Licensure compacts let healthcare professionals practice across state lines with fewer barriers. Instead of getting a new license for every state, providers can work in multiple states under one streamlined process. This blog breaks down how compacts work, their benefits, and what they mean for behavioral health providers and organizations.

The behavioral health field is steadily evolving from a traditionally local model to a more connected, multi-state approach. This shift is fueled by several factors, including advancements in technology, changing patient expectations, and the ongoing need to address workforce shortages. For behavioral health providers, administrators, and technology vendors alike, navigating multi-state licensing has become an important step toward expanding access to care, supporting organizational growth, and ensuring long-term operational stability.
Why Multi-State Practice is Now a Necessity
The traditional model of behavioral health care, confined by state-specific licensure, is increasingly ill-equipped to meet the demands of modern society. Several key drivers underscore the urgent need for cross-state practice:
- Telehealth Revolution: The exponential growth of telehealth, accelerated by the recent global health crisis, has shattered geographical barriers. Patients now expect to access care regardless of their physical location, and providers are keen to leverage technology to expand their reach. However, without multi-state licensure, the promise of telehealth remains largely unfulfilled.
- Mobile Teams and Shifting Populations: As individuals and families become more mobile, the need for continuity of care across state lines has intensified. Military families, students, and those who relocate for work often face significant disruption in their behavioral health services due to licensing limitations.
- New Demands and Workforce Shortages: The demand for behavioral health services continues to outpace the supply of qualified professionals. Multi-state practice offers a powerful solution by enabling providers to serve underserved areas and address critical workforce gaps.
Challenges for Multi-State Providers
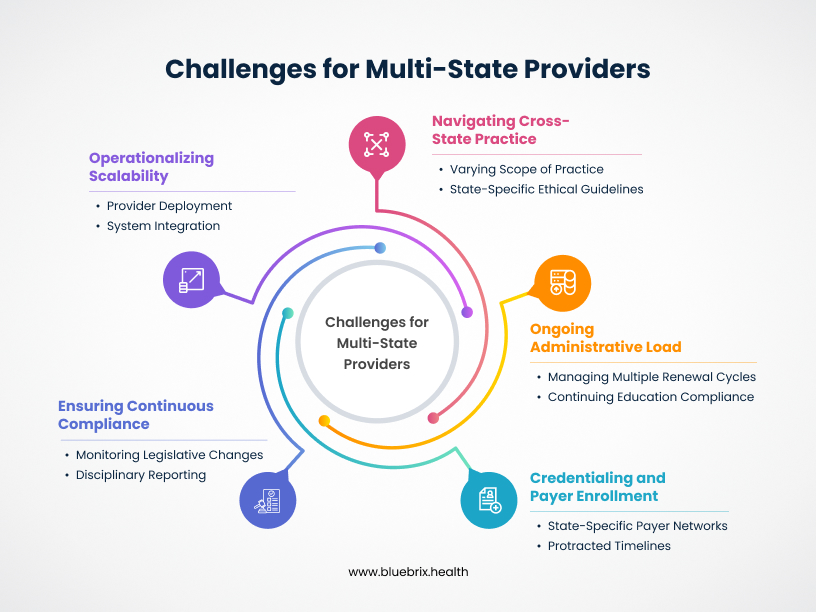
While licensure compacts have undoubtedly simplified the initial hurdle of cross-state practice, holding a compact license isn’t a “set it and forget it” solution. Behavioral health providers who have embraced this new era often encounter a secondary layer of complexities. These challenges, if not managed proactively, can still drain resources, increase compliance risk, and limit the true potential of multi-state operations.
Navigating the Nuances of Cross-State Practice
Even with compact privileges, the landscape isn’t perfectly uniform. Providers must contend with:
- Varying Scope of Practice: A psychologist’s scope of practice might differ slightly between their home state and a compact state. Similarly, a counselor’s ability to provide certain services or diagnose conditions may vary. Misinterpretations can lead to unintentional non-compliance.
- State-Specific Ethical Guidelines: While core ethical principles remain consistent, individual states may have unique ethical mandates or reporting requirements that apply to out-of-state practitioners.
