The Transforming episode accountability model (TEAM) is a pivotal and ambitious development in the ongoing value-based care journey, particularly within the realm of surgical specialties. Launched by the Centers for Medicare & Medicaid Services (CMS), TEAM represents a bold and mandatory stride towards holding hospitals and their associated providers more comprehensively accountable for the entire patient journey encompassing specific, high-volume surgical procedures. It signifies a move beyond individual service payments to a more holistic view of surgical care.
This is a specific, mandatory payment initiative spearheaded by CMS, designed to fundamentally reshape how surgical care is reimbursed and delivered. The CMS TEAM model introduces a new layer of financial and quality accountability that spans beyond the operating room itself, compelling widespread participation and driving systemic change.
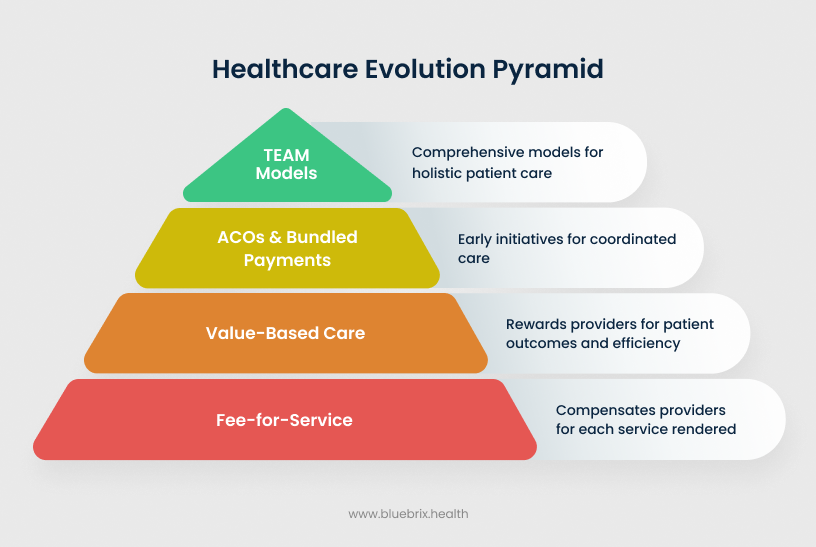
The fundamental purpose of TEAM is to directly confront and mitigate the pervasive fragmentation often observed in surgical care pathways. By establishing a single point of financial accountability for hospitals and their associated providers across an entire “episode” of treatment, CMS aims to achieve a trifecta of critical objectives:
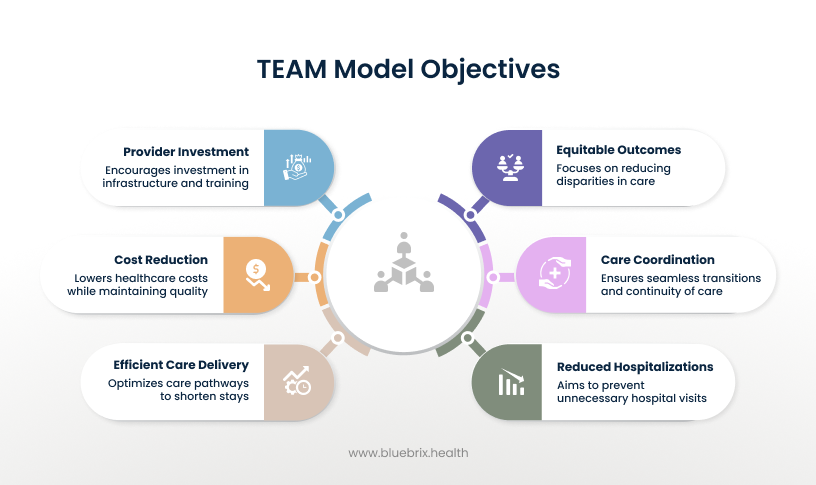
- Improve care quality: By linking payment to outcomes, TEAM incentivizes the adoption of evidence-based best practices, rigorous adherence to safety protocols, and proactive measures to reduce post-operative complications, infections, and adverse events.
- Coordinate Care: The model actively encourages seamless transitions and robust communication among all healthcare providers involved in a patient’s surgical journey – from pre-operative assessments to the inpatient stay, and crucially, through the post-acute recovery period. This integrated approach aims to reduce redundant tests, improve information exchange, and enhance patient safety.
