In this new healthcare landscape, one specific appointment has risen to critical importance: the Annual Wellness Visit (AWV). Often misunderstood, the AWV is not a physical exam, but a strategic meeting designed to proactively plan for a patient’s health. However, in many settings, the AWV is still treated as a fragmented, administrative task. The true value of this visit is often lost in paperwork and disjointed systems. This is where the power of integrated care coordination comes in—connecting all the pieces of a patient’s health journey to turn the AWV from a simple checklist into a powerful, proactive health strategy.
The foundation of annual wellness visits
To understand how to maximize the value of an AWV, we must first understand what it is and what it isn’t.
What constitutes an AWV? (a brief overview)
Annual Wellness Visits (AWVs) are yearly preventive care appointments available to Medicare beneficiaries. These visits are designed to identify risk factors early, so that providers can develop a personalized prevention plan. Unlike traditional physical exams, AWVs do not involve a full head-to-toe examination or routine lab work. Instead, they emphasize proactive health management tailored to each patient’s current condition and long-term goals.
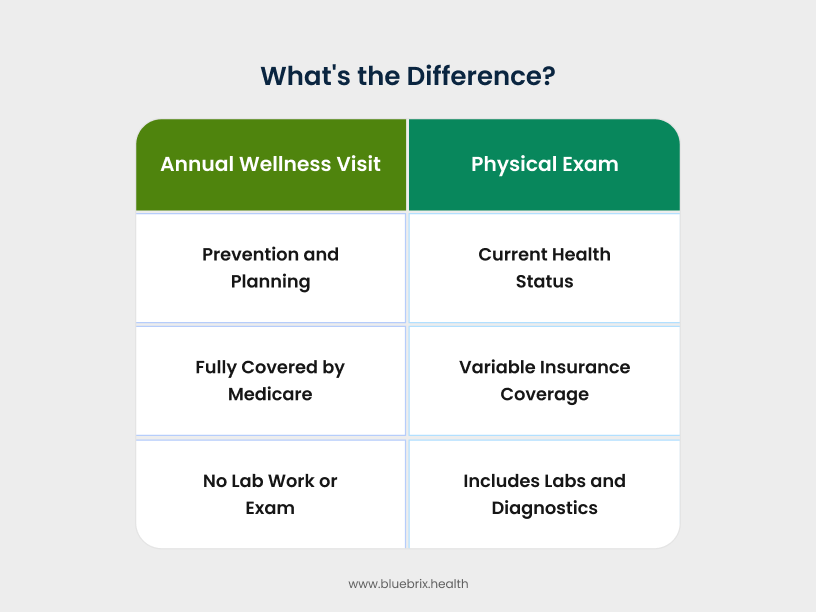
AWV vs. physical exam: what’s the difference?
An Annual Wellness Visit (AWV) differs significantly from a traditional physical exam—both in purpose and procedure. The AWV is designed to focus exclusively on preventive care and is covered under Medicare. It includes:
- A review of medical and family history
- Risk assessment for falls, functional ability, and safety at home
- Measurement of vital signs (height, weight, blood pressure, BMI)
- Cognitive and depression screenings
- Medication and specialist reviews
- Preventive service plan (immunizations, screenings, lifestyle advice)
Notably, an AWV does not include a full physical examination, lab tests, or hands-on evaluation—unless a specific symptom or condition warrants a need. It’s forward-looking and risk-oriented, serving as a foundation for proactive health management. For eligible Medicare patients, AWVs are fully covered with no out-of-pocket costs.
In contrast, a traditional physical exam is a more comprehensive, diagnostic visit. It typically involves:
- A full-body physical exam with physical touch
- Lab work or diagnostic testing as needed
- Evaluation of current symptoms or chronic conditions
- In-depth assessment of present health status
This type of exam is reactive by design—used to investigate, manage, or diagnose medical issues. Coverage for physical exams varies by insurance plan and may involve copays or patient responsibility.
Key components of the annual wellness visit (AWV)
The Annual Wellness Visit (AWV) is a structured opportunity for Medicare providers to engage in comprehensive, preventive care planning. Rather than focusing on diagnostics or physical exams, the AWV emphasizes early risk detection, health goal setting, and longitudinal care coordination.
Key components include:
- Health risk assessment (HRA): Patients complete a questionnaire covering demographic data, self-reported health status, lifestyle risks (e.g., tobacco use, nutrition, physical activity), psychosocial concerns, and social determinants of health. This forms the baseline for all personalized care planning.
- Medical and family history review: Providers review the patient’s past medical and surgical history, allergies, hereditary risk factors, current medications, and a list of all healthcare providers involved in the patient’s care.
