“A good navigation guide is like a compass in the unknown; it provides direction and clarity, ensuring you reach your destination even when the path is unclear.”
Patient navigation in value-based care
Let’s understand the role of patient navigation in healthcare with an example:
John, a 45-year-old father of two, had been feeling unusually fatigued for weeks. Lately, he also noticed some unexplained weight loss and persistent discomfort in his abdomen. These symptoms gnawed at him, raising a terrifying question in his mind: Could this be cancer?
Unsure of what steps to take, he hesitated to visit the doctor, overwhelmed by the potential diagnosis and the complexity of navigating medical consultations. “I just wish someone could guide me,” John thought, “someone who could help me understand my symptoms and point me in the right direction.” He longed for a support who could make the journey less intimidating, ensuring he received timely and proper care.
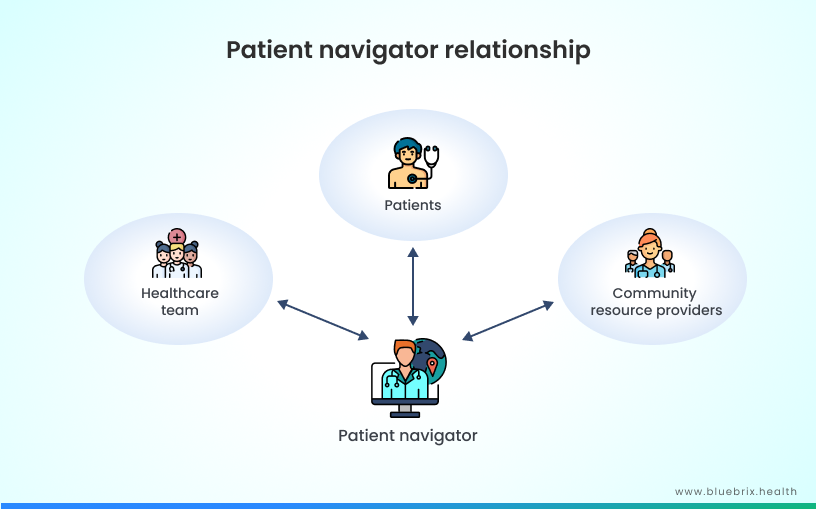
A patient navigator could guide patients like John through the complexities of the healthcare system, ensuring he receives timely consultations, appropriate tests, and emotional support during his journey to diagnosis and treatment, easing both his anxiety and decision-making process.
Patient navigation programs have significantly reduced care gaps and improved treatment access, especially for patients with chronic conditions like cancer. Research shows that patient navigation is critical in streamlining access to timely diagnosis and care by reducing barriers to services and improving outcomes for underserved populations. In the value-based care model, where healthcare providers are rewarded for quality over quantity, patient navigation plays a pivotal role. By guiding patients through complex care pathways and ensuring they receive the right care at the right time, navigation ensures better outcomes, reduces healthcare costs, and enhances patient satisfaction.
In this article, let’s explore how providers can enhance this navigation through seamless workflow automation, personalized treatment plans, and secure data sharing, aligning care teams and patients more effectively than ever before with patient navigation.
What is patient navigation?
Patient navigation refers to the process of guiding patients through the complex healthcare system, ensuring they receive timely care and the necessary support to make informed decisions. Patient navigators help individuals access appropriate healthcare services, manage treatments, and overcome barriers such as financial, language, or logistical challenges. Initially developed for cancer care, this concept has expanded to other chronic conditions, improving patient outcomes through personalized assistance and care coordination.
How is patient navigation relevant in value-based Care?
In Value-Based Care, patient navigation plays a crucial role by improving care coordination and reducing barriers that patients face when navigating complex healthcare systems. In a VBC model, the focus is on patient outcomes, and patient navigators ensure timely access to care, help manage chronic conditions, and reduce unnecessary services. By guiding patients through their care journey, they help achieve better health outcomes, increase patient satisfaction, and lower healthcare costs, aligning with the goals of VBC.