- Payer Requirements and Reimbursement Rules: Just because you’re licensed to practice in a state doesn’t automatically mean you’re credentialed with all local payers or that their reimbursement rules for telehealth or specific services will align with your home state’s. This often remains a state-by-state hurdle.
The Ongoing Administrative Load
The paperwork pile-up doesn’t entirely disappear with compacts; it merely changes form. Providers and organizations still face:
- Managing Multiple Renewal Cycles: While not full licenses, compact privileges often have their own renewal processes and timelines, distinct from a provider’s home-state license. Tracking these various deadlines for a team of multi-state providers can become an administrative headache.
- Continuing Education (CE) Compliance: Different states, even within a compact, may have specific CE requirements or approved CE providers. Ensuring each provider maintains compliance for every jurisdiction they serve adds complexity.
- Documentation and Record-Keeping Variations: Some states might have specific requirements for electronic health records (EHRs), patient consent, or initial assessment documentation that differ from your home state.
Credentialing and Payer Enrollment Complexity
Perhaps one of the most significant and persistent challenges for multi-state providers is navigating the labyrinth of payer enrollment:
- State-Specific Payer Networks: Insurance networks are often state-bound. A compact license permits you to practice, but securing reimbursement requires individual credentialing and contracting with each payer in every state where your patient resides.
- Protracted Timelines: Payer enrollment processes are notoriously lengthy, often taking 90-180 days per payer per state. For organizations scaling into new compact states, this can create significant revenue delays.
- Evolving Requirements: Payer requirements for credentialing, re-credentialing, and even telehealth-specific billing can change frequently, demanding constant vigilance and adaptation.
Ensuring Continuous Compliance and Risk Mitigation
With an expanded footprint comes expanded regulatory scrutiny:
- Monitoring Legislative Changes: State legislatures continually update laws pertaining to behavioral health and telehealth. Staying abreast of these changes across all compact states of practice is a formidable task.
- Disciplinary Reporting Across Jurisdictions: Compacts facilitate the sharing of disciplinary actions. Providers and organizations must understand how adverse action in one state could impact practice privileges across all compact states and ensure timely, accurate reporting.
- Data Security and Privacy: While HIPAA provides a federal baseline, states may have additional, stricter privacy laws (e.g., related to substance use disorder records or minors’ consent) that must be adhered to in the patient’s location.
Operationalizing Scalability for Multi-State Teams
For larger organizations or growing practices, managing a team of multi-state licensed providers introduces new operational complexities:
- Provider Deployment and Resource Allocation: Efficiently assigning providers to patients in different states based on their compact privileges requires sophisticated tracking.
- Training and Onboarding: Ensuring all providers are fully aware of and compliant with the specific rules of every compact state they serve demands robust training programs.
- System Integration: Integrating licensing, credentialing, scheduling, and behavioural health EHR systems across multiple states to provide a seamless operational flow can be a significant technical hurdle.
Strategies for Maximizing Your Multi-State License Success
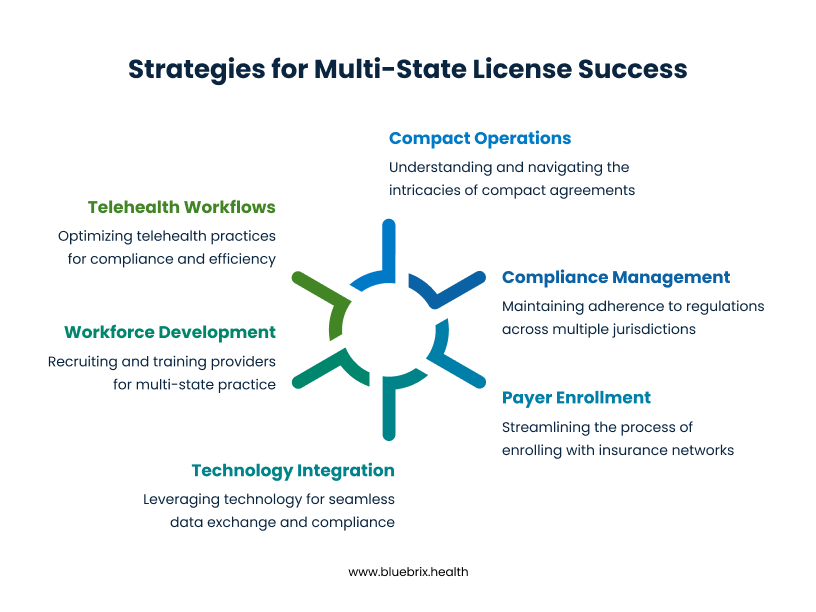 Having a multi-state compact license is a powerful asset, but unlocking its full potential requires a strategic approach to overcome the remaining complexities. By implementing smart processes and leveraging the right tools, providers and organizations can truly thrive in the multi-state landscape.
