Care coordination is meant to simplify healthcare. Yet for many organizations, it’s become a maze of disconnected systems, manual workflows, and reactive decision-making. Providers struggle to keep up. Patients fall through the cracks. And despite investing millions in EHRs and digital tools, fragmentation persists. The truth is, coordination isn’t achieved by adding more technology. It’s achieved through orchestration. This guide is for healthcare leaders ready to eliminate chaos, unify teams, and move from reactive care to intelligent, proactive coordination at scale.
The imperative for care coordination
Healthcare organizations today face unprecedented complexity: multiple providers, fragmented data systems, patients with chronic or complex conditions, and growing expectations for outcomes-based care. The traditional approach where coordination is mostly manual, reactive, and siloed leads to:
- Poor patient outcomes: Missed follow-ups, gaps in preventive care, and avoidable complications.
- Inefficiency: Staff spend hours tracking referrals, chasing labs, or duplicating work already done elsewhere.
- Financial risk: Higher readmissions, missed shared savings opportunities, and penalties under value-based care models.
- Patient dissatisfaction: Confusion, repeated explanations, and fragmented communication reduce trust and engagement.
Without structured, proactive care coordination, healthcare organizations are left reacting to crises rather than preventing them.
Why coordination is central to value-based care
Value-based care (VBC) fundamentally shifts the focus from volume to outcomes. To succeed, organizations must demonstrate:
- Improved clinical outcomes (e.g., reduced HbA1c in diabetics, fewer hospital readmissions)
- Cost reduction and efficiency
- High patient satisfaction and engagement
Care coordination is the operational backbone that ties these metrics together. Without a centralized orchestration framework, even the best clinical teams cannot deliver consistent, measurable results.
The problem today: fragmentation and siloed systems
Most organizations use a patchwork of:
- EHRs with limited interoperability
- Separate referral tracking tools
- Population health or risk stratification platforms
- Manual care plans stored in spreadsheets or PDFs
The result? Care gaps, duplicated tasks, and lack of accountability. For example, a patient discharged from the hospital may have:
- A follow-up scheduled in one EHR
- Labs ordered in a different system
- Physical therapy referrals managed manually via fax or phone
This siloed approach creates the very fragmentation that allows critical patient steps to fall through the cracks, severely impacting both outcomes and reimbursement.
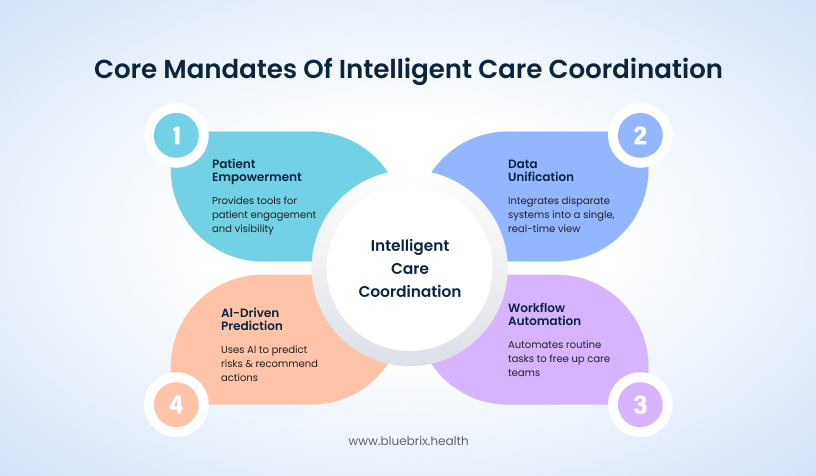
The solution: intelligent care coordination orchestration
If fragmentation is the problem, then orchestration is the answer. Intelligent care coordination platforms are designed to impose order on the chaos of disparate systems and complex patient journeys. They don’t just add another tool; they provide the central command structure that ensures every moving part works together perfectly. blueBriX addresses the main challenges in healthcare by executing four non-negotiable mandates:
Unifying data into a single truth: We tear down silos by integrating every disparate system such as EHRs, labs, monitoring devices to give coordinators a single, real-time, comprehensive view of the patient.
- Putting workflows on auto-pilot: We automate routine administrative tasks like referrals, reminders, and follow-ups. This frees your expert care teams from administrative drag so they can focus their time and compassion on complex patient needs.
- Making data predictive with AI: We leverage Artificial Intelligence to identify care gaps, predict patient risk before issues arise, and instantly recommend the next best action. This transforms your care model from reactive to proactive.
- Empowering the patient as a partner: We extend visibility and control directly to the patient. By providing real-time engagement tools and clear care plan visibility, we ensure patients and caregivers are active, informed participants in their own success.
The business case for care coordination investment
Investing in a care coordination program yields a tangible return. Data on coordinated care models for high-risk Medicare beneficiaries shows annual savings per enrollee ranging from $493 to over $5,300, with some programs demonstrating an ROI as high as 607% (The Commonwealth Fund).
For example, consider a Chronic Care Management (CCM) program focused on patients with congestive heart failure (CHF). A coordinated approach using remote monitoring, proactive check-ins, and streamlined primary care access can significantly reduce high-cost events like Emergency Department (ED) visits and hospital readmissions. Savings from targeted interventions addressing SDOH alone show meaningful impact:
- Supportive housing interventions: Studies on housing for complex patients have shown reductions in ED visits by 24% to 33% and hospital admissions by 15% to 42%.
- Case management programs: Comprehensive care management, such as the Pathways model, has resulted in a net benefit of approximately $89 to $422 per patient per month for high-risk, chronically ill populations, driven by reductions in utilization charges.