The principles of patient navigation
The principles of patient navigation focus on eliminating barriers to care and ensuring timely access to healthcare services. The key principles include:
- Elimination of barriers: The primary goal of patient navigation is to identify and remove barriers (financial, social, or logistical) that prevent patients from accessing timely care.
- Timely access to care: Patient navigation aims to ensure that patients receive appropriate care in a timely manner, from diagnosis through treatment and follow-up.
- Patient-centered care: Navigation is focused on the specific needs of the patient, ensuring culturally sensitive care tailored to each individual.
- Guidance across the care continuum: Patient navigation supports patients throughout their entire healthcare journey, coordinating care between different providers and healthcare systems.
- Collaboration: Navigators work with healthcare teams, social workers, and other professionals to ensure integrated care for patients.
- Cross-system navigation: Navigators must assist patients in transitioning between disconnected care systems, such as from primary care to specialized treatment.
- Coordination: A well-coordinated navigation system is essential for effective patient care, ensuring all care providers and services are aligned.
- Cost-effective delivery: The services provided should be aligned with the navigator’s training and skills, ensuring efficient and effective care without unnecessary expenses.
- Clear scope of practice: Patient navigation must be defined with a clear scope, distinguishing the navigator’s role from other healthcare providers, ensuring everyone understands their responsibilities.
- Skills determination: The complexity of each phase of care should dictate the level of skills required by the navigator, ensuring the right expertise is available at each step.
- Defined start and end: It is important to establish when patient navigation begins and ends within the care continuum, offering patients clear guidance.
- Trust and communication: Building trust and effective communication between the patient, navigators, and the care team is critical for success in patient navigation.
Key components of patient navigation
Key components of patient navigation include personalized support, care coordination, education, and resource connection. These elements help ensure that patients receive the right care at the right time, improving health outcomes and satisfaction, particularly in vulnerable populations like cancer and HIV patients. Let’s look at some of these key components in detail:
- Assessment of individual needs and barriers: Identifying personal health and social challenges that may prevent patients from accessing timely care. This includes financial, logistical, and emotional barriers.
- Education: Educating patients about their diagnosis, treatment options, and overall health. It also involves community outreach to spread awareness about healthcare services and preventive care.
- Coordination of care: Linking patients with various healthcare providers and resources, ensuring continuity of care across primary, secondary, and specialized care settings.
- Appointment scheduling and reminders: Assisting with booking appointments and sending reminders to ensure patients do not miss crucial treatments or consultations.
- Emotional and social support: Offering emotional guidance and linking patients to social services like financial aid, transportation, or housing support.
- Facilitation of referrals: Ensuring that patients are referred to the correct healthcare providers in a timely manner to receive the appropriate care.
The role of navigators
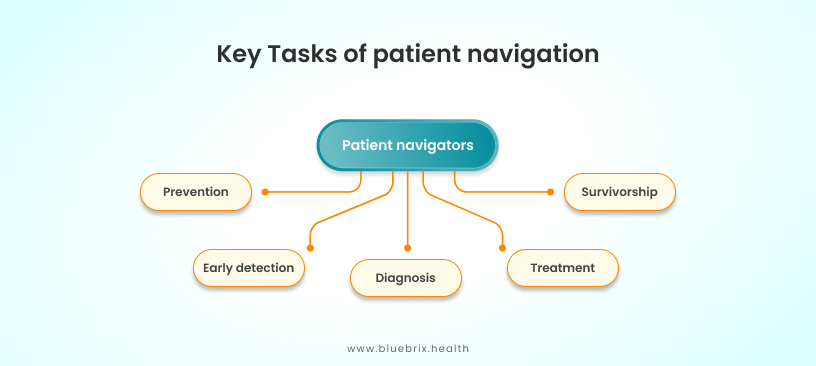
Patient navigators perform a range of critical tasks to support the patient journey through healthcare systems. They focus on:
- Identifying individual needs and barriers to care: Navigators assess the personal health and social needs of each patient, ensuring that they receive the right services.