- Routine measurements: Includes vitals such as height, weight, blood pressure, body mass index (BMI), and other measurements deemed clinically relevant based on patient history.
- Cognitive function screening: Using direct observation and validated screening tools, providers assess for signs of cognitive impairment, including early indicators of Alzheimer’s or other dementias.
- Depression screening: Standardized tools help assess risk of depression or other mood disorders—often an overlooked factor in chronic disease management and senior care planning.
- Functional ability and safety evaluation: Assessment of the patient’s ability to perform activities of daily living (ADLs), risk of falls, hearing impairments, and potential safety concerns at home.
- Personalized prevention plan development: Based on the patient’s risk profile and age, a forward-looking prevention strategy is developed, often covering the next 5–10 years. This plan outlines recommended screenings, immunizations, and care intervals.
- Health advice and preventive referrals: Tailored health counseling is provided, along with referrals to preventive services such as nutrition support, tobacco cessation programs, fitness interventions, and cancer screenings.
- Advance care planning (optional): If the patient opts in, providers can facilitate discussions around care preferences, living wills, medical power of attorney, and identification of caregivers or healthcare proxies.
The limitations of a traditional, fragmented AWV approach
In a traditional healthcare setting, the AWV is often a rushed and inefficient experience. A patient may arrive at their appointment, receive a paper form to fill out in the waiting room, and then spend the visit with a provider who is juggling multiple systems to gather the necessary information. This fragmented approach leads to missed opportunities and a reactive, rather than proactive, health plan.
The patient’s perspective: why are AWVs undervalued?
From a patient’s point of view, an AWV can feel like a transactional and unfulfilling visit. They might confuse it with an annual physical and, upon learning it’s just a conversation, may feel it’s unnecessary. The administrative burden falls on them, as they are asked to recall complex medical histories and fill out forms with little context. This often leads to patient disengagement and low attendance rates.
The provider’s perspective: administrative burdens and missed opportunities
For providers, the traditional AWV can be a source of significant administrative burden. The manual process of collecting data, entering it into an Electronic Health Record (EHR), and creating a prevention plan is time-consuming. This takes valuable time away from meaningful patient interaction. Furthermore, without a coordinated system, the provider may be unaware of a patient’s recent specialist visits or other critical health events, leading to a fragmented and incomplete view of their health.
The HCC score perspective: critical financial link
A fragmented AWV process often leads to incomplete Hierarchical Condition Category (HCC) capture. When chronic conditions are not accurately documented or updated annually, the patient’s risk score is understated. This often results in:
- Underpayment: The organization is not reimbursed fairly for the complex care they are providing.
- Sub-optimal care planning: Without a complete and up-to-date picture of a patient’s conditions, the care team cannot create the most effective plan.
This directly reduces risk-adjusted reimbursements, skews population health data, and can leave providers under-resourced for delivering appropriate care. Ensuring precise HCC capture during AWVs is therefore critical for both financial performance and accurate care management.
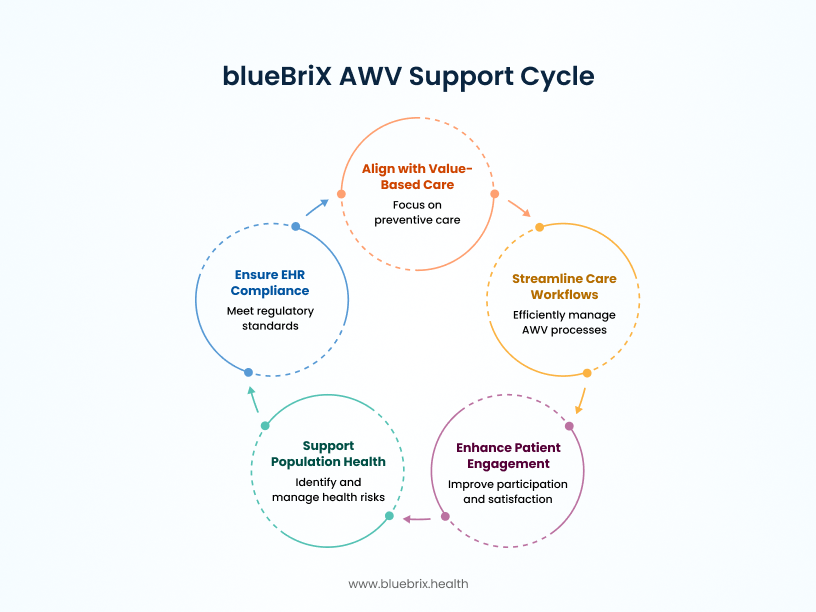
How integrated care transforms the AWV into a proactive health strategy
The solution to these challenges lies in a more connected approach: integrated care coordination.
