The evolution of healthcare can be looked at as a full-scale migration, rather than a slow trend. The Value-Based Care (VBC) model has fundamentally redefined success, shifting the reward structure from the volume of services rendered (Fee-for-Service) to the measurable quality of patient outcomes and cost-efficiency. This seismic change demands that healthcare leaders focus on improving health outcomes, enhancing the patient experience, and delivering services at a reasonable cost.
But VBC success is not an aspiration; it is an operational mandate built on execution. The primary adversary in this transition? Fragmentation.
The current system is riddled with disjointed handoffs: patients are unclear on referrals, specialists lack crucial information and updates, and follow-up data often gets lost. This inefficiency is fiscally destructive. Studies confirm that proactive, coordinated efforts have the potential to decrease patient costs by nearly 50% compared to fragmented care.
For any organization taking on risk, the transition to Value Based Care is a test of integrated operations. If the care delivery model is fragmented, the resulting inefficiencies immediately strain the bottom line. This is why VBC success focuses on mastering a foundational triad, three interdependent Key Performance Indicators (KPIs), that, when aligned by sophisticated care coordination, transforms risk into reward.
The foundational KPIs of value based care
In a risk-bearing model, you must simultaneously manage financial accountability, patient complexity, and clinical outcomes. Relying on a single metric is like trying to build a house on a single support beam.
The success mantra is to balance the three core VBC KPIs:
- Hierarchical condition categories (HCC): The engine of risk and revenue integrity.
- Healthcare effectiveness data and information set (HEDIS): The standardized scorecard for clinical quality and outcomes.
- Medical loss ratio (MLR): The mandate for financial efficiency and regulatory compliance.
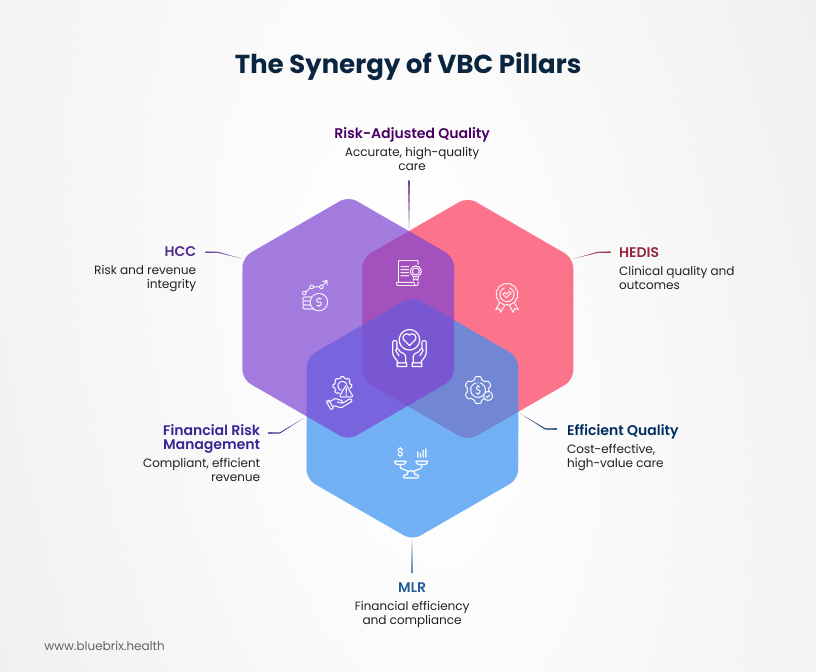
Care coordination is the unified operating system that optimizes all three of these pillars. Here is how that triad works in practice.
PILLAR 1: HCC and revenue integrity
If you don’t accurately know how sick your patients are, you will lose money. It is that simple.
The HCC model, particularly within Medicare Advantage (MA), is the mechanism CMS uses to quantify a patient’s burden of illness. By coding chronic diagnoses (using ICD-10 codes), the system calculates a Risk Adjustment Factor (RAF) score for each patient. This RAF score is a prospective measure, predicting the healthcare costs for that individual in the coming year.
The financial implication is immense: The capitated payment your organization receives from CMS is directly adjusted by your population’s RAF scores.
How is HCC connected to care coordination?
Failure to accurately “know how sick your patients are” (i.e., failure to capture complexity via HCC coding) results in a massive gap between the revenue received and the actual cost of providing care, directly leading to financial loss, regardless of how efficient the clinical team is.