- Educating patients and communities: Navigators play an important role in informing patients about their conditions and treatments, as well as educating the broader community on health resources and preventive care.
- Linking patients with providers: They coordinate across different levels of healthcare, ensuring smooth transitions between primary care, specialists, and other services.
- Making appointments and setting reminders: Navigators assist patients with scheduling appointments, ensuring they attend consultations and treatments, while also sending reminders to reduce missed appointments.
Key tasks of patient navigation
- Health and social needs assessment: Identifying patient needs to ensure comprehensive care.
- Barrier identification: Recognizing and overcoming individual and systemic obstacles to healthcare access.
- Coordination and communication: Acting as a liaison between patients and various healthcare and social services providers to enhance continuity of care.
- Facilitation of referrals: Helping patients navigate complex referral processes to access necessary treatments or specialists.
- Appointment scheduling and follow-up: Ensuring that patients keep track of their appointments and providing follow-up support.
- Self-management support: Empowering patients to manage their own health effectively, providing them with tools and information to take an active role in their care.
- Outreach and education: Conducting community outreach programs to inform patients and communities about health services, preventive care, and available resources.
- Translation and interpretation: Offering translation services to bridge language barriers, ensuring patients understand their treatment options and care plans.
- Emotional and social support: Navigators provide patients with emotional reassurance and connect them with social support services like transportation, financial aid, or housing assistance.
By focusing on these components, patient navigation ensures that patients receive holistic care that addresses not only their medical needs but also the social determinants of health that may impact their outcomes.
Who implements patient navigation?
Patient navigation can be implemented by a wide range of healthcare providers and organizations:
-
- Primary care providers: Clinics and healthcare centers focused on preventive care and chronic disease management can integrate patient navigators to enhance care coordination.
- Hospitals and health systems: Large health systems, including cancer centers and hospitals, use patient navigation to guide patients through complex treatment plans, especially for oncology and chronic diseases.
- Community-based health programs: Organizations like community health centers and substance use prevention programs use patient navigation to help patients navigate barriers to care, including social services and mental health support.
- Public health agencies: Governmental agencies, such as HIV care programs, utilize patient navigation to ensure vulnerable populations receive timely and appropriate care.
- Accountable care organizations (ACOs): ACOs implement patient navigation to enhance care coordination and improve patient outcomes. Navigators within ACOs help identify care gaps, connect patients with necessary services, and facilitate communication among providers, thereby reducing hospital readmissions and ensuring timely interventions.
- On-site clinics: On-site clinics utilize patient navigators to streamline access to healthcare for employees. These navigators assist in scheduling appointments, providing education on available services, and ensuring that employees understand their care plans, which improves overall health engagement.
- Medicare advantage: Medicare Advantage plans often include patient navigation services as part of their offerings. Navigators help seniors understand their benefits, navigate complex healthcare decisions, and access the resources they need to manage their health effectively.
- Oncology and other disease-specific navigation: In oncology, patient navigators play a crucial role in guiding patients through their cancer treatment journey. They assist with scheduling appointments, managing treatment side effects, and providing emotional support, thereby improving adherence to treatment plans. Disease-specific navigation also applies to chronic conditions such as diabetes or heart disease, where navigators help coordinate care across various specialties.
- Transitional care: Patient navigators are instrumental in transitional care, which involves the process of moving patients from one care setting to another, such as from hospital to home. They ensure patients have the necessary follow-up appointments and resources, reducing the risk of complications and readmissions.
- Employers: Employers are increasingly implementing patient navigation services to promote employee health and reduce healthcare costs. By offering navigators, companies can help employees better manage their healthcare needs, improve access to services, and foster a healthier workforce.