- Control costs: By holding providers accountable for the total cost of an episode, TEAM drives efficiency and discourages unnecessary spending within the defined surgical period. This includes optimizing resource utilization, managing length of stay, and ensuring appropriate use of post-acute care services.
How does the TEAM model work?
TEAM’s operational framework is meticulously structured around the concept of a defined “episode of care” and a unique retrospective payment and reconciliation process. Under TEAM, an “episode of care” represents a comprehensive and financially accountable period of treatment for a specific surgical condition, extending beyond just the procedure itself.
Episode initiation: An episode officially begins with a Medicare beneficiary’s admission to an acute care hospital for an “anchor procedure” – the primary surgical intervention that triggers the episode. This can be either an inpatient hospitalization, or a qualifying outpatient procedure performed at a hospital outpatient department.
Episode duration: The episode then extends for a critical period of 30 days after the patient’s hospital discharge (or following the outpatient anchor procedure). This extended timeframe is strategically chosen because a significant portion of post-operative complications, readmissions, and critical recovery needs typically occur within this immediate post-discharge window. By including this period, TEAM compels providers to focus on the entire continuum of recovery, not just the acute phase.
Comprehensive inclusion: The episode’s financial scope is remarkably broad, encompassing nearly all Medicare Part A and Part B items and services directly related to the anchor procedure. This means that the total cost for the episode will factor in:
- Hospital inpatient care (including the DRG payment for the surgery)
- Physician services (surgical, anesthesia, and other specialists)
- Outpatient therapy services (e.g., physical, occupational, speech therapy)
- Skilled nursing facility (SNF) care
- Home Health services
- Related diagnostics (e.g., lab tests, imaging)
- Medications (Part B drugs)
- Durable Medical Equipment (DME)
- Any hospital readmissions or emergency department visits within the 30-day post-discharge period.
The fives surgical procedures covered in TEAM
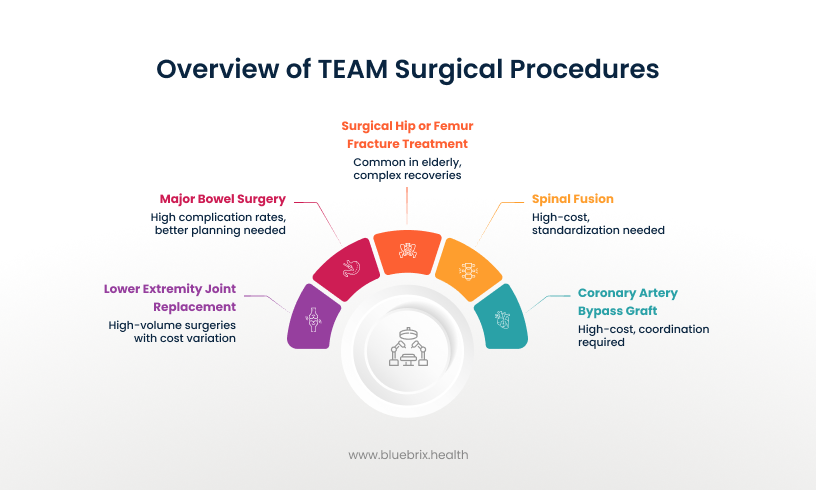
CMS has strategically selected five high-volume surgical procedures that are frequently performed on Medicare beneficiaries and often exhibit significant cost variation and opportunities for quality improvement. These are:
- Lower extremity joint replacement (LEJR): Includes common procedures like total hip and knee replacements. These are high-volume surgeries with substantial cost variation, particularly in post-acute care utilization. Previous bundled payment models have already demonstrated significant savings and quality improvements in this area, making LEJR a natural fit for TEAM.
- Surgical hip or femur fracture treatment (SHFFT): Covers procedures to repair hip and femur fractures, which are particularly prevalent in the elderly population and often lead to complex, lengthy recoveries and high post-acute care needs. TEAM aims to standardize care and reduce complications for this vulnerable group.
- Spinal fusion: A procedure joining vertebrae, often performed to treat spinal instability or degenerative conditions. Spinal fusions are high-cost procedures with wide variations in surgical approaches and significant post-operative care requirements, making them ripe for standardization and efficiency gains.
