Part 1: The end of the pilot era
Welcome to the dual world
Ten years ago, value-based care (VBC) was a project. It was a pilot program with a small cohort of patients, managed by a dedicated team of nurses working off spreadsheets. It was manageable. It was contained. Today, VBC is the business model. But it’s a messy one.
We have entered what industry veterans call the dual world of risk. It is no longer sufficient to ask, Is this patient fee-for-service or value-based? The reality is far more complex. A single patient might be:
- Attributed to your MSSP ACO (Medicare Shared Savings Program).
- Simultaneously enrolled in a private Medicare Advantage (MA) plan.
- Receiving supplemental support through a direct primary care (DPC) membership or a specific disease management grant.
Each of these identities carries a different set of rules.
- The ACO wants you to lower Total Cost of Care (TCOC) and keep them out of the ER.
- The MA plan wants you to close HEDIS gaps and document risk adjustments (HCCs) with extreme precision.
- The DPC model demands a consumer-grade experience with high-touch access.
For your operational leadership (COOs) and financial leadership (CFOs), this overlap creates a dangerous blind spot. You are effectively running three different businesses for the same customer, using the traditional EHR that was designed for a fourth business (Fee-for-Service billing).
The swivel-chair crisis
The result of this dual world is the Swivel-Chair Crisis.
Walk into any care coordination center in the US today, and you will see the same scene: A highly trained nurse or social worker sits in front of two monitors. On the left screen is the EHR (Epic, Cerner, Athena). On the right screen is a browser with five tabs open:
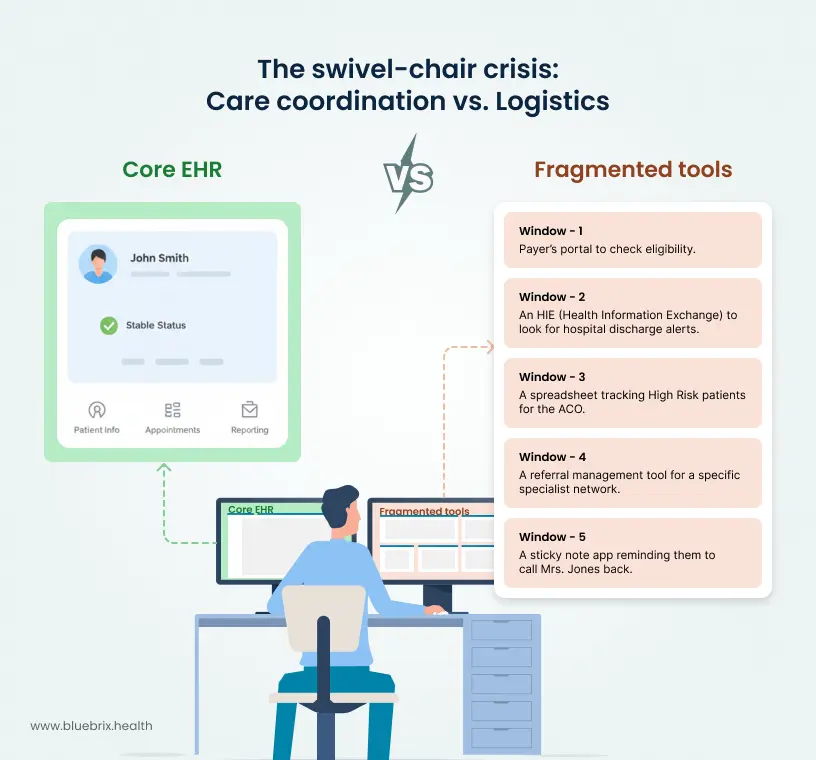
This care coordinator is not managing care; they are managing logistics. They are the human glue trying to hold together a fragmented system.
This isn’t just a workflow problem; it’s a unit economics problem. Every minute that coordinator spends swiveling between tabs is Dead OpEx—operational expenditure that generates zero value for the patient and zero revenue for the organization.
As you scale from 5,000 lives to 50,000 or 500,000, this human glue approach breaks. You simply cannot hire enough coordinators to swivel-chair your way to profitability.
Part 2: The new P&L of care coordination
To fix the problem, we must first quantify it. We need to stop treating Care Coordination as a cost center and start modeling it like an asset class with its own P&L.