- Medicaid: Medicaid programs frequently incorporate patient navigation to assist beneficiaries in accessing healthcare services. Navigators help Medicaid recipients understand their benefits, connect with healthcare providers, and overcome barriers to care, ultimately aiming to improve health outcomes in underserved populations.
Patient navigation in private and public systems
The differences between patient navigation in public and private healthcare systems can be significant, impacting how services are delivered and the overall patient experience:
| Focus area | Public | Private |
|---|---|---|
| Accessibility and resource availability | Patient navigation in public healthcare often aims to address systemic barriers to care, such as long wait times and limited resources.Navigators may work to connect patients to available services within a strained system, often prioritizing underserved populations. | In contrast, patient navigation in private healthcare typically emphasizes efficiency and personalized service. Navigators may have more resources at their disposal, allowing for quicker access to diagnostics and treatments, as well as streamlined processes. |
| Focus and approach | Navigators in public systems often focus on managing complex cases and ensuring equitable access to care. They may work with a broader range of community resources and services, including social services and public health initiatives, to address patients’ comprehensive needs. | In private settings, the focus may be more on enhancing patient satisfaction and optimizing the care experience. Navigators often facilitate communication between patients and providers, assist with insurance processes, and ensure that patients adhere to treatment plans. |
| Funding and accountability | Funding for navigation services in public systems is often derived from government programs or grants, which can influence the scope of services offered and the number of navigators available. | In private healthcare, funding typically comes from the healthcare organization itself, which may allow for more flexibility and innovation in navigation services but can also lead to variations in quality and availability based on the organization’s priorities. |
| Training and expertise | Patient navigators in public systems may have diverse backgrounds, including community health workers and social workers, emphasizing cultural competency and community engagement. | Navigators in private settings may have formal healthcare training (such as nursing or healthcare administration), focusing on clinical pathways and organizational efficiency. |
These distinctions highlight how the environment and structure of the healthcare system can shape patient navigation services and their effectiveness in supporting patients throughout their care journey.
Who benefits from patient navigation?
Patient navigation benefits a wide range of individuals, especially those facing complex healthcare systems and barriers to care. These include:
- Patients with chronic conditions: Those with cancer, diabetes, and other long-term illnesses often struggle with navigating multiple providers and treatments. Patient navigators streamline their care and ensure timely access to necessary services.
- Vulnerable populations: Individuals from underserved communities, including racial and ethnic minorities or low-income patients, can benefit from patient navigation to overcome financial, social, or logistical barriers to healthcare access.
- Elderly patients: Older adults, who may struggle with the complexity of healthcare systems, can benefit from navigation that helps coordinate their care, manage medications, and attend appointments.
- Patients needing preventive care: Those requiring screenings or preventive treatments benefit from guidance to ensure timely interventions and adherence to care plans, which helps in preventing disease progression.
- Uninsured and underinsured patients: These individuals often face barriers to accessing care and rely on patient navigators to coordinate services and find affordable healthcare options.
Factors influencing patient navigation
Several factors influence the effectiveness and implementation of patient navigation programs, including:
- Resource availability: Adequate human, financial, and organizational resources are essential for the successful implementation and maintenance of patient navigation programs.
- Patient characteristics: Individual patient needs, including cultural, socioeconomic, and health literacy levels, can affect how navigators interact with patients and tailor their support.
- Healthcare system structure: The design and organization of the healthcare system, including integration between services, can impact the efficiency of navigation efforts. Systems that facilitate communication and collaboration among providers enhance navigation.
- Training and skills of navigators: The level of training and the skills possessed by patient navigators are crucial. Well-trained navigators can more effectively address barriers and provide appropriate support to patients.
- Community resources: Availability of community resources and services can support patient navigators in connecting patients with additional support and resources they may need.
- Policy and regulation: Local and national healthcare policies, including those related to funding and service delivery, influence how patient navigation programs are structured and operated.
