Your practice sees 200 diabetic patients annually. If just half of them have their diabetes properly documented and coded each year, that’s worth approximately $180,000 in additional revenue. Even though your EHR captures all the necessary patient data, you’re still experiencing this exact revenue leakage. That’s the reality for most healthcare practices using standard EHRs. You’re left with manual mapping to HCC codes, tracking chronic diseases across fragmented problem lists, and hoping nothing falls through the cracks during busy patient visits. The gap between what you should earn and what you actually receive often comes down to technology that wasn’t built for the complexity of risk adjustment.
Here in this blog, we will explore the critical challenges healthcare practices face with standard EHRs when it comes to meeting HCC-specific functionalities and discuss how blueBriX can help optimize financial reimbursement and streamline workflows for your organization.
Why standard EHRs struggle to meet HCC-specific functionalities?
Standard EHRs often fall short on the essentials like clean problem lists, precise HCC mapping, risk visibility, and seamless workflows—making accurate coding harder than it should be.
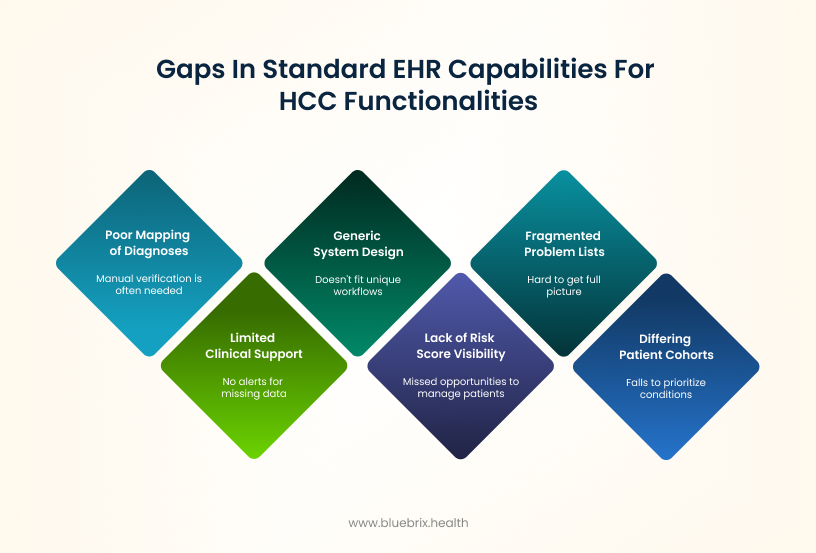
Not built for your unique care workflow
Most of the standard EHRs are built as generic systems that don’t fit the way you deliver care day-to-day. Instead of supporting your clinical routines, they impose rigid workflows that disrupt how you document, review, and code patient information. This creates friction, forcing clinicians to spend extra time fixing, duplicating, or working around the system just to get the job done. The end result? Inconsistent, incomplete documentation that hurts the accuracy of coding and your revenue.
Patient cohorts differ in complexity and needs
Standard EHRs rarely accommodate the unique characteristics of your patient cohorts, such as variations in chronic disease prevalence, socioeconomic factors, or care complexity. Without tailoring to your specific patient populations, these systems fail to prioritize or capture condition details critical to accurate risk adjustment. This gap results in underreporting of high-risk patients and incomplete risk profiles, reducing reimbursement accuracy and care management effectiveness.
Limited clinical decision support for HCC coding
Most EHRs don’t give you the clinical decision support they need for HCC coding. There are no alerts for missing MEAT (Monitor, Evaluate, Assess/Address, Treat) documentation, no prompts for chronic condition specificity, and no guidance on which diagnoses actually impact risk scores. You’re left to rely on memory—causing missed codes, incomplete documentation, and lost revenue.
Fragmented problem lists undermine chronic condition tracking
Patient problem lists in many EHRs are often outdated, incomplete, or poorly maintained across different providers. This fragmentation makes it hard for you to get a full, accurate picture of all active chronic conditions during visits.
As a result, you frequently miss reviewing or re-documenting existing chronic diseases—which is critical for accurate HCC coding and risk adjustment. For example, a diabetic patient’s CKD may go unrecorded if the problem list doesn’t highlight it, resulting in lost revenue and underreported patient risk.
Poor mapping of clinical diagnoses to HCC categories
Many standard EHR systems don’t automatically map ICD-10 codes to their corresponding HCC categories, forcing providers or coders to manually verify which diagnoses qualify for risk adjustment. This manual process often leads to missed nuances—such as diabetes with complications or specific CKD stages—that are crucial for accurate HCC coding. Without this precise mapping, patients may be under-coded, resulting in lower risk scores, reduced reimbursement, and increased audit risk.
Lack of risk score visibility at the point of care
Most EHRs don’t display a patient’s RAF score or alert you when risk levels change during visits. Without real-time visibility into how documentation impacts patient risk profiles and reimbursement, you miss opportunities to proactively manage high-risk patients or adjust care plans based on accurate risk stratification. This gap undermines value-based care effectiveness and can lead to patients not getting the intensive management they actually need.
Limited workflow integration
Without HCC tailored workflows built into daily clinical routines, reviewing and capturing all relevant conditions becomes a fragmented process. Most EHRs treat HCC documentation as an afterthought, while coding teams work from disconnected reports that arrive days after encounters. This forces you into time-consuming manual reviews and follow-up tasks outside patient visits. The result: missed chronic conditions, incomplete documentation, and lost reimbursement opportunities—all because the technology doesn’t support the workflow you actually need.