- Coronary artery bypass graft (CABG): A major cardiac surgery that improves blood flow to the heart. CABG is a high-cost procedure with a lengthy recovery and a notable risk of rehospitalization, necessitating strong coordination between cardiology, surgical, and rehabilitation teams.
- Major bowel surgery: Encompasses inpatient surgeries involving substantial resection or repair of the bowel. These procedures can have relatively high rates of complications and readmissions, presenting a clear opportunity for TEAM to drive better perioperative planning and discharge coordination.
These procedures were chosen due to their significant volume among Medicare beneficiaries, the substantial variation in spending and outcomes observed across different providers, and the potential for improved care coordination to reduce complications and costs. This makes them ideal candidates for a model designed to drive standardization, efficiency, and improved quality across a defined episode.
Payment mechanism and reconciliation process of TEAM
The financial accountability component is the cornerstone of TEAM, shifting risk and reward to participating hospitals. During the actual episode of care, hospitals and providers continue to bill Medicare under the traditional fee-for-service (FFS) system, as they normally would. After each performance year concludes (typically six months after the end of the year to allow for claims to run out), CMS performs an annual, retrospective reconciliation. They meticulously compare the hospital’s actual aggregate Medicare spending for all its TEAM episodes against a pre-determined target price for those same episodes. This retrospective nature means hospitals are accountable for costs already incurred.
The target price for each episode is calculated prospectively and is a complex undertaking. It’s based on a weighted three-year baseline of regional historical spending for the specific procedure. Crucially, it’s adjusted for patient-specific risk factors (e.g., comorbidities, age), case mix, and the location of care (inpatient versus outpatient). A discount factor (typically 1.5% to 3%) is also applied to ensure guaranteed savings for Medicare. This risk adjustment aims to create a fair comparison among hospitals treating different patient populations.
The reconciliation process determines the financial outcome for the hospital:
- Bonuses (Positive Reconciliation): If a hospital’s actual episode spending is below the calculated target price, and they meet specific quality thresholds, they can receive a reconciliation payment (a bonus) from CMS. This is their reward for delivering high-value, efficient care.
- Repayments (Negative Reconciliation): Conversely, if the hospital’s spending exceeds the target price, they may owe a repayment amount to CMS. This creates a strong financial incentive for efficient and high-quality care, as inefficient care directly impacts the bottom line. For example, if a hospital’s average episode cost is $35,000 and the target price is $32,000, they would owe CMS $3,000 per episode (subject to caps and quality adjustments).
The role of quality thresholds in reconciliation payments
Quality performance is not merely a suggestion; it is inextricably linked to financial outcomes. Hospitals must meet established quality measures to be eligible for full reconciliation payments or to mitigate potential repayments. These measures often include:
- Hospital-wide all-cause readmission (HWR) rates
- Complication rates (e.g., PSI 90, surgical site infections)
- Patient-reported outcome measures (PROMs) for specific procedures (e.g., THA/TKA)
- Patient experience scores (e.g., HCAHPS). This ensures that cost savings are not achieved at the expense of patient safety or quality of care.
Participation and timeline in TEAM
Who is Required to Participate (Hospitals, Regions)? Approximately 741 acute care hospitals located in 188 specific core-based statistical areas (CBSAs) across the US are required to participate. This broad inclusion is a strategic move by CMS to gather robust data, accelerate the adoption of value-based care principles across diverse markets, and overcome the selection bias often seen in voluntary models. Hospitals in these designated regions, unless explicitly excluded (e.g., Critical Access Hospitals), must participate.
The TEAM model officially commenced on January 1, 2026, and is slated to run for five years, concluding on December 31, 2030. This five-year period allows for sufficient time to test the model’s effectiveness and gather comprehensive data.