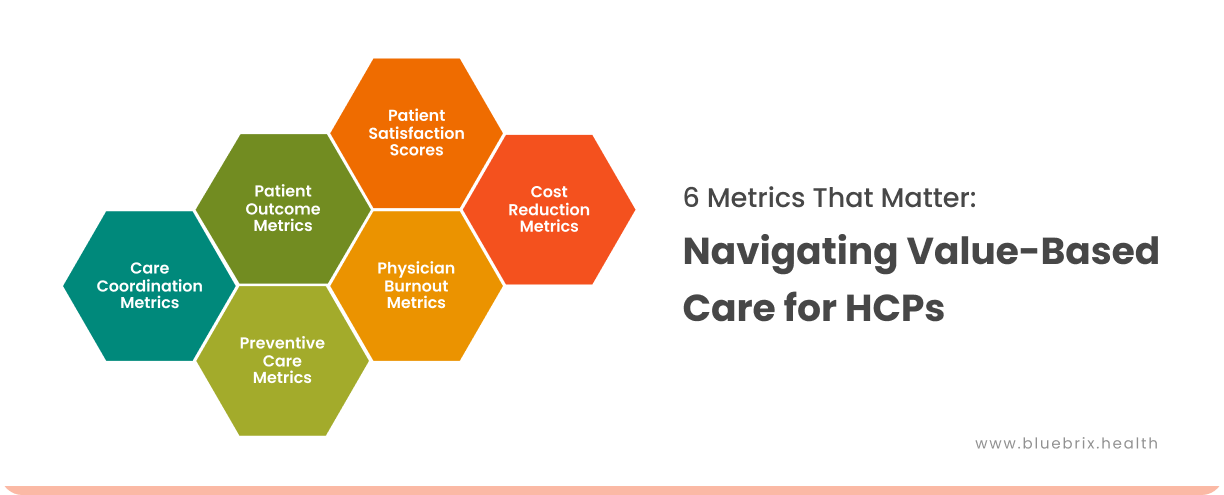
Key quality metrics and financial indicators
Successful coordination programs impact the most critical areas of healthcare performance.
So, what does truly intelligent care coordination translate to on your balance sheet and in your quality scores? It’s not just about happier teams; it’s about shifting the most critical financial and quality indicators in your favor.
Here’s how successful coordination programs directly impact the key areas of healthcare performance:
- Utilization control: A significant reduction in 30-day readmission rates comes with the avoidance of costly penalties and frees up operational capacity (beds, staff) for scheduled, profitable care.
- Quality & compliance: Tangible improvement in HEDIS/Star ratings scores unlocks major performance-based revenue and bonuses from payers (like Medicare Advantage) and secure better contracts.
- Patient experience: Consistently improved CAHPS scores (patient satisfaction) indicate engaged, satisfied patients which also mean higher patient retention, stronger market loyalty, and positive referrals which helps in long-term growth.
- Operational efficiency: Reduced length of stay (LOS) in acute and post-acute settings lead to a decreased overall cost of care per episode, proving your value and boosting margin.
Intelligent care coordination isn’t a cost center. It’s a revenue driver that optimizes utilization, maximizes quality incentives, and builds sustainable patient loyalty.
What Good Looks Like:
- A patient’s care plan is visible to the assigned care team in real-time
- Automated alerts flag overdue labs or missed appointments
- Coordinators spend time on intervention, not chasing data
- Performance dashboards track KPIs across the organization
Implementing intelligent orchestration transforms coordination from a reactive, labor-intensive process into a proactive, measurable, and patient-centered function which is the foundation for successful value-based care.
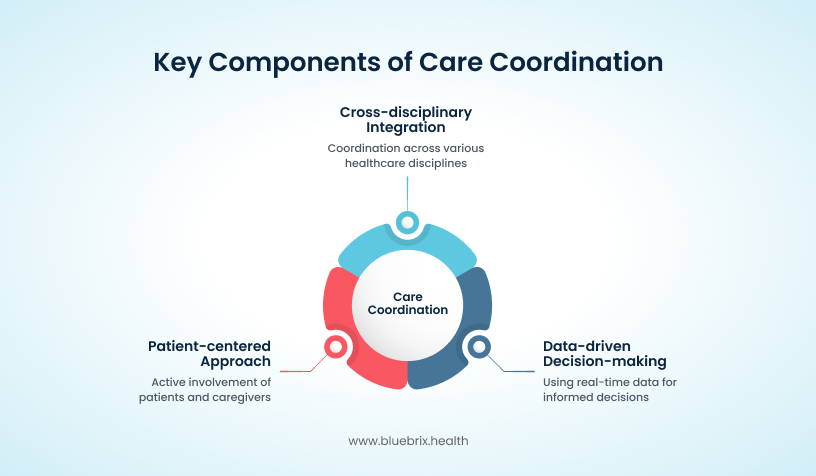
Defining care coordination in modern healthcare
Care coordination is often misunderstood as simply scheduling follow-ups or managing referrals. In reality, it is a structured, systematic process that ensures all aspects of a patient’s care are aligned, timely, and effective across multiple providers and care settings.
Core definition
Care coordination is:
“The deliberate organization of patient care activities and information sharing among all participants concerned with a patient’s care to ensure the right care is delivered at the right time, prevent duplication, and improve outcomes.”
Why care coordination matters
Without effective coordination:
- Patients experience confusion: Multiple providers, conflicting instructions, and missed communications.
- Clinicians spend time on non-value tasks: Repeating tests, tracking down missing information, and reconciling care plans.
- Organizations lose money: Unnecessary hospitalizations, missed preventive care, and poor adherence to value-based metrics.