- Inter-professional collaboration: Effective teamwork and collaboration among healthcare providers and organizations enhance the navigation process, allowing for a more comprehensive approach to patient care.
- Financial resources: Patient navigation programs need consistent funding sources. Securing external funding through grants, operational budgets, or other financial streams ensures sustainability and the ability to meet program goals.
- Appropriate space for navigator and navigation work: Physical infrastructure, such as a dedicated space for navigators, is essential to ensure privacy for patient discussions and efficient workflow.
- Technological resources:
- Internet resources to locate resources and support complex cases: Access to internet tools allows navigators to find community resources and support patients, particularly in complex cases that require external services.
- Electronic health records (EHR) to support documentation of evidence-based care plans, patient assessments: EHRs are crucial for creating, storing, and accessing patient care plans, ensuring consistency and improving care coordination.
- EHR to support access to community resources, coordinate transitions, and promote self-management: EHRs enable navigators to link patients to community resources, assist with care transitions, and provide tools to encourage self-management.
- Email or phones to support communication with physicians: Effective communication tools such as email and phones allow navigators to easily coordinate with healthcare providers, ensuring timely responses to patient needs.
- Adequate time for transitional care: Navigators need sufficient time to follow up with patients, coordinate complex transitions, and manage larger caseloads effectively.
- Strong inter and intra-organizational relationships/partnerships: Strong relationships and partnerships between organizations help streamline patient care, allowing resources to be shared and enabling better care coordination across different healthcare settings.
- Lack of available services in a community: Some communities may lack key healthcare services or resources, presenting a significant barrier to patient care. Navigators must be resourceful in helping patients find alternative solutions when local services are unavailable.
- Effective communication between providers: Efficient communication between providers across different settings ensures that patients experience seamless transitions in care and that all stakeholders are informed of care plans and changes in patient conditions.
- Program uptake and buy-in by end users: The success of navigation programs depends on the buy-in from healthcare providers, patients, and other stakeholders. Encouraging active participation and integrating the program into the healthcare culture is crucial for uptake.
- Valuing navigators: Organizations should recognize the role of patient navigators as vital to patient care. Ensuring that navigators are valued and supported by their teams fosters motivation and retention.
- Evaluation of navigation programs: Continuous evaluation of navigation programs using metrics such as patient outcomes and satisfaction helps assess program effectiveness and identify areas for improvement.
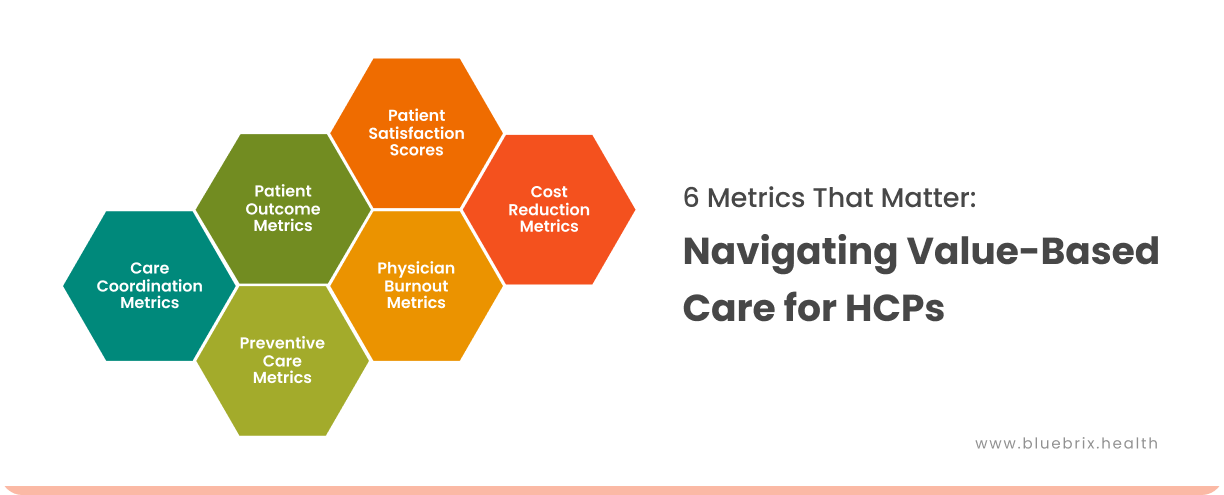
Key benefits of patient navigation programs

Key challenges in patient navigation
Patient navigation faces various challenges at the micro, meso, and macro levels:
- Micro-level challenges: These occur at the individual patient and navigator interaction level. Issues include communication barriers, lack of trust, and limited health literacy, making it difficult for patients to follow care plans or fully understand their healthcare options.
