The healthcare landscape is quite complex, and providers face the daunting challenge of coordinating care across fragmented systems. Consider a patient with chronic heart disease who needs support from a primary care physician, a cardiologist, a nutritionist, and a mental health counselor. Often, these specialists operate within separate networks. The first hurdle for the primary care physician or specialists will be to have a reliable network of providers and other support groups who can fill the gaps and ensure the best care delivery and patient outcomes. Then comes well-coordinated communication and cohesive treatment plans that can drive positive health outcomes.
For instance, if one or some of the patients need to consult cardiologist, and if the primary physician does not have a good one in his/her network, the patient is likely to switch to a more equipped provider. Further, if the cardiologist prescribes a new medication but fails to relay this information to the primary care physician, the patient may encounter dangerous drug interactions or receive conflicting advice about their diet and lifestyle changes. This scenario underscores the pressing need for integrated provider networks that facilitate seamless collaboration and real-time information sharing.
By establishing a provider network that fosters collaboration and real-time data sharing, healthcare professionals can break down these walls and ensure seamless, coordinated care that enhances the patient’s overall experience. A well-integrated provider network acts as a bridge, connecting different specialists and enabling them to work together, ensuring the patient receives holistic and timely care.
Healthcare isn’t a series of isolated transactions; it’s a symphony of care, where every note matters. As Steve Jobs once said, “Great things in business are never done by one person. They’re done by a team of people.” In a world where collaboration is the key to success, the question is: why are we still building walls when we should be building bridges?
With blueBriX’s Provider Network Management (PNM) solutions, we’re not just connecting people; we’re transforming how care is delivered, moving from disjointed silos to a harmonious, integrated effort.
The problem of siloed systems
Siloed systems in healthcare refer to isolated and disconnected processes where data and information are trapped within individual departments or systems. This fragmentation means different healthcare providers (doctors, hospitals, specialists) often operate independently without shared access to crucial patient information. These silos result in a lack of coordination, inefficiencies, and hindered communication across the care continuum.
What if a patient is discharged from a hospital without their primary care provider being informed? Without crucial updates about post-hospitalization care, the patient may not receive necessary follow-up treatments, which could lead to complications, readmissions, or worse outcomes. Medication errors or duplicated tests can arise from the lack of a shared health record.
Outdated health systems, such as paper-based records or incompatible electronic health record (EHR) systems, act as barriers or “walls” to effective collaboration. These systems often lack interoperability, preventing seamless information exchange between different healthcare settings. This lack of connectivity increases errors, reduces efficiency, and ultimately compromises patient care.
How provider networks improve care
Provider networks are organized groups of healthcare providers, such as hospitals, doctors, and specialists, who are contracted to offer medical services to individuals under specific insurance plans or healthcare systems. They facilitate data sharing and smoother transitions across care settings, ensuring that patients receive the right care at the right time without unnecessary delays or repeated tests.
By bridging the gap between isolated providers and enabling shared access to patient data, Provider Network Management fosters a coordinated care ecosystem. Through integrated technology, Provider Network Management removes these barriers, ensuring healthcare teams can communicate effectively, collaborate on care plans, and improve outcomes. Essentially, it creates a pathway to overcome these silos, promoting connected care and reducing the risks posed by fragmented systems
What is provider network management (PNM)?
Provider Network Management not only helps healthcare organizations manage their network of providers efficiently, but it also enables the creation of a “single source of truth” (SSOT). This concept is essential in value-based care, where accurate, consistent, and up-to-date data is crucial for making informed decisions that impact patient outcomes, cost efficiency, and overall network performance. By establishing a SSOT, Provider Network Management ensures that all stakeholders—whether providers, payors, or patients—are working from the same set of reliable data. This helps avoid duplication of services, reduces errors, and improves the coordination of care across the healthcare continuum, ultimately leading to better patient outcomes and enhanced operational efficiency in a value-based care environment. Before we explore this further, let’s quickly understand the 3 components:
- Provider: Refers to the doctors, hospitals, clinics, or specialists who deliver healthcare services. These providers are part of an insurer’s or health plan’s network, meaning they have agreed to provide services under the terms of that plan.
- Network: This is the group of healthcare providers that have been contracted to deliver services to the health plan’s members. A well-organized network ensures that patients have access to a wide range of medical services while controlling costs for both the patients and insurers.
- Management: Involves overseeing the entire network to ensure efficiency, compliance, and quality care. This includes tasks like credentialing providers, negotiating contracts, ensuring data integrity, and monitoring performance. It also ensures that providers meet regulatory standards and that patient care is streamlined.