Participation tracks and varying levels of financial risk
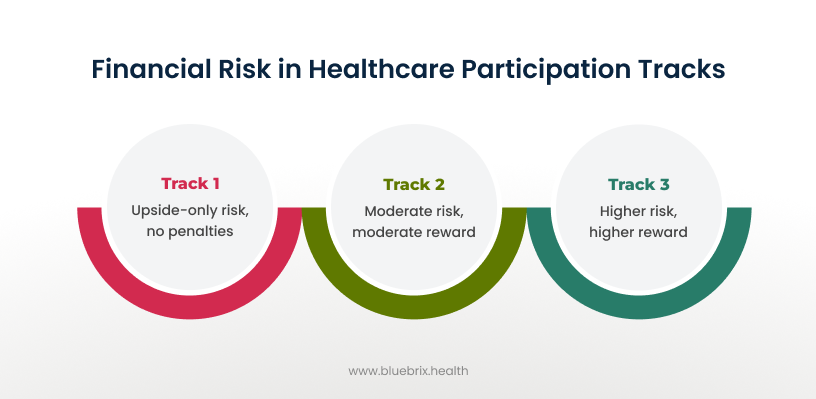
TEAM offers three participation tracks, allowing for varying levels of financial risk, which can be particularly beneficial for hospitals transitioning to value-based care.
- Track 1 (Upside-Only Risk): Available to all participants in Performance Year 1, and for up to three years for safety-net hospitals. Hospitals can earn bonuses if savings are achieved but face no repayment obligations to CMS. This serves as a “glide path” for organizations new to bundled payments.
- Track 2 (Moderate Two-Sided Risk): Offers both upside rewards and downside penalties, with financial risk capped at a moderate percentage (e.g., 5%). Certain hospital types (e.g., rural, Medicare-dependent) may be eligible for this track in later years.
- Track 3 (Higher Two-Sided Risk): Carries higher potential rewards but also higher potential penalties (e.g., up to 20%). This track is available to all participants for all five performance years, suitable for organizations more experienced in risk-based models.
Why TEAM is a game-changer for US surgical healthcare
-
Driving the shift from volume to value
TEAM’s financial structure is ingeniously designed to directly encourage efficiency without compromising, and indeed, while actively promoting quality.
- Reducing avoidable readmissions and complications: Since readmissions and complications within the 30-day episode directly increase the total cost of care for which the hospital is accountable, there’s a powerful financial incentive to implement evidence-based protocols to prevent these adverse events. This includes rigorous infection control, effective pain management, early mobility programs, and robust patient monitoring.
- Optimizing resource utilization across the episode: Providers will be highly motivated to scrutinize every aspect of resource use throughout the episode. This includes avoiding unnecessary diagnostic tests, redundant procedures, inappropriate specialist consultations, or prolonged inpatient stays. The focus shifts to delivering only necessary, high-value care, thereby optimizing the entire care pathway and reducing waste.
-
Fostering enhanced care coordination and collaboration
Fragmented care is a persistent and costly challenge in healthcare, often leading to medical errors, redundant services, and poor patient experiences. TEAM directly addresses this by:
- Breaking down silos between acute and post-acute care: The model incentivizes hospitals to establish robust relationships and work closely with their network of post-acute care providers, including skilled nursing facilities (SNFs), inpatient rehabilitation facilities (IRFs), and home health agencies. This collaboration ensures that patients receive appropriate, high-quality care even after they leave the hospital, reducing the likelihood of complications or unnecessary readmissions.
- Importance of seamless patient transitions: The 30-day post-discharge window is a particularly vulnerable and critical period for patient recovery. TEAM encourages meticulous discharge planning, comprehensive patient and caregiver education, and proactive follow-up mechanisms. The aim is to prevent adverse events, ensure medication adherence, and provide necessary support, thereby ensuring patients receive the right care at the right time and avoid costly, avoidable readmissions or emergency department visits.
-
Promoting cost containment and efficiency
TEAM’s financial structure is ingeniously designed to directly encourage efficiency without compromising, and indeed, while actively promoting quality.
- Reducing avoidable readmissions and complications: Since readmissions and complications within the 30-day episode directly increase the total cost of care for which the hospital is accountable, there’s a powerful financial incentive to implement evidence-based protocols to prevent these adverse events. This includes rigorous infection control, effective pain management, early mobility programs, and robust patient monitoring.
- Optimizing resource utilization across the episode: Providers will be highly motivated to scrutinize every aspect of resource use throughout the episode. This includes avoiding unnecessary diagnostic tests, redundant procedures, inappropriate specialist consultations, or prolonged inpatient stays. The focus shifts to delivering only necessary, high-value care, thereby optimizing the entire care pathway and reducing waste.
