Why are coalitions critical in value-based care?
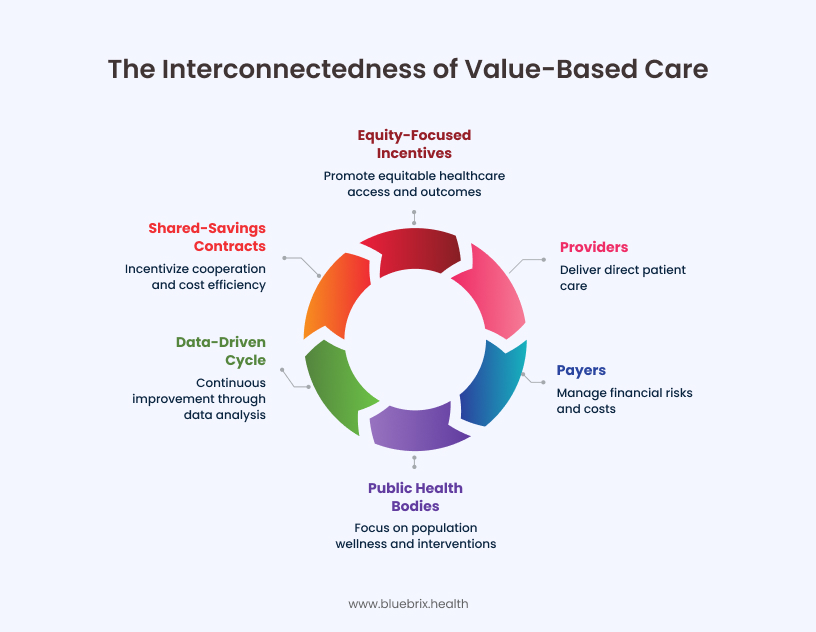
Coalitions connect every piece of the system; providers who deliver care, payers who manage financial risk, and public health bodies that focus on population wellness. When these groups share a common purpose, care coordination becomes a continuous, data-driven cycle rather than a series of handoffs. A primary care physician can see which of their patients are flagged for rising risk, a payer can anticipate cost spikes, and a public health agency can deploy targeted interventions. In 2025, CMS and major payer groups are reinforcing this approach through shared-savings contracts and equity-focused incentives that reward cooperation rather than competition.
The challenge in value-based care coalitions
Building these coalitions is not easy. Incentives differ, data lives in silos, and technology adoption is uneven. A provider’s EHR may not talk to a payer’s claims platform, and public health databases often lack patient-level visibility. Even when everyone agrees on the desired outcome, the absence of shared infrastructure creates operational blind spots. These disconnects make it difficult to measure success, allocate savings fairly, or respond quickly to changing patient needs. The result is frustration and fatigue in a system that depends on coordination to thrive.
The opportunity with technology
This is where technology becomes the difference-maker. Modern interoperability frameworks such as FHIR, TEFCA, and API-based data exchange now allow coalitions to share information securely and in near real time. Predictive analytics highlight at-risk populations before crises occur, while dashboards turn data into shared accountability. Technology does not replace relationships, it strengthens them. It gives every stakeholder the same version of the truth and the ability to act on it. For value-based care, this is how coordination scales beyond pilot projects into sustainable transformation.
To turn collaboration from concept into practice, coalitions need a clear roadmap—one that aligns goals, standardizes data sharing, and defines measurable impact. The following steps outline how technology can operationalize this alignment, transforming coalitions from loosely connected partners into high-performing ecosystems of care.