Let’s come back to the core question, what is Provider Network Management?
Provider Network Management is the process of organizing, maintaining, and overseeing a network of healthcare providers to ensure they deliver high-quality, cost-effective, and compliant care. It includes recruiting, contracting, credentialing, and monitoring providers to meet healthcare standards and regulatory requirements.
Provider Network Management is crucial for health plans (payors) as it supports the relationship between healthcare providers and insurance companies, ensuring coordinated care, efficient patient data management, and streamlined services. It aims to enhance provider relations, streamline credentialing processes, and improve patient outcomes by creating an integrated network of services.
Key functions of provider network management
- Provider onboarding: Streamlines the process of enrolling providers into a healthcare network to ensure timely access to care.
- Credentialing: Verifies and manages provider qualifications, reducing the administrative burden for healthcare providers.
- Data management: Consolidates essential provider data, such as credentials, contracts, and care plans, ensuring accuracy and efficiency.
- Automation: Provider Network Management streamlines repetitive tasks such as credentialing, contract approvals, and provider data updates.
- Workflow management: Effective workflow management helps in tracking progress at each stage, from initial provider applications to contract renewals, ensuring that nothing is overlooked, and timelines are maintained.
- Relationship management: Relationship management focuses on maintaining strong, collaborative ties between payors and healthcare providers.
- Contracting: Efficient contract management ensures compliance with legal and regulatory requirements, helps manage reimbursement rates, and supports transparency in provider relationships.
- Compliance and quality assurance: Ensures that providers adhere to regulatory standards and maintain high-quality care throughout their tenure.
- Lifecycle tracking: Monitors the entire provider lifecycle to maintain network quality and track performance
- Visibility and accuracy: Enhances access to accurate provider information for members.
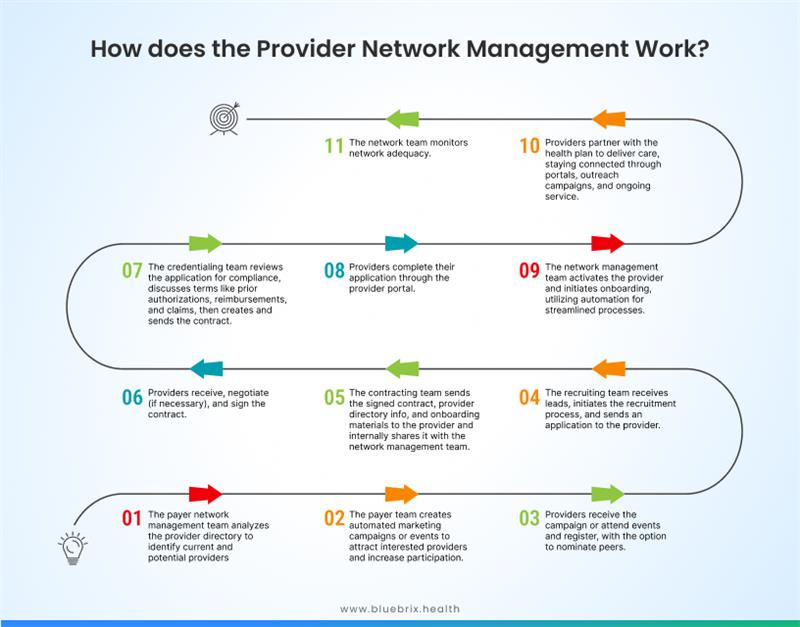
How does the provider network management work?