Having a multi-state compact license is a powerful asset, but unlocking its full potential requires a strategic approach to overcome the remaining complexities. By implementing smart processes and leveraging the right tools, providers and organizations can truly thrive in the multi-state landscape.
Deep Dive into Compact Operations
Don’t just get the compact; understand its intricacies:
- PSYPACT’s E.Passport and IPC: For psychologists, recognize that the E.Passport is for telepsychology, while the Interjurisdictional Practice Certificate (IPC) allows for temporary in-person practice. Understand the duration limits for temporary practice and any specific requirements for each.
- Counseling and Social Work Privileges: For counselors and social workers, grasp the specific process for applying for “privileges to practice” in each desired compact state. While streamlined, it’s not always automatic and may still involve state-specific fees or attestations.
- Home State vs. Remote State Rules: Always prioritize understanding the regulations of the state where the client is physically located. While your home state license is foundational, the “remote” state’s laws often dictate scope of practice, informed consent, and emergency protocols for that specific client encounter.
Proactive Compliance Management
Staying compliant across multiple jurisdictions requires a disciplined approach:
- Centralized Compliance Calendar: Develop a comprehensive calendar that tracks not only your home state license renewal but also all compact privilege renewal dates, continuing education (CE) deadlines, and any specific state reporting requirements (e.g., quarterly usage reports for PSYPACT).
- Streamlined CE Tracking: Identify CEs that are broadly accepted across compact states. Consider platforms that automatically track and verify CE units against multiple state board requirements. Be mindful of any state-specific “cultural competency” or “ethics” CE mandates.
- Regular Regulatory Scans: Designate a team member or leverage a technology solution to regularly monitor legislative and regulatory changes in all compact states where you practice. This includes changes to scope of practice, telehealth regulations, and new mandatory reporting laws.
Streamlining Payer Enrollment
This is often the longest pole in the tent, but strategies exist to accelerate it:
- Prioritize Payer Networks: Identify the most prevalent insurance networks in the compact states you wish to serve based on patient demographics and referral patterns. Focus your enrollment efforts strategically.
- Utilize CAQH ProView: Ensure your CAQH ProView profile is meticulously updated, comprehensive, and attested every 120 days. Many payers pull provider data directly from CAQH, making this a critical foundation for efficiency.
- Consider Delegated Credentialing: For larger organizations, explore delegated credentialing agreements with major payers. This allows your organization to conduct the primary source verification, significantly speeding up the payer’s internal approval process.
- Invest in Payer Enrollment Expertise: Whether internal staff specializing in payer enrollment or a third-party service, having dedicated expertise can navigate the unique application forms, follow-up processes, and negotiation points for each payer.
Optimizing Telehealth Workflows
Compacts are a boon for telehealth; ensure your operations are optimized:
- Consistent Informed Consent: Develop a multi-state informed consent document that covers general telehealth risks and includes specific language for each state’s unique requirements (e.g., emergency protocols, data privacy, minor consent).
- Emergency Protocols: Establish clear, multi-state emergency protocols for telehealth sessions, including local emergency contacts and resources for patients in remote states.
- Technology for Compliance: Ensure your telehealth platform and EHR can capture and manage state-specific documentation requirements and offer secure, compliant communication features suitable for all jurisdictions.