- Meso-level challenges: These relate to organizational factors within healthcare systems. Problems include fragmented care coordination, lack of integration between healthcare providers, and insufficient training for navigators to handle complex patient needs.
- Macro-level challenges: These are broader systemic issues, including inadequate policy support, insufficient funding for navigation programs, and a lack of standardized regulations. These create disparities in access to patient navigation services across different regions and healthcare settings.
The role of technology in enhancing care coordination and patient engagement
Technology plays a pivotal role in transforming healthcare by streamlining care coordination and improving patient engagement. Key innovations like secure messaging, telehealth, and integrated documentation systems are fostering better communication between patients and providers, ultimately leading to improved health outcomes.
Information and communication technologies (ICT)
ICT enables seamless information sharing between healthcare providers and patients, enhancing coordination and engagement. For example, electronic health records make patient data accessible across various care settings, improving the efficiency of clinical decision-making. ICT also supports self-management by allowing patients to track their health via apps and portals. For instance, diabetic patients can monitor their glucose levels using smartphone apps, helping them stay on top of their care.
Integrated documentation for seamless care coordination
Integrated health documentation systems allow care teams to maintain a unified, up-to-date record of each patient’s medical history, treatments, and social determinants of health (SDOH). This centralization of data facilitates seamless communication between multidisciplinary teams, ensuring that all healthcare professionals involved in a patient’s care have access to the same information. The result is more coordinated care that minimizes errors and ensures that no aspect of the patient’s care is overlooked.
Patient portals
Patient portals give individuals access to their medical records, lab results, and appointment histories, allowing them to actively participate in their care. For instance, a patient with chronic kidney disease can monitor their test results and medication adherence, thus fostering a more engaged, informed relationship with their healthcare team. This transparency boosts patient confidence and supports better self-management.
Telehealth for expanded access
Telehealth technologies bridge geographical gaps by enabling remote consultations, reducing the need for in-person visits, and enhancing access to care for patients in underserved areas. It offers flexibility for patients who may face mobility challenges or time constraints, ensuring continuity of care. For providers, telehealth promotes timely follow-ups and proactive monitoring of patient health, resulting in quicker interventions and improved outcomes.
Secure messaging and communication
Secure messaging tools allow patients and providers to communicate in real-time, providing a direct channel for addressing patient concerns, clarifying treatment plans, and handling logistical issues. This continuous exchange of information helps keep patients informed and engaged in their care, reducing misunderstandings and improving adherence to treatment protocols.
Internet of things (IoT)
IoT allows real-time health data collection and monitoring through devices such as wearable fitness trackers or smart medical devices. These technologies provide healthcare providers with continuous updates on patients’ conditions, leading to timely interventions and improved outcomes. For example, wearable heart monitors can alert doctors if a patient’s heart rate spikes, enabling quicker responses to potential cardiac events.
How does blueBriX support Patient navigation?