Here’s a step-by-step breakdown of how Provider Network Management works:
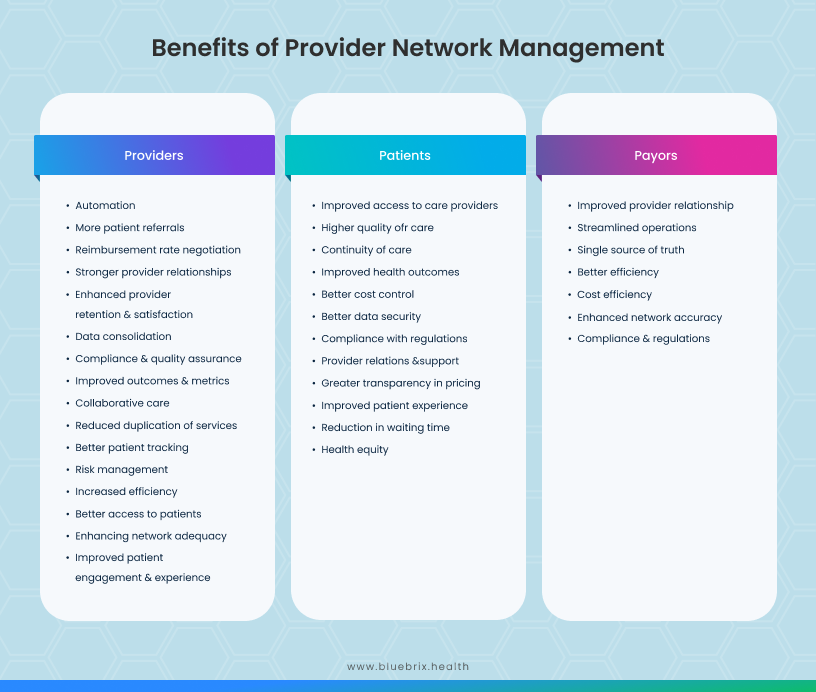
Benefits of provider network management
Provider Network Management enables providers with seamless data sharing, ensuring coordinated care, and reducing care fragmentation. It also automates administrative tasks like credentialing and contract management, allowing providers to focus on patient care, improving operational efficiency, and boosting outcomes.
Challenges in provider network management
Provider Network Management plays a crucial role in ensuring the seamless integration of healthcare providers to deliver coordinated care. However, managing these networks comes with a variety of challenges that can hinder efficiency and effectiveness. These challenges stem from the complexities of credentialing, data management, and maintaining seamless communication across a diverse network of providers. Understanding these obstacles is vital for addressing gaps and optimizing network performance.
- Credentialing delays: Slow credentialing processes create bottlenecks in on-boarding new providers, leading to inefficiencies, increased administrative overloads, and frustrations among healthcare teams.
- Data integration: Ensuring that all provider and patient data are seamlessly integrated across platforms is difficult, often leading to fragmented information.
- Network performance: Managing and optimizing network performance is an ongoing issue for providers, with poor performance impacting provider collaboration and patient care.
- Compliance and security: Meeting regulatory compliance standards and ensuring data security in a healthcare network environment presents significant challenges.
- Provider dissatisfaction: Many providers express dissatisfaction with network management, particularly around communication and support services.
Pillars of the provider network management bridge
Despite the above challenges, Provider Network Management can succeed by focusing on key pillars that ensure efficiency, scalability, and provider engagement. They typically include:
- Network development & optimization: Identifying, recruiting, and contracting sufficient providers in a geographic area to meet patient needs. An effective strategy is using data analytics to map out areas of patient demand and provider availability. This will help the providers streamline care coordination. Ongoing analysis to improve network efficiency, ensuring patient needs are met without excessive resource use. For instance, using predictive analytics to identify gaps in care access thereby enabling providers to cut re-admission costs.
- Credentialing: Ensuring providers meet compliance standards. Automating credentialing processes can reduce delays and errors, allowing for faster on-boarding.
- Referral management: Streamlining the process of directing patients to appropriate specialists or services within or outside the network. It improves continuity of care by ensuring that referrals are tracked, managed, and optimized based on patient needs and provider availability. By automating referral processes and providing insights through dashboards, referral management systems enhance the accuracy and efficiency of care pathways, supporting timely and effective patient transitions.
- Contract management: Helps providers in negotiating and maintaining provider contracts. A best practice is using software to track contract terms and renewals to avoid lags in network performance.
- Care coordination: Integrates patient care activities across multiple providers, helping to align treatment goals and reduce gaps in patient care. Effective care coordination tools enable providers to share information seamlessly and manage patient interactions, resulting in cohesive, patient-centered care. This pillar fosters collaboration among healthcare professionals, supports multidisciplinary workflows, and improves patient outcomes by ensuring that care is organized, communicated, and aligned across all stakeholders within the provider network.