- Geofencing and Location Verification: Implement tools or protocols to verify the patient’s physical location at the start of each session, ensuring you are legally practicing within a compact state.
Building a Future-Ready Workforce
Leverage compacts for strategic growth and talent management:
- Targeted Recruitment: Actively recruit providers who either already hold compact licenses or are eligible and willing to obtain them, expanding your talent pool beyond single-state boundaries.
- Flexible Deployment: With multi-state licensed providers, organizations gain unparalleled flexibility to deploy staff where demand is highest, reassigning providers to different states as needed, especially beneficial for sudden surges in demand or in addressing specific geographic shortages.
- Professional Development: Support providers in understanding and navigating the nuances of multi-state practice, potentially offering internal training programs or access to specialized consultants.
Leveraging Technology and EHR Systems
Your behavioural health EHR and supporting tech stack must evolve to match the complexity of compact-enabled care delivery:
- Interoperability First: Choose behavioural health EHRs that support seamless data exchange across state lines, especially those integrated with HIEs and capable of syncing with other providers’ systems.
- State-Specific Customization: Configure your behavioural health EHR to reflect state-level nuances in documentation, billing, and compliance. This includes differential coding rules, informed consent formats, and required disclosures
- Credentialing and Privileging Dashboards: Use technology to track provider licenses, compact privileges, payer enrollments, and CE credits—ensuring real-time visibility into who can practice where, and when.
- Data Security & Access Control: Implement strict access management protocols to maintain HIPAA compliance across jurisdictions. Audit trails, role-based access, and location-aware permissions help prevent compliance violations as your organization scales.
How blueBriX Helps Multi-State Licensing in Behavioral Health
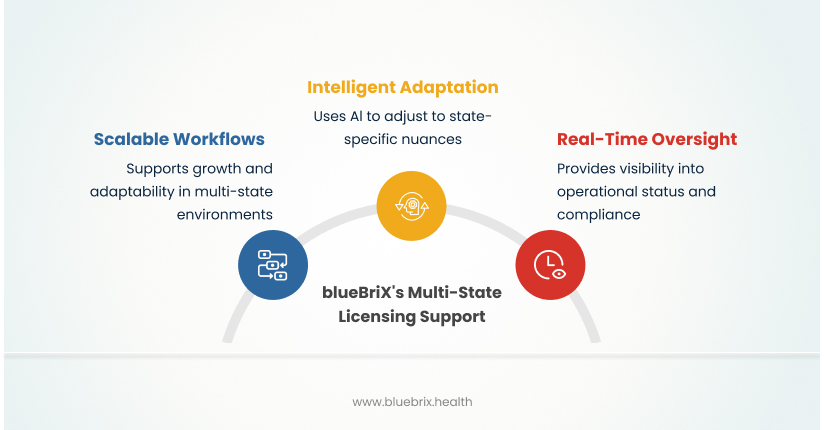
Scalable and Configurable Multi-State Workflows for Growth
The blueBriX platform’s architecture is fundamentally built for growth and adaptability in a multi-state environment. It supports custom workflow configurations and documentation templates that can be aligned precisely with individual state mandates and evolving compact regulations. This robust flexibility is crucial for organizations looking to expand:
- Seamless Market Expansion: Easily configure workflows, set up new compliance parameters, and integrate new state-specific operational protocols when entering new compact states, minimizing the setup time and ensuring immediate, compliant operations.
- Consistent Operational Practices: Implement standardized intake processes, clinical documentation templates, and billing procedures that intelligently adapt to state-specific rules without requiring entirely new, disparate workflows for each jurisdiction.
Intelligent Adaptation to Workflow Nuances and Regulatory Variations
The true power of blueBriX in operationalizing multi-state practice lies in its AI-powered PULSE agents, which dynamically adapt to the subtle, yet critical, state-specific nuances in regulations, documentation standards, and ethical guidelines that persist even within compact frameworks. This means:
- Automated Workflow Customization: Workflows and forms are automatically tailored to align with each jurisdiction’s specific operational requirements. For instance, this could involve dynamically adjusting fields for unique informed consent language required for telehealth in a particular compact state or adapting emergency protocols based on the patient’s physical location.