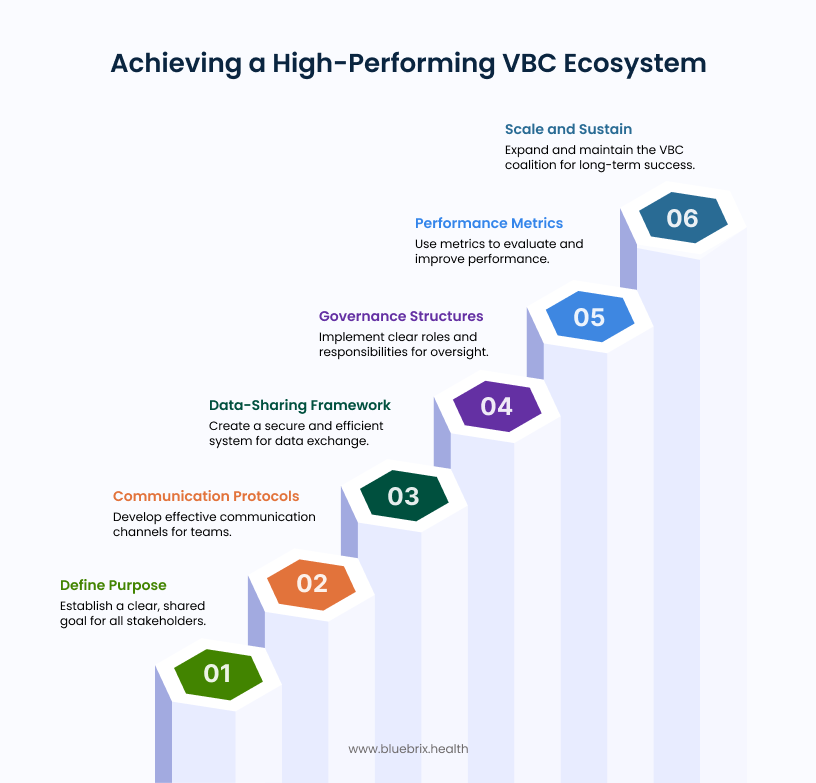
Step 1: Define a common purpose in the value-based care context
Coalitions succeed when all parties agree on what “value” means and how it will be measured. Providers usually care most about quality, safety, and patient satisfaction. Payers prioritize reduced total cost of care and minimized financial risk. Public health agencies focus on equity and measurable improvement at the population level. The coalition’s first task is to merge these perspectives into a single statement of purpose.
That purpose must then translate into measurable goals. A coalition might commit to reducing emergency department visits for chronic-disease patients by twenty percent within eighteen months. Technology converts these goals into tangible progress through shared dashboards and digital scorecards that display key performance indicators for everyone involved. When all partners see the same data, alignment becomes more than an aspiration, it becomes routine.

Step 2: Establish communication protocols for multi-stakeholder teams
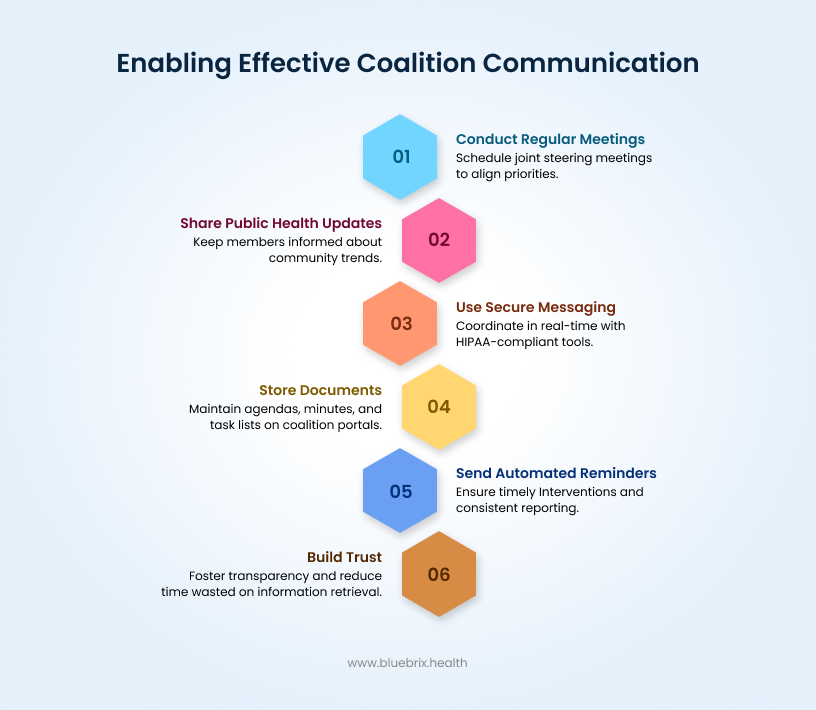
Even the best data-sharing plan fails without clear communication. Coalitions need structured, predictable dialogue between providers, payers, and community organizations. Regular joint steering meetings ensure that clinical and financial priorities stay synchronized. Public health updates keep all members aware of community-level trends that may affect outcomes.