Example:
A patient with congestive heart failure may see a cardiologist, primary care provider, nutritionist, and home health nurse. Without proper coordination:
- The patient may receive conflicting medication instructions
- Follow-up labs may be missed
- Care gaps increase the risk of avoidable ER visits
Core principles of modern care coordination
- Collaboration across disciplines
Effective coordination requires shared responsibility and seamless communication among physicians, nurses, social workers, pharmacists, and other allied health professionals. - Clear accountability
Every task, referral, and follow-up has an assigned owner. This prevents duplication and ensures tasks are not overlooked. - Patient-centered engagement
Engaging patients in their care plan improves adherence, reduces anxiety, and empowers self-management. Tools like mobile apps, text reminders, and educational resources enhance engagement. - Data integration & accessibility
Coordinators need a unified view of all clinical, social, and behavioral data. Fragmented records prevent proactive care and slow decision-making. - Continuous monitoring & adaptation
Patient needs change over time. Effective care coordination is dynamic, with real-time adjustments based on outcomes, risk stratification, and patient feedback.
How care coordination works across care models
ACO/Value-based care:
- Care plans shared across all providers, linked to outcome metrics.
- Real-time dashboards track performance at patient and population levels.
Behavioral health organizations:
- Coordination between mental health providers, primary care, and social services.
- Automated reminders and telehealth check-ins improve adherence.
Direct primary care (DPC):
- Patient engagement is central; coordinators track wellness, preventive care, and chronic conditions.
- Digital portals allow patients to view care plans and upcoming visits.
FQHC/Public health centers:
- Large patient populations with high social determinant needs require scalable coordination solutions.
- Integration with community resources ensures comprehensive care.
Global/International networks:
- Multi-location coordination requires interoperable platforms to connect providers across regions.
- Ensures continuity of care for patients who travel or relocate.
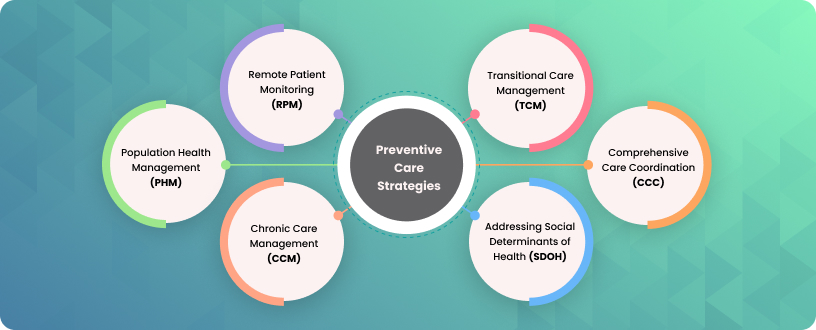
Different types of care coordination
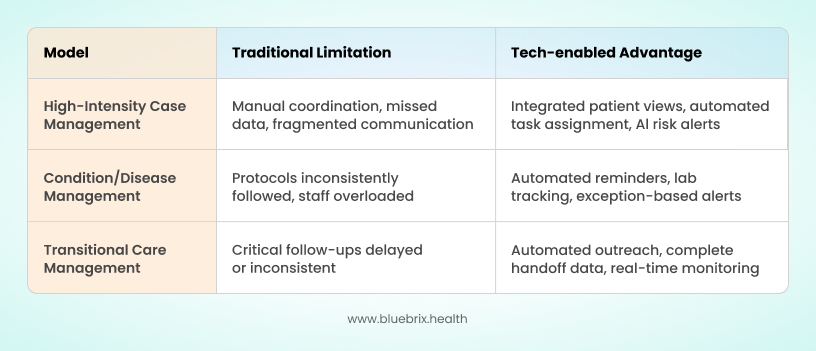
We all know that care coordination is not one-size-fits-all. Different patient populations (from high-risk, multi-morbidity patients to defined disease cohorts and recently discharged patients) require different approaches. What is evolving is how technology enables these models to be executed consistently, efficiently, and proactively, freeing clinical teams to operate at the top of their license.
Below, we explore the three core coordination models, illustrated with examples of how intelligent orchestration platforms enhance outcomes.
1. High-intensity case management
High-intensity case management is designed for patients with complex chronic conditions, behavioral health needs, and social vulnerabilities. Clinicians excel at managing these patients, but operational friction often slows progress: incomplete data, missed follow-ups, and fragmented communication.
Integrated assessment tools provide longitudinal patient views, automated task assignment ensures nothing falls through the cracks, and AI-driven risk alerts highlight patients needing immediate attention. Clinicians spend less time on logistics and more on meaningful intervention, allowing the highest ROI for intensive care management.
2. Condition / disease management
Disease or condition management programs target defined populations, such as diabetics or patients with heart failure. The challenge is to scale adherence to protocols consistently across large populations.
Orchestration platforms automate reminders, lab tracking, and patient engagement, while exception-based alerts allow teams to focus only on deviations or patients requiring intervention. This combination preserves standardization while delivering personalized attention at scale.
3. Transitional care management (TCM)
Transitional care programs focus on the critical post-discharge window, where readmission risk is highest. While clinical teams know the steps – reconciliation, follow-up, handoff – execution consistency has historically been difficult.
Platforms automate outreach, monitor responses, and consolidate complete handoff information. The result is a reliable, predictable transition process that reduces readmissions without adding administrative burden.
For executive leadership, the value is clear: intelligent orchestration transforms operational efficiency into measurable financial and clinical outcomes. By enabling high-touch teams to focus on complex cases, ensuring standardized care protocols are followed, and closing critical post-discharge gaps, organizations reduce avoidable hospitalizations, improve quality metrics, and increase patient engagement, all while maximizing return on existing clinical resources.