At its core, integrated care coordination is about connecting every part of a patient’s health journey. Imagine the difference: a doctor seeing a patient with no record of a recent ER visit versus having a complete, real-time view of their health history. With that kind of insight, the Annual Wellness Visit evolves from a routine, box-checking appointment into a meaningful milestone that anchors a patient’s ongoing care plan for the year.
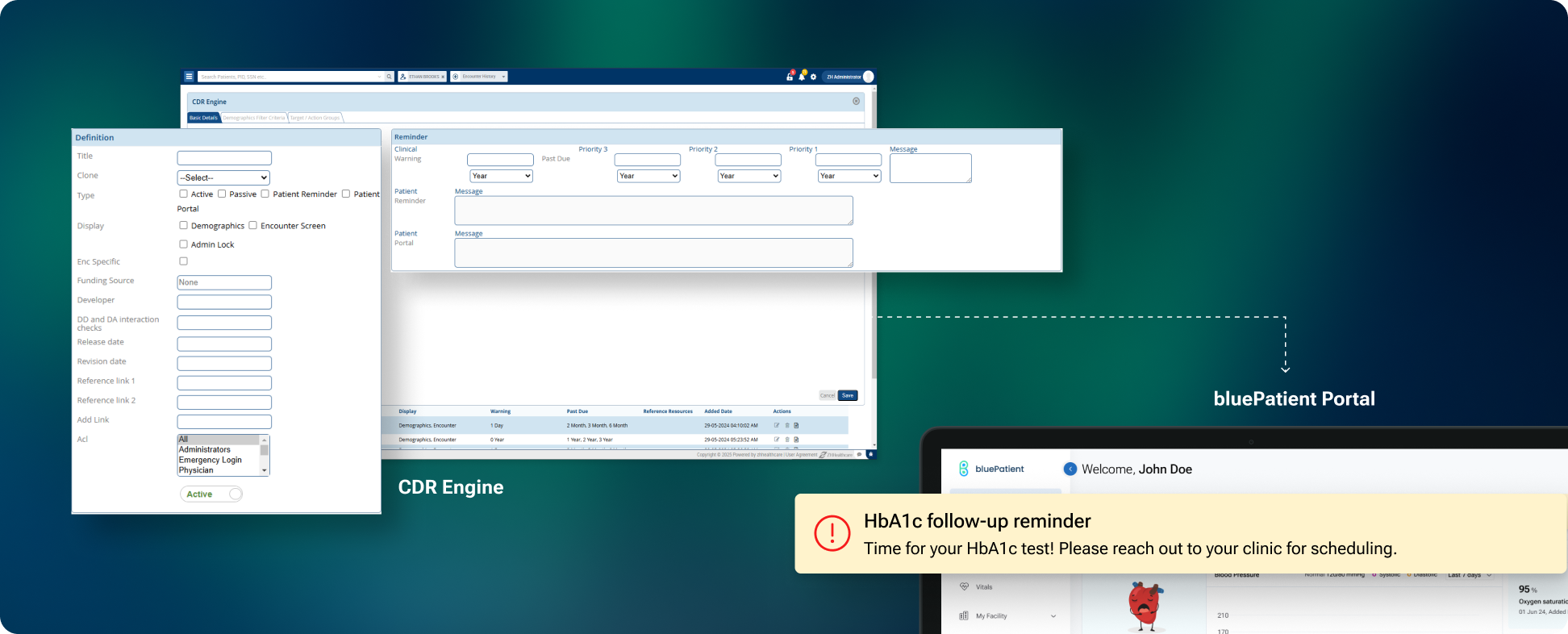
Imagine an AWV that begins weeks before the patient ever steps into the clinic. Automated reminders prompt scheduling, and the patient completes a digital Health Risk Assessment at home. By the time of the visit, the provider has comprehensive insights readily available, eliminating redundant data collection. The encounter shifts from administrative tasks to a focused, collaborative discussion on health priorities. Instead of checking boxes, the provider leverages a complete patient profile to capture chronic conditions accurately, address care gaps, and design a personalized plan that supports both outcomes and compliance.
Key components of integrated care coordination for annual wellness visits
- Patient engagement tools: These tools keep patients connected and involved. Think of remote patient monitoring (RPM) that can track a patient’s blood pressure or glucose levels between visits. Personalized health plans are accessible through a portal, making them a living document the patient can refer to and update. These tools turn the AWV into a year-long conversation, not a one-time event.