The unit economics equation
The fundamental equation for the profitability of a risk-bearing organization is:
Net Margin = PMPM revenue + shared savings – medical loss + OpEx
Where:
- PMPM revenue: Capitation payments or management fees.
- Shared savings: The bonus for keeping the patient healthy (below benchmark costs).
- Medical loss: The cost of the actual healthcare services (claims).
- OpEx: The cost of your care team (salaries, technology, overhead).
In the dual world, two variables in this equation are under attack: revenue (due to Leakage) and OpEx (due to Friction).
1. The cost of friction (OpEx inflation)
Let’s look at the Scalability Math of a Care Coordinator.
- Fully loaded cost: $85,000/year (Salary + Benefits).
- Workable hours: ~1,800 hours/year.
- Cost per hour: ~$47.
If your coordinator spends 15 minutes per patient per month navigating the dual world friction (logging into portals, re-entering data, searching for faxes), the math gets ugly fast.
- Friction cost: 15 mins = 0.25 hours = $11.75 per patient/month in pure waste.
- Impact: If you are receiving a $20 PMPM care management fee, you just burned 58% of your margin on administrative friction.
This is why so many ACOs struggle to show ROI. They assume their staff is working on Care, but their staff is actually working on Data Entry.
2. The cost of leakage (revenue destruction)
Leakage is the silent killer of Value-Based Care.1 It happens when a patient moves outside of your coordination loop. In a Dual HCC world, leakage hits you twice:
A. Referral leakage (The immediate cost)
You refer a patient to a cardiologist. Because your coordination tools are fragmented, you don’t realize the patient went to an out-of-network provider or a high-cost hospital system.
Result: Your TCOC (Total Cost of Care) spikes. You miss your shared savings benchmark.
B. Data leakage (The future cost)
This is more insidious. Let’s say that out-of-network cardiologist diagnoses the patient with Congestive Heart Failure with Complications. Because they are not on your integrated platform, that diagnosis never makes it back to your primary risk view.
Result: You fail to capture the HCC (Hierarchical Condition Category) code.
Financial hit: The patient’s Risk Adjustment Factor (RAF) score remains low (e.g., 1.0 instead of 1.4). Next year, CMS pays you $3,600 less for that patient, even though their complexity is high.
The multiplier effect:
If you have 10,000 lives and you experience Data Leakage on just 5% of them (500 patients), and each leak costs you an average of $2,500 in missed risk adjustment:
$500 X $2,500 = $1.25 Million in Lost Revenue
This is money you earned by managing the risk, but lost because your coordination platform couldn’t close the data loop.
Part 3: Why more staff is the wrong answer
When faced with these problems, the traditional healthcare instinct is to throw bodies at it.
- The coordinators are overwhelmed? Hire 5 more.
- We’re missing HCC codes? Hire a team of coders to review charts.
This is the linear scaling trap.
In a Fee-for-Service world, revenue scales linearly with volume (more visits = more money), so hiring more staff makes sense. In a value-based world, revenue scales with efficiency.
If you hire more staff into a broken, high-friction workflow, you are simply scaling your inefficiency. You are increasing your fixed OpEx without solving the root cause of the margin erosion. You are adding more swivel chairs to the room.
The diminishing returns of human warehousing
There is also a management tax. As your coordination team grows from 10 to 50 to 100, the complexity of communication grows exponentially. Handoffs become the most dangerous moment in a patient’s journey.
- Coordinator A handles the MA requirement.
- Coordinator B handles the ACO requirement.
- Coordinator C handles the Social Determinants (SDOH) referral.
Without a central brain which works like an orchestration layer, Coordinator A doesn’t know what Coordinator B did. The patient gets three different phone calls asking the same questions. Patient satisfaction drops. Engagement drops. And the dual world friction wins.
Part 4: The solution—The orchestration layer
So, how do you solve the Unit Economics problem without bankrupting the organization on a massive EHR replacement project?
You adopt an Orchestration Strategy.
What is an orchestration layer?
An Orchestration Layer is a technology platform that sits between your core systems (EHR, Billing) and the outside world (Payers, Patients, Community Partners).
It does not replace your EHR. It makes your EHR usable for value-based care.

blueBriX is built specifically for this purpose. It is a Care Coordination Orchestration Platform. Think of it as the air traffic controller for your patient risks.