Common pitfalls in care coordination
Common pitfalls in care coordination can significantly impact patient outcomes and operational efficiency. Siloed EHRs often lead to missed updates and duplicated tests, which can be addressed by implementing a unified orchestration platform that consolidates patient data and provides real-time visibility to all providers. Manual referral processes increase the risk of lost or delayed appointments, but automated referral workflows can streamline tracking and ensure timely follow-ups. Poor patient engagement frequently results in non-adherence to care plans, a challenge that can be mitigated through digital engagement tools and patient education resources that empower individuals to actively participate in their care. A lack of accountability allows tasks to fall through the cracks, emphasizing the need for clearly assigned ownership and dashboards to monitor task completion. Finally, a reactive approach to care increases the likelihood of readmissions and complications, highlighting the importance of AI-powered proactive alerts that identify high-risk patients early and enable timely intervention. Together, these solutions form a strategic framework for improving care coordination and driving better patient outcomes.
Modern care coordination is more than process. It is the backbone of value-based care success.
Coordination impact snapshot
- Coordinated care reduces readmission rates by 20–30% in high-risk populations
- Improves adherence to care plans by up to 25%
- Enhances patient satisfaction scores by 15–20%
The 8-step care coordination framework
A successful coordination process must be structured, deliberate, and supported by a robust technological platform. The first step in any effective coordination model is assigning clear roles and accountability. Effective coordination relies on three foundational pillars:
- Assigning the coordinator: Accountability for coordinating activities must be explicitly assigned, often to a primary care provider, case manager, or advanced practice RN.
- The interdisciplinary care team (ICT): Coordination is a team sport. Utilizing an ICT structure allows different types of staff to share their expertise, knowledge, and skills to solve complex problems that cannot be managed by a single discipline alone.
- Empowering the patient and caregiver: Patients and their families must actively participate by communicating their healthcare priorities. If a patient cannot participate, an alternative caregiver must be identified, and permission must be documented for them to receive medical information.
A structured framework is essential for consistent, high-quality care coordination. The following 8-step model provides a repeatable approach for healthcare organizations of any size or specialization.
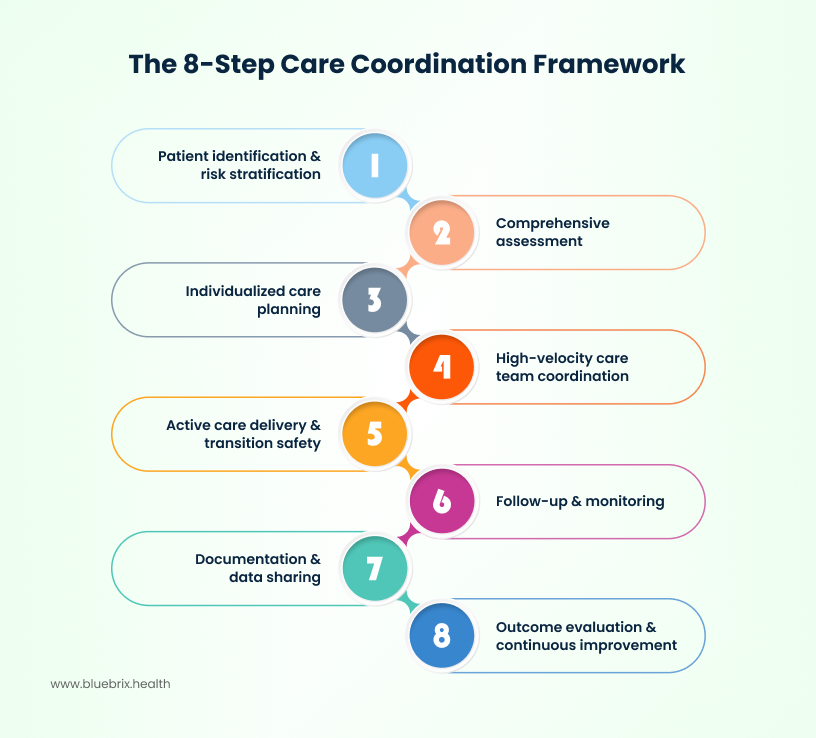
Step 1: Patient identification & risk stratification
The foundation of any successful care coordination strategy rests on who you decide to engage and why. It’s about moving beyond simply responding to high-utilization reports and actively predicting risk. This first step is where technology absolutely changes the game. We’re talking about transitioning from manual data extraction by stitching together claims, EHR files, and limited social data to leveraging true predictive intelligence. The goal is to move past broad categorization and instantly synthesize a refined, actionable patient segment. This ensures that expert coordinator time is strategically prioritized for maximum preventive impact, allowing the system to focus resources where they can preempt a crisis, not just manage the fallout.
Key actions:
- Move beyond clinical data: Seamlessly unify patient files with demographic and social data to create a true 360-degree profile, ensuring high-risk identification is comprehensive, not fragmented.
- Deploy predictive algorithms: Apply sophisticated AI and risk stratification models that automatically segment and score the patient population based on care complexity and anticipated needs.
- Optimize resource allocation: Use the platform’s intelligence to precisely prioritize patients for outreach, guaranteeing that coordination resources are deployed where they will deliver the greatest clinical and financial impact.
Example:
A diabetes patient with poorly controlled HbA1c and recent ER visits is flagged for intensive care coordination. Automated alerts notify the care team for timely intervention.
Proactive identification can reduce hospitalizations by up to 20% in high-risk populations.