The costly consequences: what these gaps mean for your practice
These gaps in standard EHRs aren’t just technical flaws—they translate into financial losses, regulatory exposure, and missed opportunities that impacts your reimbursements, patient outcomes and of course patient are journey.
Revenue loss from inaccurate risk-adjusted payments:
When coding misses key diagnoses or yearly recaptures, your practice earns less than it should, directly impacting your reimbursement.
CMS audit exposure and compliance penalties:
Incomplete or incorrect documentation increases the chance of CMS audits, which can lead to steep fines, denied payments, or even suspension of Medicare billing privileges—putting your practice’s financial health at serious risk.
Compromised patient care due to missed clinical complexity:
Without accurate documentation of a patient’s full health status, care plans may fall short. This means you might miss identifying high-risk patients who need closer management, affecting outcomes.
Provider burnout from manual documentation tasks:
Manually tracking missing codes and reconciling fragmented data creates unnecessary administrative work, contributing to clinician frustration and burnout in already time-pressed environments.
Missed revenue from uncoded high-value diagnoses:
Complex chronic diseases that go uncoded represent missed legitimate revenue opportunities that could support practice growth and patient care investments.
Delayed clinical decisions without patient risk data:
Lack of real-time risk scores in your workflow hampers your ability to make informed decisions quickly, potentially delaying interventions that improve patient health.
The HCC-ready EHR checklist: essential features your system should have
HCC success starts with the right EHR features. From problem list management and AI-driven disease discovery to real-time RAF visibility and smart analytics, here’s your roadmap to smarter risk adjustment.

Comprehensive problem list management
A reliable EHR keeps your patient’s problem list clean, up-to-date, and focused on active chronic conditions. This matters because it gives you a quick snapshot of patient complexity—no more wasting time sifting through outdated or irrelevant issues dumped years ago. Clear problem lists mean you can deliver the right care and capture the right codes without extra hassle.
Automated disease discovery
AI-powered disease discovery in EHRs leverages machine learning and natural language processing technologies to automatically analyze clinical notes, lab results, and medication records. These systems identify potential diagnoses by detecting patterns and clinical markers that might have been missed or undocumented.
This automation reduces the time for manual chart reviews, improves the accuracy of diagnosis capture, and ensures that all relevant chronic diseases are documented properly for risk adjustment and reimbursement purposes. AI models used include predictive analytics and deep learning algorithms that continuously learn from new data to enhance diagnostic support and clinical decision-making.
Data aggregation & interoperability
While an EHR primarily stores clinical data from patient visits, it should also integrate data from external systems like insurance claims and social services databases. This integration uses interoperability standards and APIs to pull in relevant non-clinical and financial information, enriching the patient record.
By doing so, the EHR provides a more complete picture of patient health, including SDOH data that impact care. This comprehensive data supports accurate HCC coding and helps you make informed, holistic care decisions without needing to switch between multiple systems.
Seamless mapping to HCC categories
Manually matching diagnoses to coding categories is tedious and error-prone. Your system should leapfrog this by automatically mapping everything—from structured inputs to unstructured text notes—to the right HCC codes per CMS standards. This saves you time, reduces mistakes, and makes sure complex chronic conditions get recognized where they matter most.
Manual HCC mapping versus automated HCC mapping
| Manual HCC Mapping
(Standard EHR) |
Automated HCC Mapping (Smart EHR) |
|---|---|
|
Problem List
|
Problem List
|
Diagnoses (ICD-10)
|
Diagnoses (ICD-10)
|
HCC Categories
|
HCC Categories
|
Impact
|
Impact
|
Visibility into RAF scores and risk changes
Your EHR should include built-in RAF scoring models because Medicare releases official Risk Adjustment Factor (RAF) scores only once a year, not in real time. These integrated models estimate each patient’s current risk score using the latest clinical and claims data. By closely approximating the official Medicare scores, these EHR-generated RAF estimates help you to prioritize patients needing closer management and support data-driven decision-making about care complexity and documentation during clinical encounters, all within your workflow.
Smart analytics and workflow automation
Your EHR should have tools that analyze your entire patient population and practice data to identify the biggest coding gaps or opportunities—such as patients missing documentation for chronic conditions. Once identified, these tools proactively guide your team through alerts, task lists, or nudges so you can address these issues quickly and efficiently. This automation reduces the time spent on manual chart reviews and administrative follow-ups, helping you capture more accurate diagnoses, improve revenue, and free up clinical staff to focus on patient care rather than paperwork.
Support value-based care models at scale
Managing large patient panels under value-based contracts isn’t easy. Your EHR system should help by automating risk adjustment, tracking outcomes, and ensuring compliance—all at scale. This lets you focus on delivering high-quality care efficiently while maximizing your financial rewards.
Leverage blueBriX for effective HCC optimization
You don’t need to scrap your existing system. Instead, with blueBriX you can fix the fractures in your current system in accommodating HCC functionalities without disrupting workflows your team already knows. Our integration-agnostic platform connects seamlessly with your existing systems, making them communicate better and work smarter together.
Our no-code solution fills the gaps by adding real-time clinical decision support that flags missing MEAT documentation and prompts for chronic condition specificity right within your familiar interface. blueBriX automatically maintains clean problem lists and maps diagnoses to HCC categories in the background, while delivering RAF scoring insights at the point of care.
The platform uses smart analytics and automated alerts to help close coding gaps efficiently, all while preserving your team’s existing processes. By enhancing what you already have rather than replacing it, blueBriX optimizes HCC capture and maximizes reimbursement without the learning curve or workflow disruption of a complete system overhaul.