Challenges and opportunities for hospitals and providers under TEAM
Implementing a model as comprehensive and mandatory as TEAM undoubtedly presents its share of significant challenges. However, for organizations that strategically adapt and innovate, it also unlocks substantial opportunities for growth and leadership in the evolving healthcare landscape.
Potential challenges
- Operational restructuring and clinical redesign: Hospitals will need to undertake a comprehensive re-evaluation and fundamental redesign of their existing clinical pathways to align with the episode-based accountability. This requires significant cross-departmental collaboration, a willingness to challenge established norms, and robust change management strategies to ensure buy-in from all levels of staff.
- Investment in data analytics and technology infrastructure: Success under TEAM is heavily reliant on an organization’s ability to accurately track, analyze, and predict costs and outcomes across the entire episode. This necessitates substantial investment in advanced data analytics capabilities, platform built electronic health record (EHR) systems, and potentially new technology solutions that can provide actionable insights, not just raw data. Without this, identifying areas for improvement and measuring progress will be nearly impossible.
- Aligning diverse stakeholders and care teams: Bringing together a multitude of diverse stakeholders – including surgeons, anesthesiologists, nurses, therapists, post-acute care providers, and administrative staff – to work cohesively towards common goals under a new payment model can be incredibly complex. There may be initial resistance to changes in workflow, communication styles, and established practices.
- Navigating financial risk: For hospitals participating in Tracks 2 and 3, the potential for repayment to CMS if costs exceed targets introduces a new layer of financial risk. This requires sophisticated financial planning, robust risk mitigation strategies (such as strong care management programs and preferred provider networks), and a clear understanding of their cost structures.
Significant opportunities
- Earning financial incentives for high-value care: Hospitals that successfully manage episode costs below the target price while maintaining or improving quality can earn substantial reconciliation payments. These bonuses represent a significant new revenue stream that can be reinvested into further care improvements, technology, or staff development.
- Enhancing reputation and market competitiveness: Demonstrating consistent success under the TEAM model, particularly in terms of quality outcomes and cost-efficiency, can significantly bolster a hospital’s reputation. This can attract more Medicare beneficiaries seeking high-value care and strengthen the hospital’s competitive position within its market.
- Strengthening provider networks and partnerships: TEAM fosters deeper collaboration and integration between hospitals and their broader network of referring physicians and post-acute care providers. This leads to the development of highly integrated care delivery systems, characterized by shared goals, improved communication, and a collective commitment to patient outcomes.
- Achieving long-term sustainability and growth: By driving internal efficiencies, optimizing care pathways, and reducing avoidable costs, TEAM can help healthcare organizations achieve greater financial stability and resilience. This positions them for sustainable long-term growth in an increasingly value-based healthcare environment, making them more attractive partners and employers.
Key strategies for success with TEAM
For hospitals and providers located in the mandatory regions, proactive and strategic preparation is absolutely essential for successful participation and maximizing the benefits of TEAM. Here are a few core strategies to look into:
Conduct a baseline performance assessment (Cost and Quality)
The first critical step is to gain a granular understanding of current performance. Hospitals must meticulously analyze their historical Medicare claims data for the five covered procedures. This assessment should pinpoint:
- Average episode costs: Identifying current spending patterns and high-cost drivers.
- Readmission rates: Understanding the frequency and causes of unplanned re-hospitalizations.
- Complication rates: Tracking surgical site infections, adverse events, and other post-operative issues.
- Patient satisfaction scores: Gauging the patient experience through surveys like HCAHPS. This baseline will serve as a crucial benchmark and identify specific areas ripe for improvement and intervention.
Implement robust care coordination and pathway standardization
Developing and implementing standardized, evidence-based care pathways for each of the five surgical procedures is paramount. This involves establishing consistent approaches across the entire patient journey:
- Pre-operative optimization programs: Ensuring patients are in the best possible health before surgery to reduce risks.
- Intra-operative best practices: Standardizing surgical techniques and protocols.
- Post-operative recovery protocols: Implementing consistent approaches to pain management, mobility, and discharge readiness.
- Dedicated care navigators or coordinators: Assigning personnel to guide patients through their entire episode, ensuring seamless transitions and addressing needs.