Technology supports this rhythm. Secure, HIPAA-compliant messaging allows care teams to coordinate in real time without resorting to unsecured channels. Coalition portals store agendas, minutes, and task lists so decisions do not get lost between meetings. Automated reminders and workflow alerts keep interventions on schedule and reporting consistent. When communication is transparent and recorded, coalitions build trust faster and waste less time chasing information.
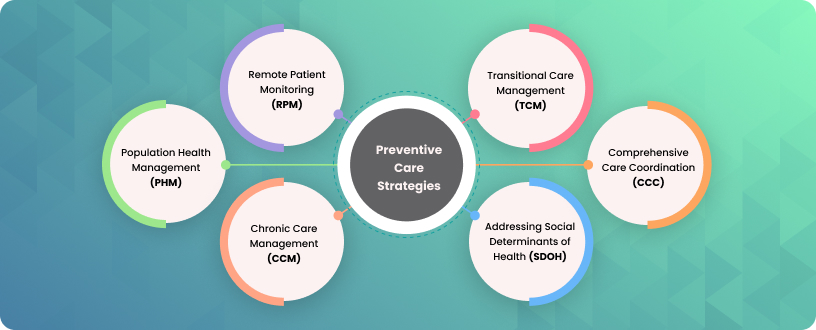
Step 3: Build a data-sharing framework across healthcare entities
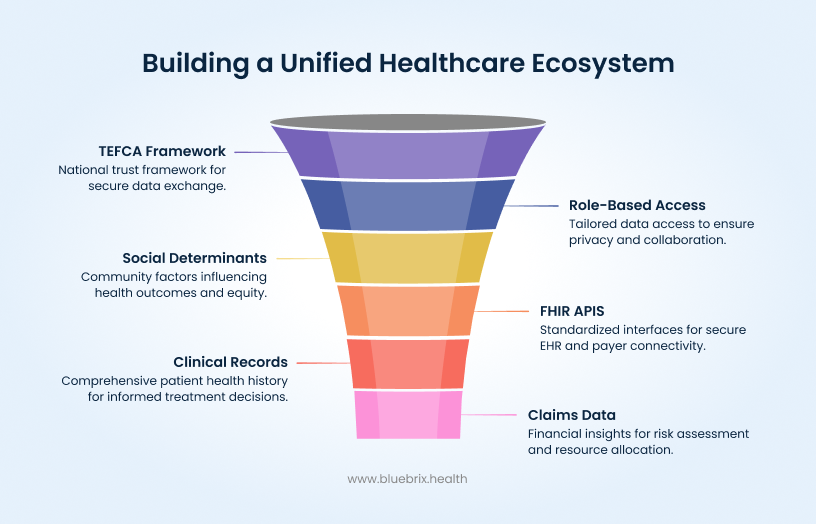
Data is the backbone of care coordination. A complete picture of patient health requires blending clinical records, claims, and social determinants data. Modern standards make this achievable. FHIR-based APIs connect EHRs and payer systems, while TEFCA participation provides a trusted national framework for secure exchange.
A well-structured framework defines what each stakeholder can see and use. Providers need patient-level details to inform treatment. Payers require aggregate views to evaluate risk pools. Public health teams depend on de-identified, community-level data to measure equity. Role-based access controls, single sign-on, and automated consent workflows maintain privacy while enabling collaboration. Instead of fighting over data ownership, coalition members can focus on shared insight and faster action.