- The Under-Coding Crisis: Unlike Fee-for-Service, which focuses on the presenting problem, VBC demands comprehensive, whole-person documentation. If patient complexity is under-coded, the resulting RAF score will be artificially low, leading to insufficient Per Member Per Month (PMPM) payments to cover the actual cost of care. Failure to capture complexity can cost millions annually.
- Annual Recapture: Every chronic medical problem must be coded and documented annually to be factored into the risk score.
Imagine a Value-Based Care organization operating a Medicare Advantage contract, where payment is fixed based on the predicted health status of its enrolled population. This prediction is made using the patient’s Risk Adjustment Factor (RAF) score, which is calculated from the chronic conditions documented annually through HCC coding.
The average, healthy Medicare beneficiary has an RAF score of 1.000, which translates to a specific base payment (Per Member Per Month, or PMPM) from the payer. Patients who are sicker receive an RAF score above 1.000, triggering a higher PMPM payment.
Consider two patients in your network, both of whom have severe, poorly controlled Type 2 Diabetes, complicated by chronic kidney disease and peripheral neuropathy. They are clinically complex and require specialized care, multiple medications, and frequent follow-ups. The actual cost of care for each patient is projected to be $1,500 PMPM.
Patient A had a comprehensive annual visit where the physician meticulously documented all of their chronic conditions, including the complications, meeting the strict HCC documentation guidelines. Result: The system accurately calculates an RAF score of 1.50. The VBC organization receives a PMPM payment of $1,500. (Breakeven)
Patient B had a quick visit where the physician only documented “Type 2 Diabetes” and missed the required annual documentation (recapture) of the chronic kidney disease. Result: The system calculates an artificially low RAF score, say 1.00. The VBC organization receives a PMPM payment of $1,000. (Underpaid)
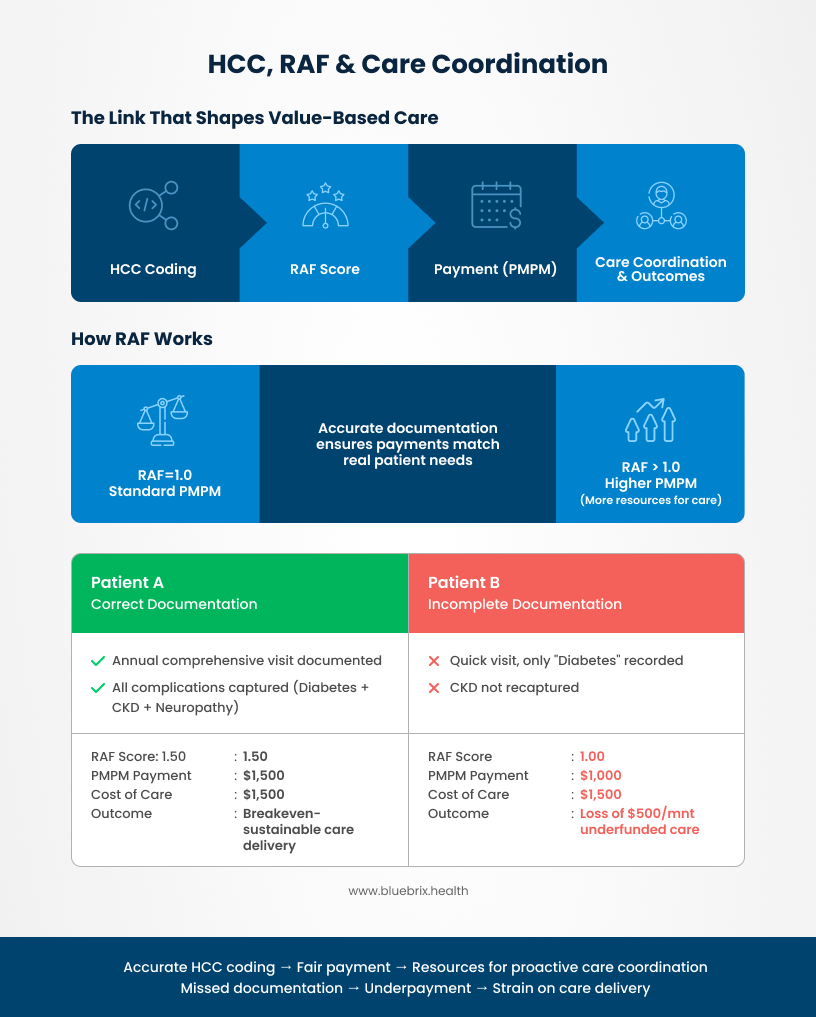
In this simple scenario, the organization loses $500 per month for Patient B because the documentation failed to reflect the true financial burden of her illness. The organization has to spend $1,500 to provide quality care, but it only received $1,000 in revenue to cover it.