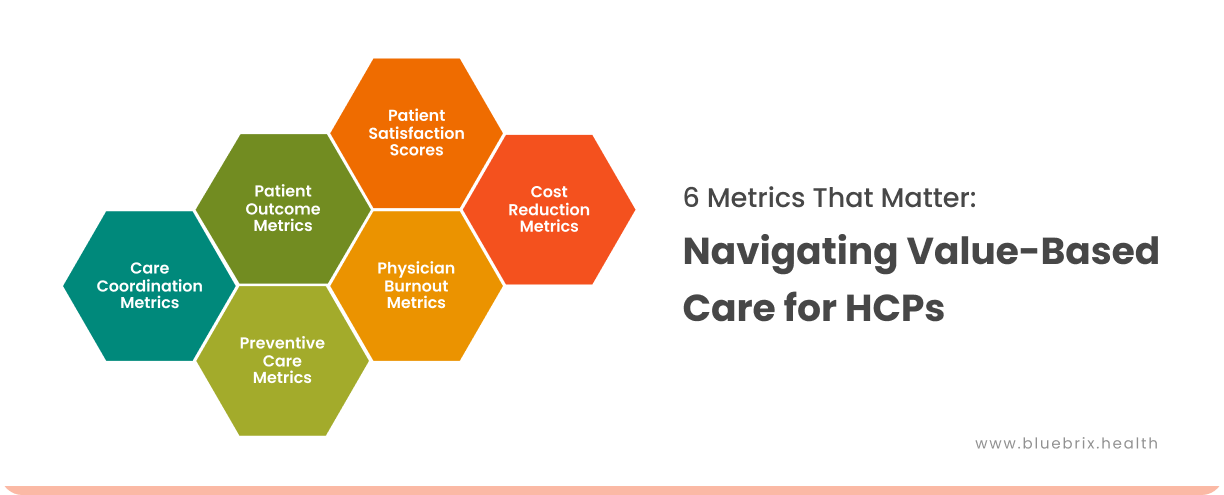
- Performance management: Regularly assessing provider performance using data-driven insights to optimize care quality and efficiency. For example, setting benchmarks for patient satisfaction and tracking them via analytics.
Strategies for efficient provider network management
Building a strong Provider Network Management system requires a mix of technology, strategic planning, and data utilization. Here are some key strategies:
- Use real-time data to assess network performance, optimize provider contracts, and identify gaps in care. This ensures a high-performance network that meets patient needs efficiently.
- Automate provider enrollment and credentialing processes to reduce administrative burdens and accelerate the time it takes for providers to join the network.
- Establish compliance protocols that continuously monitor provider performance and adherence to regulatory standards, ensuring high-quality care throughout the network.
- Implement advanced technology to integrate care plans, medical records, and communication tools across the network, enhancing collaboration and efficiency.
- Continuously assess and optimize the geographic spread and specialties within the network to ensure patient access to essential care services.
Provider network management with blueBriX
blueBriX addresses the challenges of provider network management with a comprehensive suite of solutions that can be tailored to your unique requirements. The blueBriX platform provides a wide array of highly adaptable and scalable tools such as Electronic Health Records, Patient Portal, blueIntelligence, and a host of microservices, all designed to enhance operational efficiency, foster better communication, and ensure the delivery of coordinated care across networks.
Network development & optimization
With advanced interoperability and seamless integration features, blueBriX has become a powerful asset for provider network management. Equipped with tools for clinical workflow management, telemedicine, medical device integration, and adherence monitoring, blueBriX facilitates cohesive care coordination across internal and external systems. Leveraging its low-code/no-code app builder, blueBriX makes sure that tailored solutions can be rapidly created to address the evolving network needs. blueBriX tools support optimized provider interactions and efficient patient care delivery.
Provider credentialing
Provider credentialing is a core feature in blueBriX’s Revenue Cycle Management (RCM) suite. The credentialing process ensures healthcare providers meet the stringent qualifications set by insurance companies and healthcare networks, allowing them to deliver reimbursable services while maintaining compliance. This verification not only upholds the quality of care but also streamlines claims processing and provider-payer relationships.
The Prior Authorization feature in our EHR module expedites service approvals, ensuring timely care and reducing claim denials. Eligibility Verification confirms the provider and patient coverage details upfront, enhancing billing accuracy, while Eligibility Reports provide comprehensive insights into provider/patient eligibility, helping providers make informed decisions and minimize claim errors. Together, these features promote compliance, improve financial stability, and optimize care delivery.
Referral management
blueBriX comes with a comprehensive suite of tools to support referral management that are critical for provider network management. The New Referrals feature works with both internal and external providers, while Search and Filter tools enable quick access to specific referrals based on patient, type, date, and status. Users can view All Referrals in a consolidated list, with separate sections for Internal and External Referrals, ensuring clear visibility of referral pathways within or outside the organization. The Detailed View presents referral specifics, including patient and referral coordinator details, with Date and Program Information showing when and from which program referrals were initiated. The Referred By/To feature identifies users involved in the referral process, and referrals can be prioritized and categorized as incoming or outgoing. With Actions for sending, removing, and editing referrals, along with access to status logs, blueBriX ensures a streamlined and effective referral management process across provider networks. Referral Reports provide detailed insights based on criteria such as referral type, patient, status, priority, and ICD10 codes.