Step 4: Create governance and accountability structures
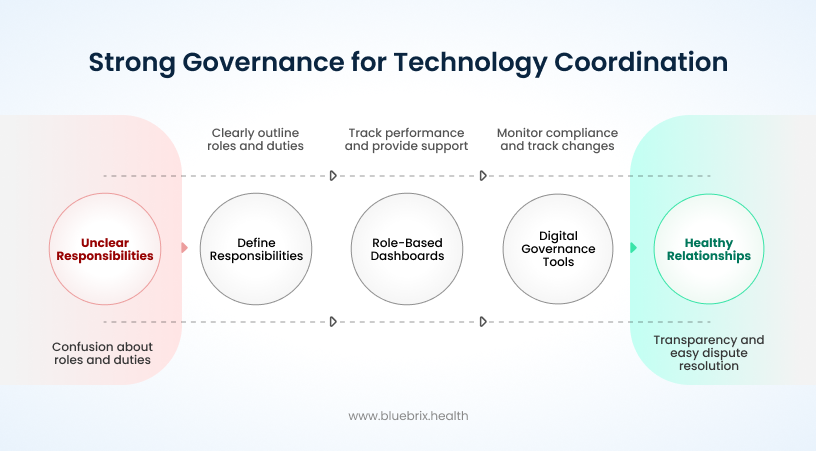
Technology enables coordination, but governance sustains it. Clear structures ensure that everyone knows their responsibilities, rights, and reporting obligations. Providers lead on care delivery and documentation. Payers manage analytics, reimbursement, and performance modeling. Public health agencies safeguard equity and community outcomes.
Transparency keeps these relationships healthy. Role-based dashboards show who is meeting goals and who needs support. Digital governance tools track approvals, monitor compliance, and log changes to contracts or workflows. When accountability is visible, disputes are easier to resolve and shared savings easier to allocate. Strong governance turns coalition meetings from negotiation tables into strategy sessions focused on patient outcomes.
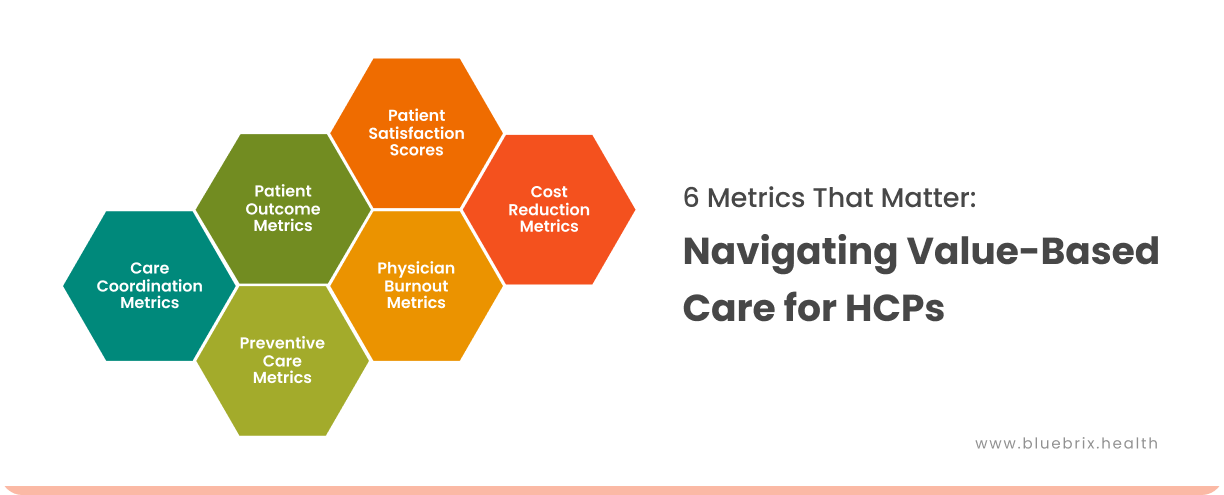
Step 5: Implement performance metrics and continuous evaluation
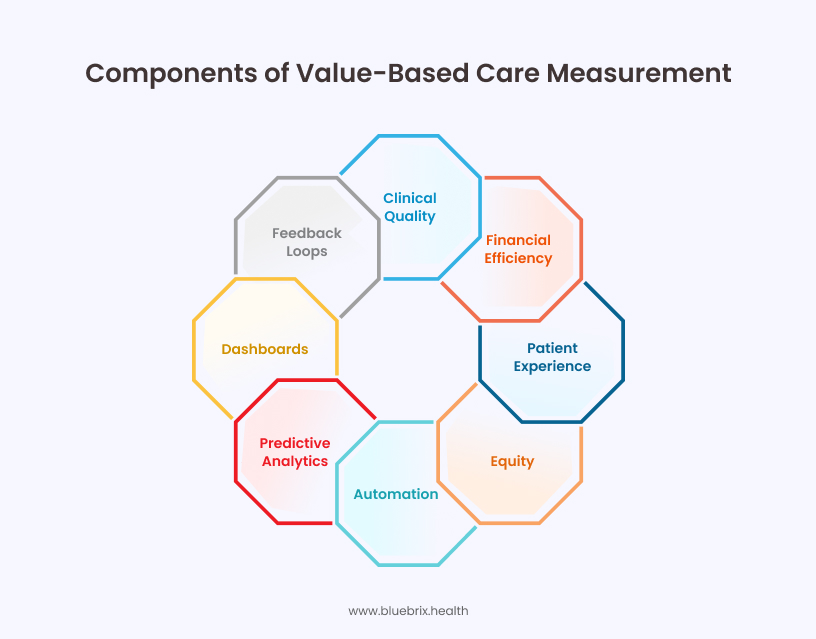