For VBC leaders, HCC accuracy is a high-stakes revenue and compliance priority.
The HCC/coordination solution: Care coordination is the operational mechanism that mitigates this risk. Integrated care teams ensure that patients with chronic conditions are proactively engaged early in the year for comprehensive wellness visits. This targeted outreach guarantees the necessary annual documentation, enabling accurate capture of chronic conditions and maintaining the financial foundation. Furthermore, accurate HCC coding provides the crucial, detailed “digital twin” of the patient, allowing care teams to precisely stratify risk and allocate high-touch resources where they are most needed.
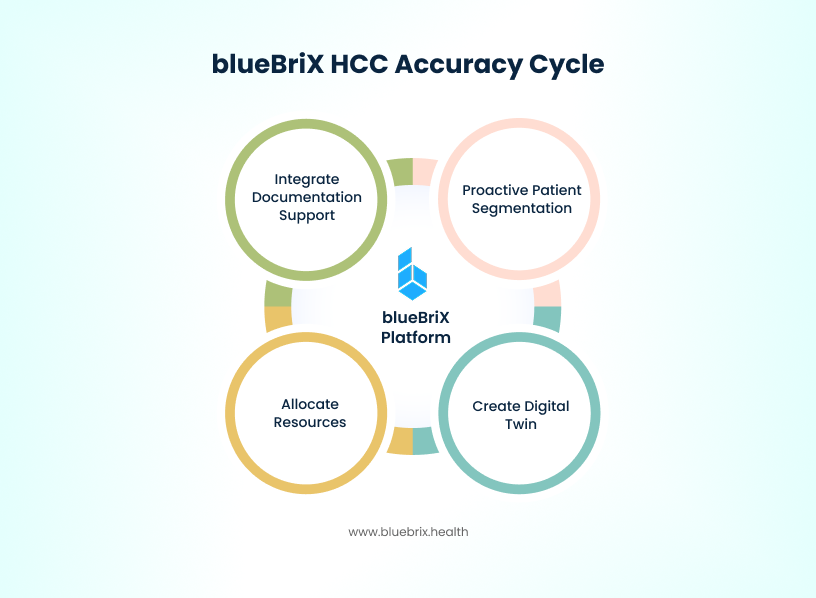
How does blueBriX help improve HCC accuracy?
For accurate HCC coding, a platform like blueBriX helps by addressing the critical gap between clinical service delivery and the required meticulous annual documentation:
- Integrated documentation Support: blueBriX provides decision-support tools and diagnosis alerts directly within the clinical workflow, which flag past HCC diagnoses and encourage providers to capture and document all active chronic conditions during patient encounters, rather than focusing only on the presenting problem. This improves documentation specificity, a requirement for HCC accuracy.
- Proactive patient segmentation: By consolidating patient data, blueBriX allows care teams to accurately stratify populations based on their predicted risk (RAF score). This precise segmentation enables care coordination teams to prioritize outreach and schedule comprehensive wellness visits early in the year specifically for high-risk patients, ensuring the necessary annual recapture of chronic conditions required to maintain the accurate RAF score and revenue integrity.
- Creating the digital twin: Accurate HCC coding paints a detailed picture of the patient’s complexity—a “digital twin” in the system. blueBriX sustains this digital twin by ensuring accurate data is collected, which in turn allows the care team to allocate high-touch resources effectively based on the true burden of illness, thereby supporting both clinical necessity and proper reimbursement.
PILLAR 2: HEDIS and clinical outcomes
The purpose of Value Based Care is to deliver better care, and HEDIS is the standardized scorecard that proves it. HEDIS measures are utilized by over 90% of U.S. health plans and over 190 million enrolled individuals, making it the industry standard for benchmarking quality.
High HEDIS performance is crucial because it leads to higher Star Ratings and quality bonuses, which are essential for VBC financial success. The measures focus on critical preventative services and chronic disease management, such as timely cancer screenings, blood pressure control rates, and appropriate follow-up care.
HEDIS and care coordination
Care coordination is the indispensable operational engine that executes the clinical tasks necessary to close gaps in care and achieve high HEDIS quality scores.