Step 2: Comprehensive assessment
Identifying the right patient is only the beginning; now, the coordinator must move rapidly to a deep, holistic understanding of that patient’s actual needs. We know a clinical snapshot isn’t enough—success hinges on uncovering behavioral and social barriers.
This step is about leveraging technology to conduct a 360-degree assessment efficiently, ensuring your coordinators gather high-quality, actionable data without administrative burden:
Key actions:
- Holistic data synthesis: Use the platform to drive and document thorough clinical, behavioral, and social assessments in one unified view. The system should flag missing data points, guiding the coordinator toward a complete picture.
- Structured engagement capture: Embed tools that capture and document patient and caregiver preferences, cultural needs, and known barriers (e.g., transportation, health literacy), ensuring this crucial human element informs the subsequent plan.
- Assessment-to-action linkage: Ensure the assessment findings automatically populate and suggest relevant sections for the care plan in the next step, eliminating the manual transfer of insights into goals.
Step 3: Individualized care planning
Once the assessment is complete, the focus shifts to creating a dynamic, measurable blueprint for improvement. The plan must be more than a static document; it must be a living, breathing tool for accountability and collaboration.
This step utilizes the orchestration platform to translate deep assessment data into clear, measurable interventions, making the plan a joint effort between the coordinator and the patient:
Key actions:
- Measurable goal setting: Employ the platform to develop measurable goals and milestones—spanning medication adherence, lifestyle changes, and preventive care using smart templates derived directly from the assessment findings.
- Shared decision-making documentation: Integrate tools that facilitate and document patient and family engagement in goal co-creation, ensuring all goals are mutually agreed upon and thus, more likely to be met.
- Dynamic plan activation: Immediately trigger automated tasks and alerts based on the finalized plan. The platform ensures that the moment a goal is set (e.g., scheduling a follow-up lab), the corresponding action is assigned and tracked automatically.
Example:
A chronic obstructive pulmonary disease (COPD) patient’s care plan includes pulmonary rehab referrals, smoking cessation support, home oxygen monitoring, and telehealth check-ins.
Individualized care plans improve adherence and reduce avoidable acute care events.
Step 4: High-velocity care team coordination
The collective impact of your care team is only as strong as its weakest point of communication. After securing external referrals, the immediate priority is to ensure the internal, multidisciplinary team including PCPs, specialists, pharmacists, and behavioral health operates as a unified, high-velocity unit.
This step utilizes the orchestration platform to enforce consistent communication standards and clear accountability:
Key actions:
- Instantaneous team formation: Automatically map and identify all required providers based on the patient’s care plan. The platform should instantly assemble the virtual care team and grant them access to the unified patient record, eliminating manual list creation.
- Shared, dynamic task management: Replace fragmented emails and paper notes with collaborative task lists and shared calendars built directly into the care plan. The system dynamically assigns and tracks responsibilities, ensuring everyone knows their immediate priority and status.
- Systematized communication flows: Establish and enforce digital touchpoints from secure, asynchronous messaging to scheduling virtual huddles, ensuring critical information flows immediately to the right person, bypassing internal communication silos.
- Automated escalation protocols: Hardwire care escalation protocols directly into the workflow. The system should automatically elevate urgent issues (e.g., missed vital checks, non-compliance alerts) to the appropriate team member, ensuring immediate and consistent intervention.
Step 5: Active care delivery & transition safety
This is the high-stakes phase where the plan is executed and the patient moves through different settings. The platform must ensure seamless treatment delivery and, most critically, prevent the patient from falling into the “transition chasm” when they leave a facility. This is where automation equals patient safety.
Key actions:
- Integrated treatment execution: The platform serves as the central hub for care delivery, coordinating and documenting all prescribed actions starting from clinical visits and home health coordination to automated virtual check-ins ensuring fidelity to the care plan.
- Proactive transition triggers: Automate the start of discharge planning immediately upon admission or initiation of care. The system should embed transition templates and alerts, ensuring this critical process is never left until the last minute.
- Mandated information handoffs: Use digital protocols to enforce the immediate, secure transfer of essential information including the discharge summary, updated medication lists, and care instructions to the next provider, eliminating the risk of paper-based errors.
- Automated follow-ups: Hardwire post-discharge care by automatically tracking and confirming follow-up appointments within the crucial 48–72 hour window. The platform must alert the care team if these critical milestones are missed, actively preventing readmissions.
Example:
When a high-risk patient is discharged, the platform instantly triggers the follow-up process, automatically scheduling and tracking the critical 48-hour appointment and pushing updated medication changes to the next provider. This automated enforcement eliminates the dangerous transition gap, actively preventing readmissions before they even begin.
Step 6: Follow-up & monitoring
Care coordination is not a one-time transaction; it’s a continuous loop of vigilance. After executing the plan, the next most strategic step is to continuously monitor the patient’s status to catch potential declines or non-adherence before they result in a negative event. This is where the platform shifts from coordination to true, real-time risk management.
Key actions:
Risk-stratified check-in scheduling: Automate scheduling regular check-ins based on the patient’s current risk level and the complexity of their care plan. The system dictates the frequency, ensuring high-risk patients receive intense support and lower-risk patients get efficient, timely maintenance.
Adherence tracking without paperwork: Seamlessly monitor adherence to medications, therapy, and lifestyle interventions by integrating patient-reported data, pharmacy refills, and remote monitoring device metrics. The platform flags deviations immediately, bypassing the need for manual chart reviews.
Predictive deterioration detection: Apply AI and advanced analytics to the incoming stream of data (from all integrated sources). The platform actively searches for early signs of deterioration or critical gaps in care, providing the care team with a warning signal instead of a diagnosis.