When a patient calls up or is referred to a provider, the patient navigator is the first point of contact who takes care of the patient’s care journey. The patient navigator (also known as case manager, care coordinator, health navigator, patient advocate, healthcare guide, medical navigator, healthcare assistant, healthcare consultant, outreach coordinator, or promotor) initiates the care journey by taking the necessary information from the patient to understand his/her needs. The patient’s medical history, demographics, social determinants, current/previous medications, recent lab results, medication details and any other relevant information are fed into the system using various electronic or physical forms (as the case may be) that will help the navigator understand whom the patient should consult. blueBriX has a wonderful feature that lets the navigator compare the patient’s information in the existing database so that if it’s an existing patient, his/her records can be updated or else, a new patient record can be created.
The navigator can check insurance eligibility and upon validation, help the patient schedule an appointment with the right doctor (primary physician or specialist as the case may be). The navigator will then help the patient with necessary intake and consent forms required and also send timely appointment reminders or call up to confirm timely arrival for pre-appointment tests, if any. The navigator can also make logistics arrangements required for the patient using the provider network management modules. The navigator will be able to search for the nearest available transportation/shelter provider available in your ecosystem and make a booking as required.
Upon arrival, the patient’s vitals are fed into the integrated EHR, and pre-tests are automatically updated in the lab results. The navigator assists the patient to the waiting area and updates the check-in for the respective doctor or nursing department. The doctor will be able to access the patient’s health information from the system and feed in his/her diagnosis, e-prescription, further tests, referrals, and treatment plan. This information will be accessible by the navigator to book appointments as required and guide the patients to navigate their care journey without any hassles.
The call-center dashboard in blueBriX helps the patient navigator to manage an existing patient’s care coordination and secure communication in the most cost and time-effective manner. Depending upon the recommended treatment plan, the navigator can schedule appointments, referrals, community support, reminder notifications, personalized educational content, and follow-ups helping the patient get holistic care and better health outcomes at reduced cost. It’s a win-win for both patients and providers under value-based care models.
With automated scheduling, reminder notifications, referrals, lab and e-prescriptions, the patients will have less concerns about their care pathway. Regular follow-up will greatly reduce the chances of no-shows and missed medications. Their entire health record will be accessible in real-time, which helps the patients make informed decisions about their treatment options. With telehealth and video consultation options integrated into the EHR module, patients and navigators can easily contact each other from any part of the world, making care more accessible for the patients. The navigator can send personalized educational material for the patient based on their treatment plan and preferences to make their care journey more active, result-oriented and practical.
blueBriX’s remote patient monitoring and interoperability features make sure that the patient can connect their smart wearables and other smart medical devices which will keep their health information up to date. This avoids any possible human errors, and the provider will have real-time information about the patient’s health in case of any emergency. With real-time access to health information and predictive analytics the patient navigator and provider will have the advantage for preventive care and early intervention which further helps with cost-reduction and better health outcomes.
The navigators can customize workflows for single patients or cohorts using blueBriX’s highly customizable platform which comes with all international security stipulations and compliances. The navigation and treatment workflows can be defined in external systems as well and pushed to our integrated EHR using the APIs. blueBriX’s systems are crafted to work individually, as a customized suite with required features and as a supportive system with external digital health tools as well.
The future of patient navigation with blueBriX
The future of patient navigation lies in the seamless integration of advanced technology and personalized care, helping patients easily access and manage their healthcare journeys. Artificial intelligence (AI) and predictive analytics have the potential to provide more personalized, data-driven healthcare journeys. AI can help identify and engage patients in real time, ensuring that they receive timely interventions and streamlined care coordination across providers. This technology enhances decision-making by analyzing vast amounts of patient data, improving outcomes, and reducing healthcare costs. As patient navigation becomes more intelligent and efficient, patients will experience a more seamless and accessible healthcare experience.
Through an open, technology-agnostic platform, blueBriX enables value-based care organizations to provide real-time support, telehealth services, and interactive tools. These innovations reduce barriers to care, enhance patient engagement, and improve health outcomes by simplifying the complex navigation process, empowering patients to take an active role in their health management.