- Population health management: This is about moving from caring for an individual to caring for a whole community. This technology helps healthcare organizations identify at-risk patients who are due for an AWV or need a specific screening. This allows for proactive outreach, ensuring that the right patients get the right care at the right time.
- Seamless data integration: This is the backbone of the entire system. It’s the ability of a platform to pull data from multiple sources—EHRs, claims data, pharmacy records, and patient-reported information. This creates a unified patient record, giving the provider a complete picture without having to chase down information from different systems.
Leveraging blueBriX for a superior AWV experience
This is where the theoretical benefits of integrated care coordination become a practical reality with a platform like blueBriX.
blueBriX provides the digital infrastructure to transform the AWV process. It is a powerful platform that connects the key “building blocks” of value-based care: care coordination, patient engagement, and population health management. It’s designed to break down the silos that lead to fragmented care and inefficiency.
Here is an example showing how AWV works with blueBriX?
Meet Evelyn, a 72-year-old retiree managing a few chronic conditions and trying to stay ahead of her health. Like many Medicare patients, she hadn’t realized she was overdue for her Annual Wellness Visit. But this time, things would be different—because her provider was using blueBriX.
- It starts with smart identification: Behind the scenes, blueBriX’s population health engine flagged Evelyn as AWV-eligible. No manual tracking, no missed opportunities. The system sent a personalized message to Evelyn—first a friendly text, then an email reminder—inviting her to schedule her wellness visit. It didn’t feel like a generic blast. It felt intentional, proactive, and tailored. Evelyn booked the appointment with a single tap.
- Prepping before the visit—on her terms: Before her appointment, Evelyn received a link to her secure blueBriX patient portal. From her tablet at home, she completed her Health Risk Assessment, updated her medical history, and listed all her current medications. No paperwork, no waiting room clipboard. By the time she walked into the clinic, her provider already had access to everything—streamlined, structured, and ready for review. What used to take up half the visit now took none.
- A visit that feels like a conversation: At the appointment, Evelyn’s provider didn’t waste time gathering data. Instead, they opened the blueBriX platform—everything was already there. The conversation turned immediately to what mattered: Evelyn’s long-term goals, her diet, the joint pain she hadn’t mentioned before, and her wish to stay active for her grandkids. With just a few clicks, her provider created a personalized prevention plan, scheduled a bone density scan, and referred her to a health coach for joint mobility exercises. blueBriX tracked it all—no faxing, no follow-up chaos.
- After the appointment—the journey continues: Evelyn left the clinic, but her AWV didn’t end there. Her entire care plan was now available through the blueBriX patient engagement app. She got a push notification reminding her about the upcoming scan, a follow-up message from her health coach, and a refill reminder for her supplements. If she had a question, she could message her care team directly—no call center hold times, no confusion.
The measurable benefits of a coordinated AWV strategy
An integrated approach to AWVs delivers tangible, measurable results for everyone involved.
For providers
- Increased operational efficiency and reduced administrative burden: By automating patient outreach, pre-visit data collection, and documentation, providers can reclaim valuable time. The system’s ability to integrate data means less time spent hunting for information and more time spent on patient care. Besides accurate HCC coding makes sure providers are fairly reimbursed for the level of care they give and helps manage patient populations more effectively.
- Better performance on quality measures (e.g., MIPS/MACRA): The AWV is a key component of value-based care reporting. An integrated platform ensures all the necessary data is captured and documented correctly, helping providers meet and exceed their quality metrics and, in turn, increasing their reimbursement potential.
For patients
- Improved health outcomes: Proactive care, timely screenings, and continuous engagement lead to better management of chronic conditions and early detection of new issues. The patient is no longer a passive recipient of care; they are an active partner.
- Greater satisfaction and a feeling of partnership: Patients feel heard and valued when their provider has a complete understanding of their health history without having to ask the same questions repeatedly. The ease of communication and access to their care plan fosters a sense of partnership in their health journey.
- Reduced stress and confusion: The system streamlines referrals and follow-ups, eliminating the common patient frustration of navigating a complex healthcare system alone.
For healthcare organizations
- Increased revenue: Higher AWV completion rates, better documentation, and improved performance on quality measures directly translate into increased revenue from Medicare and other payers.
- Reduced costs: A proactive approach to care can prevent costly emergency room visits and hospitalizations. By managing chronic conditions more effectively, organizations can significantly reduce overall healthcare costs.
- Improved patient retention: When patients feel engaged and well-cared for, they are more likely to stay with a healthcare organization. The seamless, positive experience creates loyalty and a stronger, more stable patient base.