Example:
A high-risk cardiac patient’s vitals are monitored remotely. Alerts are generated if blood pressure or heart rate exceeds thresholds, prompting immediate intervention.
Step 7: Documentation & data sharing
The entire intelligent coordination cycle from risk identification to continuous monitoring, is validated and sustained by accurate, secure documentation. This step transforms documentation from a compliance chore into a strategic advantage, ensuring every intervention is recorded, auditable, and accessible across the continuum.
Key actions:
- Unified record of truth: Ensure that the documentation of all assessments, interventions, and communications is accessible as a centralized single source of truth. This eliminates scattered records and guarantees every team member is working from the complete, accurate patient story.
- Secure, authorized information flow: Leverage the platform’s architecture to securely share clinical records instantly with authorized providers, payers, and the patient. This ensures seamless continuity of care without relying on manual faxes or portals.
- Automated compliance assurance: Hardwire regulatory standards (like HIPAA) directly into the platform’s processes. The system actively manages access controls and audit trails, making compliance a default state rather than a manual checklist item.
Centralized documentation drastically reduces documentation errors, prevents redundant work, and provides the necessary auditable data needed to accurately report and thrive under value-based contracts.
Step 8: Outcome evaluation & continuous improvement
The final, essential step is to close the loop: rigorously measure the impact of coordination and turn those insights into continuous process improvement. Coordination is a living system, not a static process, and this step guarantees perpetual refinement and maximum ROI.
Key actions:
- Track KPIs: Automatically track and visualize key performance indicators directly within the platform. This includes not just outcomes (like readmissions or cost savings) but also process metrics like referral closure rates and care plan adherence, providing immediate operational visibility.
- Data-driven bottleneck identification: Use the platform’s aggregated data to conduct periodic, objective performance reviews. The technology pinpoints specific workflow bottlenecks or areas of inefficiency (e.g., delays by a particular provider or in a specific geographical area) without manual data extraction.
- AI-informed optimization: Leverage AI recommendations to guide process adjustments. The system suggests and documents workflow modifications, facilitates the integration of new tools, and allows for rapid A/B testing of new strategies to ensure outcomes are continuously enhanced.
Example:
The coordination dashboard alerts leaders to consistent delays in completing oncology referrals, specifically for new patients. Data-driven process adjustments are instantly applied such as automatically notifying the coordinator 24 hours prior to the due date and the system tracks and verifies an immediate, measurable improvement in completion rates across the next quarter.
The multidisciplinary care team (MDT)
Caring for patients effectively isn’t a solo act; it’s a precisely choreographed performance by the Multidisciplinary Care Team (MDT). This diverse group acts as the patient’s comprehensive support system, ensuring seamless care orchestration. The Physician provides the critical clinical oversight and ultimate treatment accountability, while the Nurse Care Coordinator serves as the vital day-to-day conductor, managing medication and high-risk monitoring. Meanwhile, the Social Worker addresses the crucial social determinants of health and resource needs, the Pharmacist fine-tunes the medication regimen for safety and cost, and the Therapists (Physical/Occupational) focus on restoring function and assessing the home environment. Together, these experts transform a fragmented system into a unified, holistic, and patient-centered experience.
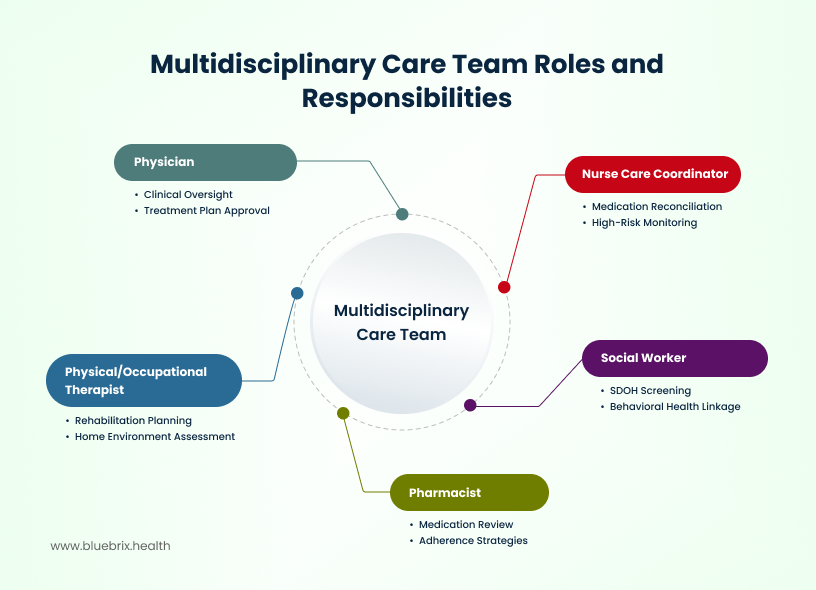
Building the team: protocols, roles, and partnerships
Intelligent care coordination relies on technology, but it’s executed by people and partners. This section outlines the essential standards and structures needed to make your team function as a unified whole, inside and outside the clinic walls.
Eliminating communication failures with handoff standards
The most vulnerable moment in a patient’s journey is often the handoff. When moving from the hospital to home, from primary care to a specialist, or between shifts. This process has to be standardized. Adopt a consistent, proven framework like SBAR (Situation, Background, Assessment, Recommendation) for all transitions. This ensures every piece of critical information is transferred efficiently, consistently, and without ambiguity, drastically reducing the risk of a communication error.