Contract management
blueBriX’s Contract Management capabilities include secured document management and messaging functionalities that streamline the handling of contracts and communication. With these tools, providers can securely store, share, and collaborate on contract documents, ensuring compliance and safeguarding sensitive information. For additional custom functionalities, blueBriX can quickly build specialized features using its no-code and low-code app builder. This flexibility allows providers to ensure compliant and secure applications that enhance their network management capabilities, driving operational efficiency and fostering stronger partnerships within their network.
Care coordination
blueBriX enhances care coordination within provider networks through a range of interconnected tools. Clinical Messaging allows healthcare providers to exchange patient information, treatment plans, and referrals in real time, ensuring all parties remain informed and aligned. The Scheduling Dashboard further supports care coordination by organizing pre-appointment processes such as intake forms, insurance verification, and payment agreements, while its customizable tracking capabilities streamline departmental communication and workflow. Calendar integration enables effective scheduling and resource management, reducing conflicts through Outlook, syncing reminders, and waiting list features, which improve patient management.
In addition, various Program Managements streamline program-specific tasks such as performance monitoring, compliance, eligibility requirements, and billing, creating a unified and coordinated care experience across multiple programs. APIs play a crucial role in enabling seamless data exchange between systems, ensuring all providers have access to real-time, comprehensive patient information for personalized treatment plans. Together, these features enhance the efficiency, communication, and organization required for effective, coordinated patient care across the provider network.
Performance management
blueBriX offers robust performance management tools for provider network management, designed to ensure quality, compliance, and optimized resource use. The Encounter Review Process supports multi-level supervisor roles, enabling supervisors to assess provider performance at different levels for quality assurance. Capacity Planning Management provides tools for generating reports like Booked vs. Actual, which analyze provider schedules, facilitating better resource allocation.
Additionally, blueBriX’s Reporting Tools enable detailed performance reviews by creating reports that compare planned activities with actual outcomes, giving a clear picture of provider performance. The Diagnosis Classification feature further supports performance management by organizing diagnostic data into primary, secondary, and tertiary classifications with CRUD capabilities, ensuring information is efficiently structured for assessment. Together, these features create a comprehensive system for managing and evaluating both internal and external provider networks.
With blueBriX as the technology backbone, healthcare organizations can effectively manage their provider networks, directories, appointments, and referrals. Providers within the network benefit from real-time access to patient data, virtual consultations, and powerful analytics, all of which contribute to improving network performance and optimizing patient outcomes.
Through its scalable and adaptive solutions, blueBriX supports diverse healthcare systems, connecting various providers into a cohesive network. This ensures that both patients and providers experience streamlined care, benefiting from a system that prioritizes collaboration, efficiency, and quality improvement.
blueBriX is designed with robust compliance and data security measures, ensuring that healthcare provider networks meet stringent regulatory requirements, such as HIPAA and GDPR. With built-in encryption, secure access controls, and customizable security analytics, blueBriX safeguards sensitive patient and provider information. These features make blueBriX the perfect solution for managing provider networks with confidence and precision.
The Future of healthcare collaboration
As healthcare continues to evolve, provider networks are moving beyond isolated, siloed systems and transforming into highly integrated ecosystems where collaboration is key. The future of healthcare is defined by connectivity—a seamless interaction between human expertise and cutting-edge technology. This collaboration is central to overcoming inefficiencies, improving patient outcomes, and providing holistic, coordinated care across networks.
The rise of artificial intelligence (AI), telemedicine, and predictive analytics is empowering healthcare providers to work together more effectively, breaking down traditional barriers that once hindered communication and collaboration. As these technologies mature, they are enabling healthcare providers to share real-time data, monitor patient progress remotely, and offer personalized treatment plans across vast networks of care. This evolution allows healthcare providers to focus on what matters most—delivering high-quality, value-based care to their patients.
Scalable platforms like blueBriX are leading this charge. blueBriX offers adaptable solutions that streamline provider network management by ensuring interoperability, enabling real-time data exchange, and fostering collaborative care workflows across various providers. Its suite of tools—ranging from electronic health records to predictive analytics in blue Intelligence—supports decision-making and enhances care coordination across multiple specialties. These innovations not only reduce administrative burden but also help providers anticipate patient needs, optimize resources, and respond faster to emerging health trends.
In a future driven by technology-human collaboration, solutions like blueBriX will continue to break down the walls of inefficiency, making healthcare a fully interconnected, patient-centered system where collaboration is easy, scalable, and impactful.