Here is a breakdown of how care coordination drives HEDIS success:
1. The Execution – Closing care gaps
HEDIS success is defined by ensuring patients receive critical preventative services and chronic disease management according to established guidelines. Care coordination teams are the ones responsible for achieving this compliance by addressing the operational and social barriers that prevent patients from receiving care:
- Proactive outreach: HEDIS measures include items like timely cancer screenings (e.g., mammography, colorectal cancer screening) and flu shots. Care coordination teams proactively engage patients to schedule and complete these preventative services, directly boosting HEDIS performance.
- Adherence to protocols: For chronic conditions, HEDIS tracks specific clinical markers, such as A1C levels for diabetic patients or blood pressure control rates. Care management services, provided by specialized teams, help members adhere to their treatment plans, which improves these measurable outcomes.
2. The mechanism – improving care processes
Care coordination focuses on organizing an individual’s care across multiple providers to reduce fragmentation. This organization directly correlates with better quality metrics, particularly in care processes that involve sharing information:
- Information sharing: Coordination involves ensuring that patient information—such as medical records or test results—is available to all doctors during a visit and that medication regimens are discussed.
- Managing transitions: HEDIS includes measures related to follow-up care, such as post-discharge visits or medication reconciliation. Care coordination services, like Transitional Care Management (TCM), are designed specifically to manage these handoffs, ensuring continuity of care and improving follow-up adherence, which directly impacts HEDIS-related readmission rates.
3. The experiential link
The association between effective coordination and quality is empirically established. Studies have concluded that beneficiaries who reported better care coordination—for instance, noting that their doctors were informed about specialist care or discussed their medications—also received higher-quality clinical care, leading to higher HEDIS performance scores.
In essence, HEDIS is the score, and care coordination is the strategy required to produce that score. High HEDIS scores require closing these gaps in care. But closing gaps is a coordination problem—not a clinical one. It means ensuring that specialist referrals are managed efficiently, that data is shared between primary care and the specialty site, and that patients adhere to their treatment plans.
Beneficiaries who report better care coordination (e.g., their doctors seemed informed about specialist care or discussed medications) also received higher-quality clinical care, leading to higher HEDIS performance scores.
The HEDIS/coordination solution: Proactive care coordination teams are the catalyst for quality. They move beyond basic appointment reminders, utilizing Social Workers and Community Navigators to address social determinants of health (SDOH), which are often the true barriers to adherence. By managing referrals and executing targeted outreach for preventative services, coordination teams directly ensure compliance with the critical measures that drive quality bonuses.
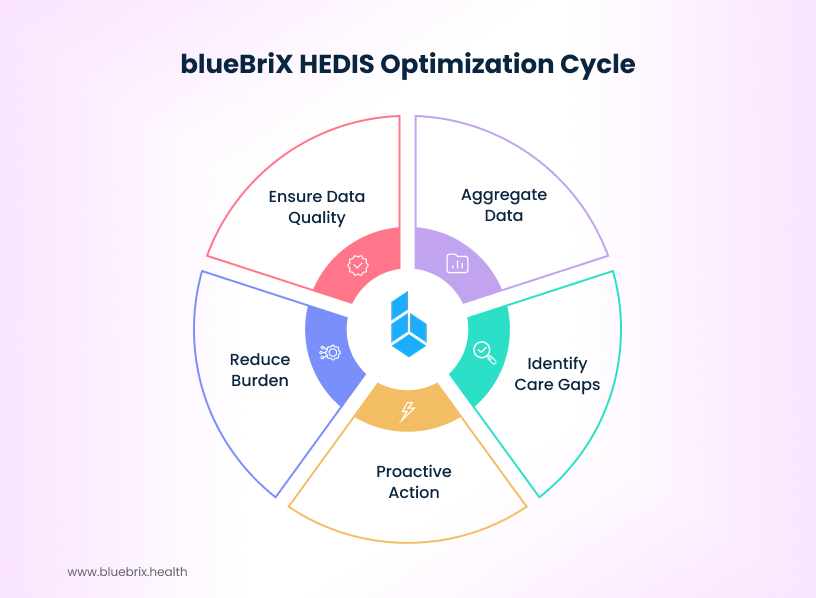
How does blueBriX help improve HEDIS score?