Value-based care lives and dies by measurement. Coalitions must track a balanced set of metrics that capture clinical quality, financial efficiency, patient experience, and equity. Clinical measures might include readmission rates or preventive-screening compliance. Financial metrics such as shared savings and medical loss ratios show whether coordination is paying off. Patient surveys and engagement rates provide a human check on whether improvements are felt at the bedside.
Automation keeps these metrics current. Predictive analytics identify early-warning signs when performance starts to slip. Dashboards consolidate results for coalition-wide visibility. Regular feedback loops (monthly for operations, quarterly for strategy) turn measurement into learning. Instead of reacting to year-end surprises, coalitions adjust course in real time.
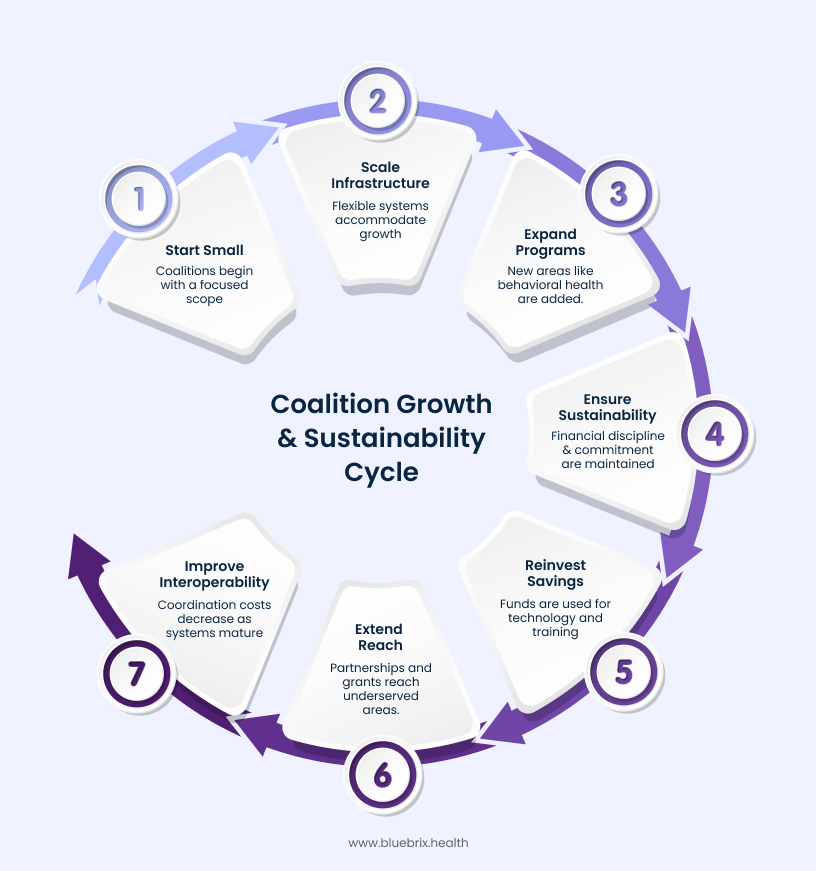
Step 6: Scale and sustain the VBC coalition
Most coalitions start small, focusing on one disease group or geography. Scaling requires flexible infrastructure that can accommodate new partners and broader goals without losing control. Configurable workflows and modular integration make it easier to expand programs from diabetes or heart failure to behavioral health, maternal care, and multi-condition populations.