- Enhanced communication protocols: Establishing clear channels for information exchange between all care team members across different settings.
Prioritize data-driven decision making
Success under TEAM is inherently data-driven. Hospitals must cultivate a culture of continuous analysis and improvement by:
- Effectively monitoring episode spending and key quality metrics.
- Identifying inefficiencies and cost drivers within care pathways.
- Proactively recognizing and managing patients at high risk for adverse events or readmissions.
- Continuously benchmarking performance against internal goals and external averages to inform strategic adjustments.
Educate and engage all clinical and administrative staff
A successful transition to TEAM requires a unified effort and shared understanding across the organization. It’s vital to:
- Provide comprehensive education: Ensure that all staff members, from surgeons and nurses to administrative and billing personnel, thoroughly understand the TEAM model, its implications, and their specific roles in achieving its objectives.
- Foster a culture of accountability and collaboration: Emphasize shared responsibility for patient outcomes and episode costs.
- Identify physician champions: Engage influential surgeons and clinical leaders who can advocate for and drive adherence to new protocols and care pathways.
Develop strong partnerships with post-acute care providers
Given the 30-day post-discharge accountability, strong relationships with post-acute care providers are non-negotiable. Hospitals should:
- Identify high-quality, cost-effective partners: Select skilled nursing facilities, home health agencies, and rehabilitation centers that consistently deliver excellent outcomes.
- Establish clear communication channels: Ensure seamless information exchange and coordinated care plans.
- Implement shared performance metrics: Work with partners to track and improve outcomes across the entire episode, not just within their individual settings.
The role of technology in mastering TEAM compliance
Navigating the complexities of TEAM isn’t solely about clinical redesign—it also involves significant data and technology considerations. Given its mandatory nature, retrospective reconciliation, and broad episode scope, having a solid technological foundation is increasingly important. Without the right systems in place, hospitals and providers may struggle to meet quality benchmarks, manage costs effectively, or identify areas for improvement.
Here’s why technology is paramount in enabling the strategies for TEAM compliance and optimizing performance:
- Aggregating disparate data into a single source of truth: TEAM requires a holistic view of the patient journey, encompassing data from inpatient stays, physician services, post-acute care (SNFs, home health), labs, imaging, and even medications. Traditional, siloed systems make this unified view nearly impossible. Advanced technology solutions are essential to seamlessly integrate data from various EHRs, claims systems, and external sources into a single, cohesive patient record. This integrated data forms the foundation for accurate episode costing and quality monitoring.
- Enabling precision in episode costing and performance measurement: The financial reconciliation under TEAM is meticulous. Hospitals need the ability to track every single service and item related to an episode, attribute costs accurately, and compare them against target prices. This demands sophisticated cost accounting and analytics capabilities. Technology platforms can automate the aggregation of relevant claims data, apply the intricate rules of episode bundling, and provide precise calculations of actual vs. target spending in real-time or near real-time.
- Facilitating proactive risk identification and management: Waiting for a retrospective reconciliation report to identify high-cost episodes or quality shortfalls is too late. Effective TEAM compliance requires predictive analytics and AI. These technologies can analyze integrated clinical and SDOH data to identify patients at high risk for complications, readmissions, or excessive resource utilization before these events occur. This allows care teams to intervene proactively, adjust care plans, and deploy targeted support, thereby mitigating financial risk and improving patient outcomes.
- Streamlining seamless care coordination and communication: The 30-day post-discharge period is a critical window for TEAM accountability. Technology can bridge communication gaps between acute care hospitals, referring physicians, and post-acute care providers. This includes:
- Shared care plans: digital platforms enable the creation and sharing of comprehensive, dynamic care plans accessible to all members of the care team.
- Secure messaging and alerts: Real-time communication tools facilitate timely updates, alerts for changes in patient status, and coordinated decision-making.
- Patient engagement tools: Portals, remote monitoring, and educational modules empower patients to actively participate in their recovery, improving adherence to care plans and reducing avoidable complications.
- Powering benchmarking and continuous improvement: To truly excel under TEAM, organizations must continuously assess their performance against benchmarks and identify areas for improvement. Technology provides the tools for:
- Performance dashboards: Visualizing key performance indicators (KPIs) related to cost, quality, and outcomes.
