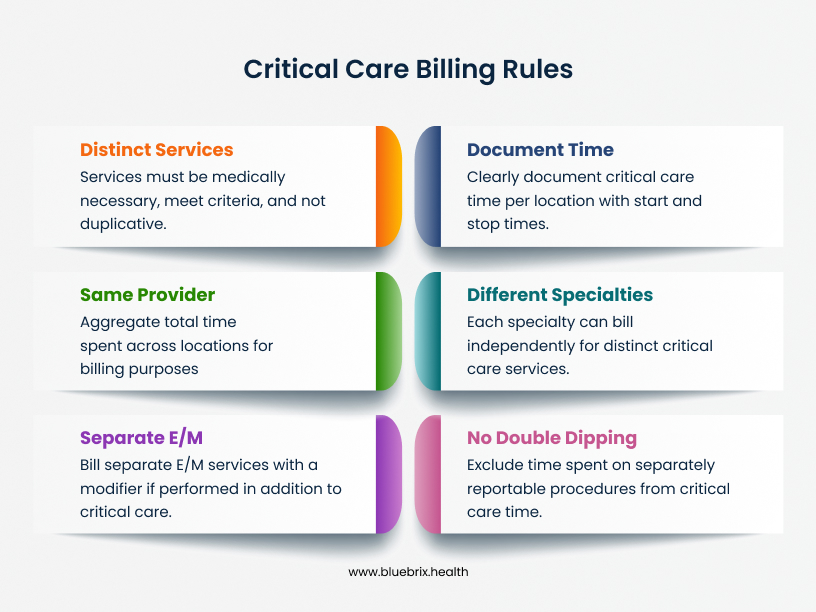
Distinct, Medically Necessary, and Non-Duplicative Services:
- Critical care can be provided and billed in both locations as long as the services are medically necessary, meet the strict criteria for critical care, and are not duplicative.
- For example, if a patient receives critical care in the ED (e.g., for acute respiratory distress) and is then transferred to the ICU where further distinct critical care is provided by a different provider/specialty (e.g., managing cardiogenic shock or specific organ system failure not previously addressed), both services may be billed if properly documented.
Document Time Per Location:
- Each location’s critical care time should be clearly documented, specifying the start and stop times and the medical necessity for the critical care provided in that specific setting. This means your ED notes should show ED critical care time, and ICU notes should show ICU critical care time.
Same Provider/Group? Aggregate Your Time!
- If the same provider (or providers in the same group/specialty) delivers critical care in both the ED and the ICU on the same calendar day, the total time spent across both locations should be aggregated.
- You will then bill using CPT codes 99291 (first 30-74 minutes) and 99292 (each additional 30 minutes).
- Important: Only one initial critical care code (99291) can be billed per group/specialty per calendar day for that patient, regardless of how many locations or individual providers within that group delivered the care. All subsequent time is billed with 99292.
- Split/Shared Critical Care: Good news! Since January 1, 2022, CMS allows for split/shared critical care services. This means the total time spent by both the physician and the Non-Physician Practitioner (NPP) in the same group is combined. The person (physician or NPP) who performs more than half of the total cumulative time bills for the service and appends modifier FS.
Different Specialties? Bill Independently (If Distinct!):
- If providers from different specialties are involved (e.g., an emergency physician in the ED and an intensivist in the ICU), each may bill for their own medically necessary, non-duplicative critical care services.
- The documentation must strongly support that the care provided by each specialist was distinct and possibly addressed different organ systems or problems. It’s not about two people doing the same thing; it’s about two different specialists managing different aspects of a complex critical patient.
Separate E/M + Critical Care? Yes, With a Modifier!
- If a separate and identifiable evaluation and management (E/M) service is performed in addition to critical care on the same day (such as an initial ED visit where the patient was not critically ill, and then later their condition deteriorates, prompting critical care), both services may be billed on the same day.
- Your documentation must clearly support this distinction – showing the initial E/M occurred before the critical state. When billing, the appropriate modifier, typically Modifier 25, should be appended to the E/M code to indicate it was a significant, separately identifiable service.
No Double Dipping on Time!
- This is huge: You absolutely cannot count time spent on separately reportable procedures as critical care time. If you intubate a patient (that’s a separate billable procedure, CPT 31500), that time must be excluded from your critical care time calculation.
- Also, if two of you from the same group are just chatting about a patient, only one of your times can count towards critical care.