An EHR and integration agnostic platform like blueBriX serves as the essential digital infrastructure for HEDIS optimization by overcoming data fragmentation. This functionality dramatically improves performance in three key ways:
- Eliminates data silos for real-time gap closure: The platform aggregates comprehensive VBC data from diverse sources—including claims, clinical registries, and various EHRs—into a single, unified view. This integrated system provides the care coordination team with real-time insights, allowing them to instantly identify and proactively act on HEDIS care gaps (e.g., missed screenings or follow-ups) rather than relying on delayed, retrospective reports.
- Reduces administrative burden: By consolidating data and automating the process of identifying completed care, the platform significantly reduces the manual effort and time traditionally spent on retrospective chart review for HEDIS reporting.
- Future-proofs quality measurement: The platform aligns with the industry’s shift toward fully digital HEDIS, leveraging Electronic Clinical Data Systems (ECDS) and the FHIR standard. By consuming and transforming ECDS, the system ensures the high data quality required for automated, interoperable quality measurement, guaranteeing that achieved quality results are accurately captured for incentive payments.
PILLAR 3: MLR and operational efficiency
The Medical loss ratio serves as the financial accountability metric in VBC, defined as the ratio of money spent on medical expenses compared to the total premium revenue collected:
For Medicare Advantage, the minimum statutory requirement is 85%. Falling below this threshold for multiple years triggers severe penalties, including rebates to CMS, a ban on new member enrollment, and ultimately, contract termination.
MLR & care coordination
The VBC financial goal is to spend the right amount, efficiently, ensuring every dollar contributes to a positive outcome. High-cost, avoidable utilization—such as Emergency Department (ED) visits and 30-day hospital readmissions—blows up the Medical Expense (the numerator), immediately straining the MLR.
- The cost of fragmentation: Disjointed care directly leads to costly acute events.
- The coordinated intervention: Coordination is the antidote. Investing in Transitional Care Management (TCM), for instance, involves robust follow-up after a hospital discharge to prevent continuity gaps. Studies on TCM have shown a direct association with significant cost reductions and fewer 30-day readmissions.
The MLR/coordination solution: Care coordination is the primary MLR optimization lever. By investing proactively in staff and processes, VBC organizations stabilize the MLR by reducing the most expensive utilization events, demonstrating that coordinated care is a core financial investment, not an administrative overhead.
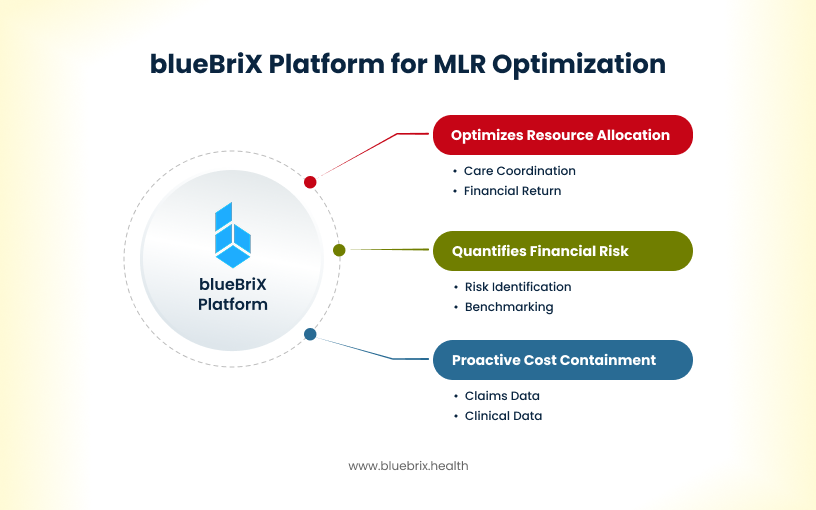
How does blueBriX help optimize MLR?
For optimizing the Medical Loss Ratio, which requires minimizing avoidable medical expenses, blueBriX provides the necessary data infrastructure for proactive financial control:
- Enables proactive cost containment (TCOC): The platform aggregates comprehensive claims and clinical data into a unified, real-time system, providing visibility into Total Cost of Care (TCOC) performance. This allows leadership to monitor component cost drivers (like avoidable Emergency Department utilization or post-acute spend) and spot early risk signals weeks or months before claims settlement, enabling proactive intervention rather than reactive, historical reporting.