Sustainability comes from financial discipline and shared commitment. Successful coalitions reinvest savings into technology upgrades and workforce training. Public-private partnerships and grants extend reach into underserved areas. As interoperability matures nationwide, the cost of scaling coordination falls. The result is a coalition that grows stronger, not heavier, as it expands.
The technology advantage: How blueBriX orchestrates VBC coalitions
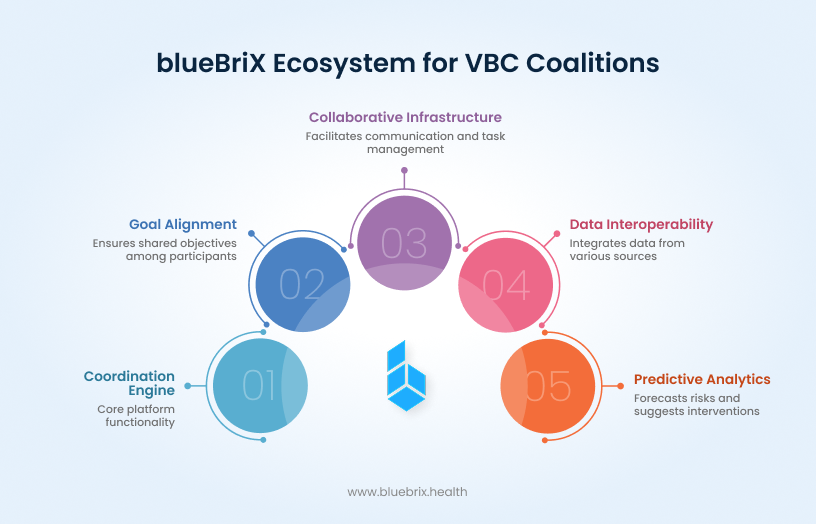
blueBriX is more than a platform; it’s the coordination engine that transforms disparate value-based care (VBC) participants—payers, providers, and public health agencies—into a single, high-performing coalition. Its core strength lies in its ability to enforce goal alignment and turn complex VBC models into transparent, measurable operations.
The key mechanism for this alignment is automated goal-mapping. blueBriX doesn’t just display goals; it actively links granular care pathways and clinical activities directly to high-level value-based metrics (e.g., reductions in readmission rates, improvements in HEDIS scores, or total cost-of-care containment). This top-down, bottom-up linking ensures every participant, from the frontline nurse to the system administrator, can see the direct causal relationship between their daily work and the collective financial and clinical outcomes. This eliminates the “black box” of VBC reporting, fostering a culture of shared accountability.
This operational clarity is backed by a robust collaborative infrastructure. The built-in communication tools offer more than secure messaging; they integrate notifications and task management directly into the care workflow. This seamless tie-in of payer, provider, and public health efforts is what turns communication into actionable coordination.