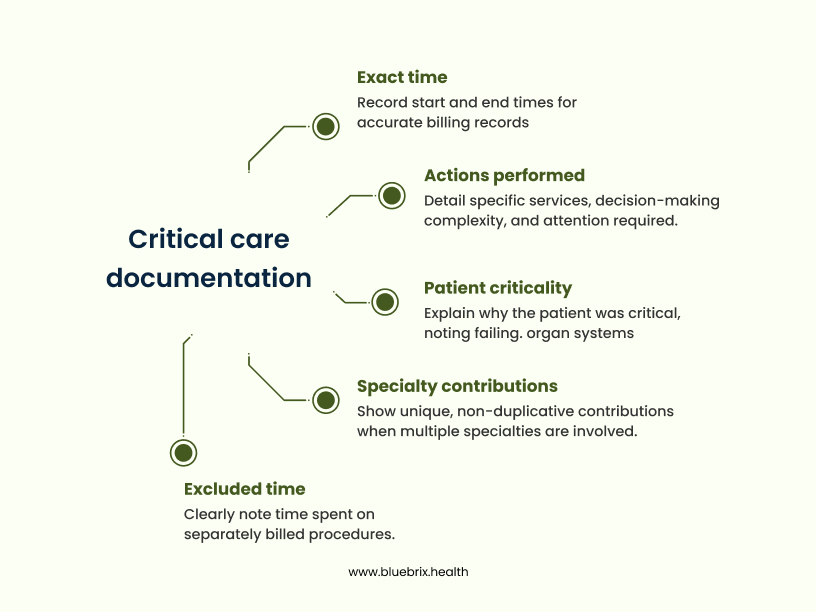
Documentation: Your Most Powerful Tool
Seriously, this can’t be stressed enough: Your documentation is the backbone of proper billing. For critical care, meticulous notes are non-negotiable. Your charts need to clearly back up:
- Why was the patient critical? What vital organ systems were failing? What was the high risk of life-threatening deterioration?
- The exact time! Write down start and end times, or the total cumulative time spent. “8:30 AM – 9:45 AM” is way better than just a total.
- What did you do? Detail the specific services you provided, how complex your decision-making was, and that it required your constant, undivided attention.
- What time was excluded? Clearly note if you spent time on procedures that are billed separately.
- If multiple specialties were involved, keep it clear: Each of your notes must distinctly show your unique, non-duplicative contributions.
Quick Stat: Did you know that claim denial rates can range from 10% to 25%, with each denial costing an average of $118 in administrative costs to rework? Incorrect critical care billing, often due to documentation errors, contributes significantly to these numbers.
It’s not just about lost revenue; compliance is key. The Centers for Medicare & Medicaid Services (CMS) reported an overall improper payment rate of 7.26% for Medicare Fee-for-Service in 2023, with billions attributed to issues like incorrect coding and insufficient documentation.
Common Traps to Steer Clear Of
- Don’t Assume: Just because a patient is in the ICU or ED doesn’t automatically mean it’s critical care. The patient’s condition and the services you provide must strictly meet the criteria.
- Be Specific: “Patient critically ill” isn’t enough. Spell out the specific organ failure(s) and why there was a high probability of life-threatening deterioration.
- Time Accuracy: Under- or over-documenting your time can lead to audits, denials, or even bigger headaches. Be precise!
- Bundling Errors: Some services are already included in the critical care bundle (like interpreting a chest X-ray or managing a ventilator). Don’t bill for them separately. Always double-check your CPT codebook.
- Modifier Misuse: Incorrectly using modifiers (like 25 for an unrelated E/M on the same day as a procedure) can cause denials.
How blueBriX Helps You on the Front Lines
We know you’re busy saving lives, not thinking about billing codes. That’s where blueBriX comes in. We support healthcare organizations across the globe, making sure that your incredible work is accurately coded and billed, so you can focus on your patients.
Here’s how we’re here for you:
- Expert Medical Coders: Our certified coders are absolute pros in the latest billing guidelines. They understand the nuances of critical care in any setting, ensuring accurate code assignment – meaning fewer errors and more appropriate reimbursement for the care you deliver.
- Smooth RCM: From verifying insurance to submitting claims and fighting denials, we streamline the entire process. This means less administrative burden on your organization and faster payments for the care you provide.
- Comprehensive Audits & Training: We review your documentation, spot potential compliance risks, and even provide targeted training to your team. Think of it as an extra layer of support, making sure your great care is perfectly reflected in the charts.
- Smart Technology: We use advanced tools and analytics to catch trends and predict potential denials, keeping your billing ahead of the curve.
In a healthcare world where every dollar counts, ensuring your critical care services are billed correctly is crucial. By understanding these guidelines, meticulously documenting your invaluable work, and partnering with RCM experts like us at blueBriX, your organization can be financially strong, compliant, and ultimately, keep doing what you do best: providing exceptional patient care. Our goal isn’t just to fix problems; it’s to transform your financial health.