- Root cause analysis: Drilling down into data to understand why certain episodes are more costly or have worse outcomes.
- Trend analysis: Identifying patterns over time to refine care pathways and optimize resource allocation.
In essence, successful TEAM participation hinges on an organization’s ability to transform vast amounts of data into actionable intelligence. This is where specialized healthcare technology solutions become invaluable partners, equipping hospitals and providers with the foresight and precision needed to thrive in this new value-based paradigm.
How blueBriX supports TEAM model compliance for providers & healthcare organizations
At blueBriX, we understand the demands of TEAM and have engineered our platform to be a cornerstone for successful compliance and operational excellence. We bridge the gap between complex regulations and seamless care delivery, ensuring you’re not just ready for TEAM, but positioned to excel.
Here’s how blueBriX empowers your organization to master TEAM compliance by directly addressing the technological needs highlighted above:
1. End-to-end workflow automation for precision & efficiency
blueBriX provides the automation necessary to standardize and manage the complex, multidisciplinary workflows central to TEAM:
- Customizable care pathways: Design flexible, compliant workflows tailored for diverse patient populations and the specific surgical episodes covered by TEAM, ensuring consistent, high-quality care delivery.
- Dynamic forms & data capture: Utilize custom documentation templates that capture every minute detail required for regulatory reporting and quality metrics, significantly reducing manual errors and preventing missed data points, crucial for accurate episode costing and auditing.
- Multi-role task management: Assign tasks precisely to the right teams—from RNs and surgeons to care coordinators—with real-time progress tracking and automated alerts for any missed care steps, fostering coordinated action across the entire care continuum.
2. Seamless compliance & quality monitoring, built-in
Compliance isn’t an afterthought with blueBriX; it’s embedded into the platform’s core, giving you peace of mind and audit readiness:
- Built-in compliance frameworks: Our platform supports HIPAA, GDPR, and other essential healthcare standards. We provide regular updates to maintain alignment with evolving regulatory requirements, including those central to TEAM.
- Audit-ready reporting: Access automated and customizable compliance dashboards that offer instant access to critical quality metrics (such as readmission rates, patient safety indicators, and patient satisfaction scores) and comprehensive submission trails, making proving adherence during CMS audits straightforward and stress-free.
- Automated rule enforcement: Program management rules, often referred to as “hard stops,” proactively prevent non-compliant activities. This could include blocking billing events if required documentation is incomplete or preventing workflows from advancing without necessary patient conditions being met, ensuring every action is TEAM-compliant.
3. Integrated care coordination for a unified patient journey
TEAM’s emphasis on comprehensive episode management demands unparalleled care coordination, which blueBriX facilitates through:
- Unified patient records: Our platform integrates seamlessly with your existing EHRs, telehealth solutions, scheduling, and billing systems, creating a consolidated, up-to-date patient view across all points in the surgical episode, from pre-op to post-discharge.
- Real-time alerts & engagement: blueBriX detects and flags potential gaps in care, triggers automated reminders for crucial post-discharge follow-ups, and tracks patient engagement against required milestones, supporting compliance with TEAM quality incentives.
4. Advanced analytics & reporting for TEAM metrics
Understanding your performance against TEAM’s demanding metrics is vital for financial success and quality improvement, which blueBriX provides through:
- Performance dashboards: Visualize your progress on all critical TEAM measures—including episode costs, quality benchmarks, readmission rates, and patient-reported outcomes. These actionable dashboards empower your teams to quickly identify trends and act on data to meet incentive thresholds.
- Configurable reports: Easily export or automate regulatory submissions in formats specifically compliant with CMS and TEAM reporting requirements, eliminating manual data extraction and significantly reducing audit preparation stress.
5. Enterprise-grade security and seamless interoperability
Protecting sensitive patient data and ensuring smooth data flow are foundational to any modern healthcare operation.
- Enterprise-grade data security: With robust features like role-based access controls, Single Sign-On (SSO), and HIPAA/SOC2 compliance, blueBriX protects sensitive patient and operational data throughout all TEAM episodes.
- API & interoperability: Our platform supports FHIR, HL7, and other industry standards, enabling smooth, bidirectional integration with your existing health IT systems. This is critical for organizations adapting their infrastructure to the complex data exchange needs of TEAM.