- Dynamic Scope-of-Practice Verification: The system can provide real-time alerts or guidance within the workflow if a provider’s planned clinical activity in a remote compact state might fall outside the specific scope of practice defined for their license type in that jurisdiction, preventing unintentional compliance breaches.
- Payer-Specific Operational Documentation: While compacts ease licensure, payer rules for documentation and billing often remain state-specific. blueBriX can help ensure that clinical notes and operational records meet the nuanced requirements of payers in each state, optimizing claims submission workflows and reducing denials. This minimizes time spent on post-session adjustments or audits.
Real-Time Operational Oversight and Strategic Deployment
blueBriX provides real-time visibility into the operational status and compliance posture of your multi-state practice. This includes:
- Centralized Provider Availability & Deployment: Quickly identify which providers are active, compliant, and available to serve patients in specific compact states at any given moment. This enables faster, more informed decisions for patient scheduling, workload balancing, and strategic provider deployment across states.
- Performance Monitoring & Utilization: Track key operational metrics related to multi-state practice, such as cross-state telehealth utilization per provider, credentialing bottlenecks in specific compact states, or provider workload distribution across jurisdictions, enabling data-driven operational adjustments.
Building a More Accessible and Inclusive Behavioral Healthcare Future, Together
Multi-state licensing, primarily through the advent of licensure compacts, is a transformative force in behavioral health. For providers who have already embraced this opportunity, the next frontier lies in mastering the operational nuances and leveraging technology to truly maximize their advantage. It addresses long-standing challenges, unlocks new opportunities for growth and service, and ultimately contributes to a more accessible, efficient, and patient-centered healthcare system. By understanding the necessity, embracing the solutions, and actively participating in this evolving landscape, we can collectively build a better behavioral healthcare future for all. Book a demo today and discover how we support behavioral health practices at every level of growth.
Frequently Asked Questions
State-by-state licensing restrictions limit behavioral health providers from delivering care across state lines—especially to patients in rural or underserved areas. This delays access to essential mental health services. For providers, these limitations reduce flexibility, restrict career mobility, and contribute to burnout. The inability to easily expand their reach or respond to demand in other states adds unnecessary strain to an already overburdened workforce.
Managing licenses in multiple states is a major administrative burden. Each state has different forms, fees, background checks, and continuing education requirements—resulting in hidden costs and significant time loss. On top of that, varying state laws and ethical standards make it easy to unintentionally fall out of compliance, even for experienced clinicians. This creates legal risk and complicates cross-state practice.
- PSYPACT (Psychology Interjurisdictional Compact): Allows licensed psychologists to provide telepsychology and temporary in-person services across participating states, significantly broadening their reach and facilitating continuity of care. To practice under PSYPACT, psychologists need an active, unencumbered license in a PSYPACT state and must obtain an E.Passport and/or Interjurisdictional Practice Certificate (IPC) from ASPPB.
- Social Work Licensure Compact: This compact is designed to allow licensed social workers to practice across state lines with a single, multistate license, drastically reducing administrative burdens and licensing delays. This enhances professional mobility and expands access to services for underserved populations. Multistate licenses are anticipated to be issued by the end of 2025, with full rollout potentially into early 2026.
- Counseling Compact: Empowers Licensed Professional Counselors (LPCs) to practice in other compact member states without needing multiple individual licenses. This offers greater flexibility, reduces administrative overhead, and supports consistent client relationships. The Counseling Compact is set to begin issuing practice privileges in late summer or early fall of 2025.
Yes, the movement towards licensure portability is expanding beyond these initial compacts. Initiatives for Marriage and Family Therapists (MFTs) and Substance Use Disorder (SUD) Counselors are actively in their planning stages. While specific timelines are still being developed, these efforts signal a significant industry-wide shift towards more integrated and efficient nationwide licensure for behavioral health professionals, aligning with the broader goal of enhancing access and continuity of care through modern solutions.