- Quantifies and prioritizes financial risk: By analyzing the aggregated data, the platform instantly identifies and benchmarks potential financial opportunities, up to 10,000 possibilities quantified by dollar impact. This intelligence directs the care coordination team to the highest-risk patients and providers, ensuring that the investment in staff and processes (e.g., Transitional Care Management) is precisely targeted to prevent the most expensive utilization events, such as 30-day readmissions, which directly lowers the MLR numerator.
- Optimizes resource allocation: The resulting efficiency ensures resources are deployed where they yield the highest financial return, demonstrating that proactive care coordination is a core financial investment associated with measurable cost reductions.
Unifying the triad
Sustainable VBC success is achieved when the three pillars reinforce each other:
- Accurate HCC provides the revenue (premium) needed to invest in HEDIS gap closure.
- High HEDIS quality prevents costly acute events, keeping the MLR numerator low.
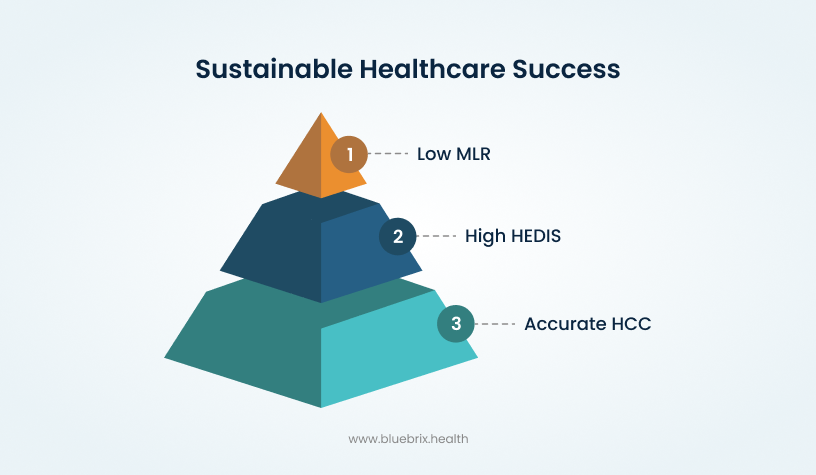
This interconnected system, however, relies entirely on data and operational alignment.
1. Mandate data interoperability and real-time analytics
Fragmented data is the single greatest barrier to KPI optimization. VBC success requires aggregating data from diverse sources—claims, registries, and various EHRs. Analytics platforms that provide quantified intelligence, will help moving beyond reactive, historical claims reports. You need real-time dashboards to monitor Total Cost of Care (TCOC) and spot risk signals weeks or months before a claim is settled. Furthermore, leaders must align technology investments with the future of digital quality measurement, leveraging FHIR (Fast Healthcare Interoperability Resources) standards to ensure seamless data exchange and reduce the burden of HEDIS reporting.
2. Align governance and team structure
KPI optimization cannot succeed in departmental silos (Finance managing MLR, Quality managing HEDIS, Coding managing HCC). The structure must reflect the interdependence of the metrics. Cross-functional workgroups involving analytics, clinicians, operations, and coders helps better alignment. This ensures that care management functions are directly aligned with the goals of minimizing high-cost utilization (MLR) and capturing accurate complexity (HCC). Staff your integrated care teams—including RN Care Coordinators, Social Workers (MSW), and Community Navigators—to focus on specific patient segments with high-risk needs, ensuring that high-touch care is delivered efficiently and impactfully.
The blueBriX care coordination solution: a unified VBC operating system
The critical step is recognizing that VBC is less a financial challenge and more a technology problem solved by an operational imperative. You need a centralized operating system, not fragmented, siloed tools. This is the blueBriX value proposition. As an EHR and integration agnostic care coordination platform, blueBriX functions as the essential infrastructure that converts the strategic VBC imperative into operational reality. By aggregating all data sources (claims, clinical, and administrative), blueBriX eliminates data fragmentation. This real-time, unified visibility allows teams to proactively manage Total Cost of Care (MLR) by targeting costly utilization, instantly identify and close HEDIS care gaps for quality bonuses , and guarantee the annual recapture of chronic conditions for accurate Risk Adjustment (HCC). The platform ensures the organization moves from reactive, historical reporting to proactive, high-ROI intervention, ensuring every strategic investment in coordination is measured and maximized against the unified MLR-HCC-HEDIS performance triad.
By leveraging a unified, data-driven care coordination strategy, your organization can transform the VBC triad from a set of compliance burdens into an integrated engine for predictable revenue, measurable quality, and sustained financial growth.