Defining roles and accountability
Gaps in care happen when a task is left undone because everyone thought it was someone else’s job. Duplication occurs when two people do the same work. Every team member’s role and specific responsibilities must be clearly documented and visible within the technology platform. The platform must automatically assign tasks based on defined roles and required skill sets. This eliminates guesswork and ensures tasks are routed to the person best equipped to handle them.
Integrating community partners (CBOs)
True care coordination extends well beyond the exam room. A patient’s outcome is often determined by social factors such as housing, food security, and transportation. The platform must seamlessly integrate Community-Based Organizations (CBOs). If a patient needs food assistance or transportation, the referral is made through the platform, and the outcome (Did the patient receive the service?) is tracked and documented back to the clinical record. This is vital for addressing the social determinants of health (SDOH).
Closed-Loop Referral Management
The external referral is often called the Achilles’ heel of care coordination, the point where accountability vanishes, leading to care delays and administrative chaos. Simply sending a request is not management; it’s merely a hope. Ideally, external referrals should be in a secure, closed-loop system. You need a technology that makes tracks the entire process when you hand off a patient to a specialist or an ancillary provider. This involves real-time tracking of requests and confirmations to eliminate the referral “black hole,” along with using network data to coordinate appointments and actively avoid delays. It’s about maintaining constant visibility and accountability for every patient, even when they step outside your immediate network.
Patient Self-Management and Shared Decision-Making
The patient isn’t just a recipient of care. They are the most important, high-touch member of the care team. Their adherence is the ultimate measure of success. Coordination workflows must prioritize patient education and motivational interviewing to help them adhere to their care plan. All clinical goals and interventions must be co-created with the patient through genuine shared decision-making. When patients help set the goal, they are far more likely to own the outcome.
8-Step framework benefits
- Reduces care gaps and avoidable hospitalizations
- Improves adherence to preventive care and chronic condition management
- Enhances communication across interdisciplinary teams
- Supports real-time, data-driven decision-making
- Aligns care activities with value-based care incentives
KPIs and performance measurement in care coordination
To truly optimize care coordination, organizations must measure performance consistently. Key performance indicators (KPIs) provide actionable insights into workflow efficiency, patient outcomes, and financial performance. Without KPIs, care coordination remains anecdotal and reactive.
Why KPIs matter
- Visibility: KPIs highlight where care gaps exist, which patients are at risk, and which processes are inefficient.
- Accountability: Assigning measurable metrics ensures care coordinators and teams are responsible for outcomes.
- Continuous Improvement: By tracking KPIs over time, organizations can refine workflows and reduce costs.
- Value-Based Care Alignment: Many VBC contracts tie reimbursement to measurable outcomes; KPIs provide evidence of performance.
Measuring KPIs is the foundation for scaling effective care coordination. You can’t improve what you don’t measure.
Core KPI categories
1.Referral efficiency – Tracks how quickly and completely referrals are processed and closed.
Key metrics:
- % of closed-loop referrals
- Average referral completion time
- Referral follow-up adherence rate
Strategic impact: Faster, complete referrals improve patient experience and reduce delays in care.
2.Care plan adherence – Measures the degree to which patients follow prescribed treatment and care plans.
Key metrics:
- Patient engagement rate
- Medication adherence
- Follow-up visit compliance
Strategic impact: High adherence directly correlates with improved clinical outcomes.
3.Clinical outcomes – Evaluates patient health improvements and reduction in adverse events.
Key metrics:
- Readmission rates
- ER visits per 1,000 patients
- Chronic disease control metrics (HbA1c, BP, cholesterol)
Strategic impact: Demonstrates care effectiveness and justifies resource allocation.
4.Patient experience & satisfaction – Captures patient perceptions and engagement quality.
Key metrics:
- Net Promoter Score (NPS)
- Patient satisfaction surveys
- Caregiver-reported burden reduction
Strategic impact: Higher satisfaction correlates with better adherence and lower churn.
5.Operational efficiency – Measures the efficiency of care coordination processes.
Key metrics:
- Average time per case
- % of tasks automated
- Staff workload balance
Strategic impact: Frees up care coordinators for higher-value tasks and reduces burnout.
6.Financial impact – Evaluates cost savings and revenue generation from coordinated care.
Key metrics:
- Per-member per-month (PMPM) savings
- Avoided high-cost utilization
- Shared savings performance under VBC models
Strategic impact: Demonstrates ROI of care coordination initiatives.
Using KPIs to drive continuous improvement
Step 1: Set baseline measurements across all KPI categories.
Step 2: Implement intelligent orchestration tools to track real-time data.
Step 3: Conduct weekly or monthly reviews to identify bottlenecks or deviations.
Step 4: Adjust workflows, automate repetitive tasks, and provide staff training based on insights.
Step 5: Benchmark against similar organizations to identify opportunities for innovation.
By combining KPIs with intelligent orchestration platforms like blueBriX, organizations can:
- Improve patient outcomes without increasing staff workload
- Reduce avoidable hospitalizations and ER visits
- Demonstrate measurable success for VBC contracts
- Increase patient satisfaction and engagement through proactive care
KPIs are not just metrics. They are the roadmap to high-performing, accountable, and sustainable care coordination.
KPI integration with AI & automation
- AI flags care gaps before they affect outcomes
- Automation ensures timely follow-ups and documentation
- Real-time dashboards allow leaders to monitor and act instantly
By combining KPIs with intelligent orchestration platforms like blueBriX, organizations can:
- Improve patient outcomes without increasing staff workload
- Reduce avoidable hospitalizations and ER visits
- Demonstrate measurable success for VBC contracts
- Increase patient satisfaction and engagement through proactive care
KPIs are not just metrics. They are the roadmap to high-performing, accountable, and sustainable care coordination.