Data interoperability and actionable intelligence
On the data side, blueBriX is engineered for true interoperability, moving beyond simple data aggregation to contextual data sharing. It integrates bi-directionally with EHRs, payer claims systems, and public health registries through modern, standardized APIs that handle varied data structures and semantic differences. This capability ensures that the coalition is always operating on the most current and comprehensive view of the patient population, unifying clinical records with financial encounters.
blueBriX platform’s reporting modules are precision-aligned with industry standards, particularly CMS metrics and other core VBC reporting requirements, reducing administrative overhead. This unified data foundation is what fuels the platform’s advanced analytical capabilities, allowing the coalition to operate not just efficiently, but predictively.
Predictive analytics: Targeting interventions before costs rise
If data integration provides the materials, predictive analytics within blueBriX serves as the coalition’s early warning radar, fundamentally altering the cost curve of population health management.
Traditional VBC reporting relies on lagging indicators (knowing the cost after a high-cost event). blueBriX generates leading indicators of risk through sophisticated machine learning models that continuously score every patient in the covered population. This goes beyond simple comorbidity indices to incorporate behavioral and social factors integrated via standardized registries.
When a patient crosses a predefined risk threshold, blueBriX doesn’t just send an alert; it automatically generates a targeted intervention plan specific to the coalition’s current objectives. Crucially, the system models the potential financial impact of the intervention—quantifying the cost avoidance potential tied to specific actions, shifting the focus from reactive treatment to proactive, personalized prevention.
Governance and accountability: Enforcing the coalition contract
In a VBC coalition, the technology must act as an impartial arbiter and an accountability enforcer. blueBriX’s governance features establish a verifiable chain of trust and responsibility:
- Granular role mapping: The platform maps specific permissions and responsibilities to defined coalition roles, ensuring that when a goal is missed, the system can precisely trace which role owned the necessary preceding action.
- Real-time audit trails: Every interaction, from a data upload to a task completion, is timestamped and logged, creating an immutable, real-time audit trail. This is crucial for resolving disputes over performance attribution and regulatory compliance.
- Standardized data definitions: The system forces the adoption of common data dictionaries for VBC metrics, ensuring that all partners are measuring against the same standard, which is foundational to coalition trust.
Payer-provider alignment: De-risking the shared contract
The pivot to VBC hinges on shared financial risk. blueBriX transforms this relationship into a transparent, mathematically verifiable partnership:
- Unified attribution and benchmarking: The platform establishes a single, agreed-upon definition of the patient population and the cost baseline, eliminating initial contractual friction points.
- Real-time performance tracking against risk pools: blueBriX automatically manages complex risk-adjustment models, calculating Per Member Per Month (PMPM) costs and quality metrics as they accrue. This shared, objective dashboard allows both parties to see potential savings or losses in-year, enabling proactive course correction and eliminating surprises.
- Contract scenario modeling: To facilitate trust before the contract is finalized, the platform allows partners to run “what-if” scenarios based on their own aggregated data, using data-driven negotiation to effectively de-risk the contracting process.
The human element: Empowering clinicians
The platform is designed to serve one core purpose: to reallocate the clinician’s time from administration to care delivery.
- Point-of-care relevance: Predictive insights are pushed directly into the provider’s workflow at the moment of patient interaction. The physician immediately sees the patient’s risk score and the top three recommended interventions, transforming data from a retrospective chore into a prospective clinical tool.
- Automated documentation and follow-up: blueBriX’s automation handles routine reporting and follow-up status updates. This frees clinicians to focus on the ‘why’—the crucial elements of empathetic, personalized care, shared decision-making, and addressing social determinants of health that drive long-term value.
The coalition mandate: Technology as the catalyst for VBC success
The journey to VBC mastery is defined by the ability to scale these coordinated efforts. blueBriX moves coalitions beyond demonstrating value in a pilot to delivering measurable, repeatable, and financially sustainable impact across entire populations.
By embedding interoperability, automation, transparency, and predictive intelligence into its core functionality, blueBriX automates the process overhead of VBC. This technological shift is what allows high-performing coalitions to not only succeed in their current contracts but to rapidly expand their VBC footprint with predictable, lower-risk overhead. The right platform is the catalyst for coalition success.