How blueBriX fixes the math
1. Unifying the risk view (killing the friction)
blueBriX connects to your existing data sources—EMRs, Claims feeds, ADT (Admission-Discharge-Transfer) feeds, and Wearables. It ingests this messy, fragmented data and normalizes it into a Single Longitudinal Patient Record.
- The Workflow Shift: The care coordinator logs into one screen. They see the patient’s clinical history (from the EHR), their risk gaps (from the MA plan), and their utilization alerts (from the ACO).
- The Economic Impact: The 15 minutes of friction drops to near zero.
- The Result: Your existing team can manage 25-30% more lives without burnout. You have effectively lowered your OpEx per life by 30%.
2. The listener architecture (plugging the leaks)
blueBriX uses a unique Listener architecture. These are automated workflows that listen for specific events in the data stream.
For example, a listener detects that a patient was discharged from the ER (via an ADT feed). It automatically triggers a task for the coordinator: Call Patient X for Transitional Care Management (TCM) within 48 hours. It simultaneously alerts the billing team to capture the TCM revenue code.
This closed-loop logic ensures that no revenue opportunity (TCM is high-margin) and no clinical risk (readmission prevention) slips through the cracks.
3. Adaptability via low-code (future-proofing)
The dual world is constantly changing. CMS changes the rules for ACOs every year. MA plans change their gap requirements every quarter.
Traditional software is rigid. Changing a workflow in a legacy EHR can take 12 months and $500k in consulting fees.
blueBriX is built on a Low-Code/No-Code framework.
- Problem: A new payer contract requires you to track Food Insecurity as a risk factor.
- blueBriX Solution: Our team can drag-and-drop a new module into the care pathway in an afternoon, get it tested quickly for your environment and release it within days. No 6-month delay.
This agility allows you to align your Tech OpEx strictly with your Revenue Opportunities. You are never paying for bloatware you don’t use, and you are never waiting on IT to capitalize on a new contract.
Part 5: Strategic implementation — the wrap, don't rip approach
The biggest fear for COOs and CIOs is implementation trauma. The idea of ripping out an EHR or migrating data is terrifying.
The Orchestration approach avoids this entirely. We call it Wrap and Extend.
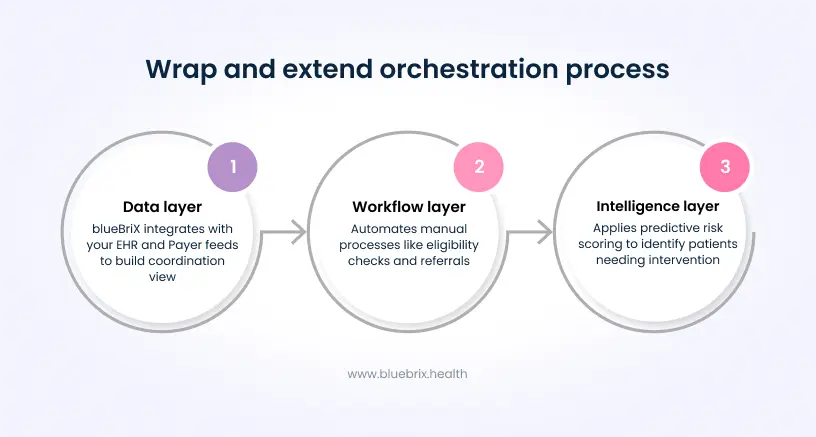
Step 1: The data layer (ingest & normalize)
We don’t ask you to move your data. We connect to it. blueBriX is integration-agnostic. We pull the necessary fields from your EHR and Payer feeds to build the coordination view. Your doctors keep using the EHR they know for prescribing and notes. Your coordinators use blueBriX for management.
Step 2: The workflow layer (automate)
We map your most expensive manual processes.
- Are you manually checking portals for eligibility? We automate that.
- Are you manually faxing referrals? We digitize that.
We target the Low Hanging Fruit of friction first to generate immediate ROI (hours saved).
Step 3: The intelligence layer (predict)
Once the data is flowing, blueBriX starts applying logic. We use predictive risk scoring to tell you not just who is sick, but who is likely to get sick next month. This allows you to deploy your expensive clinical resources (Nurses/MDs) only to the patients who need them, while using automated tools (SMS/Chatbots) for the lower-risk population.