Care coordination use cases across care settings
Care coordination is not one-size-fits-all. Different healthcare organizations face unique challenges, patient populations, and operational complexities. Intelligent orchestration platforms like blueBriX can be tailored to meet the specific needs of each setting, while maintaining a unified, measurable approach.
1. Accountable care organizations (ACOs) & value-based care
For ACOs and value-based care networks, coordinating care isn’t just a workflow challenge, it’s the difference between earning shared savings or absorbing penalties. These organizations are tasked with managing population health across a web of hospitals, specialists, primary care providers, and post-acute facilities. Keeping everyone aligned, while ensuring patients follow through on care plans, is no small feat. Add the pressure of meeting CMS quality metrics and preventing costly readmissions, and it becomes clear why so many ACOs struggle to scale impact consistently.
This is where intelligent care coordination becomes a game changer. Instead of relying on siloed EHRs and manual follow-ups, a unified orchestration layer pulls patient data from every participating provider into one command center. AI flags rising-risk patients before they spiral, automatically triggering alerts for missed screenings, unmanaged chronic conditions, or lapses in care. Coordinators are assigned tasks in real time, and every referral, appointment, and outcome can be tracked without chasing faxes or phone calls.
Consider an ACO managing over 50,000 attributed lives. By implementing AI-powered risk stratification and automated task routing, high-risk patients were proactively identified and assigned to care managers without delay. Preventive screenings were automatically scheduled. Specialists received digital referrals instead of paper trails. Leadership could finally see how they were performing against shared savings goals and quality benchmarks, all in one dashboard. The result? Within just 12 months, readmissions fell by 22%, and shared savings increased by 15%.
This isn’t just operational efficiency but proof that orchestrated care coordination turns value-based care from aspiration into reality.
2. Multi-specialty clinics & large hospitals
For multi-specialty clinics and large hospital systems, care coordination can feel like managing a symphony with too many instruments playing independently. Referrals between departments often get delayed, critical information may not flow seamlessly between primary care and specialists, and operational inefficiencies can frustrate both staff and patients. Every missed handoff or delayed follow-up risks compromising patient outcomes and satisfaction.
Intelligent care coordination changes this dynamic entirely. By orchestrating both internal and external referrals, it ensures that every patient moves through their care journey smoothly, with no gaps or lost communication. Unified dashboards give care teams a clear view of patient status, task ownership, and upcoming interventions, while automation handles routine reminders and follow-ups. This frees coordinators to focus on high-risk patients rather than administrative paperwork, making their efforts more impactful.
Take the example of a large multi-specialty hospital. By implementing an automated referral workflow, the organization reduced referral completion times from 10 days to just 3 days. Coordinators could redirect their attention to complex cases, ensuring timely interventions for those who needed it most. The outcome? Not only did operational efficiency improve, but patient satisfaction scores also climbed by 18%, demonstrating that smoother coordination translates directly into a better patient experience.
In essence, for hospitals juggling multiple departments and specialties, orchestrated care coordination is a strategic advantage that improves both outcomes and satisfaction.
3. Chronic care management programs
Managing patients with chronic conditions is one of the most complex and high-stakes areas of healthcare. Coordinators must monitor multiple care touchpoints, ensure adherence to medications and lifestyle interventions, and prevent avoidable acute events all while keeping patients engaged and supported. Without a cohesive system, it’s easy for critical warning signs to slip through the cracks, resulting in hospitalizations and compromised outcomes.
Intelligent care coordination transforms chronic care from reactive to proactive. Personalized care plans guide each patient’s journey, supported by automated reminders for medications, appointments, and lifestyle goals. Remote monitoring devices feed real-time data into the system, while AI-driven alerts flag deviations or concerning trends, prompting early interventions. Integration with telehealth platforms ensures that coordinators, clinicians, and patients remain connected, even outside the clinic walls.
Consider a diabetes management program as an example. Remote glucose monitoring devices send real-time readings directly to the platform, and coordinators are automatically alerted when values fall outside safe ranges. Digital care plans provide patients with clear guidance and reminders, while telehealth check-ins enable timely adjustments to treatment. Within a year, hospital admissions dropped by 25%, and patient-reported adherence improved by 30%.
By bringing together technology, data, and human oversight, chronic care management programs can shift from fragmented, reactive care to continuous, connected, and patient-centered management, ultimately improving both clinical outcomes and quality of life for patients.
4. Behavioral health organizations
Behavioral health care presents unique challenges that extend beyond medical treatment. Coordinating therapy, medications, and social services while integrating with primary care can feel overwhelming. Tracking patient progress across multiple providers is often fragmented, making it difficult to identify early warning signs or lapses in care. For patients, these gaps can mean missed sessions, inconsistent treatment, and reduced engagement, all of which can impact outcomes and quality of life.
Intelligent care coordination addresses these challenges by creating a seamless, connected system for behavioral health. Coordinators can track each patient’s progress across therapy sessions, medication adherence, and follow-ups, ensuring that no step is missed. Scheduling, reminders, and patient communications are automated, reducing administrative burden and improving efficiency. Secure communication channels allow providers, patients, and caregivers to stay aligned, fostering collaboration and trust throughout the care journey.
Take the example of a community behavioral health center. By integrating its EHR and telehealth platforms with blueBriX, the center receives automated alerts whenever a patient misses a therapy session. Coordinators can reach out proactively, addressing potential gaps before they escalate into crises. The result is tangible: patient engagement rises by 20%, and no-show rates drop by 15%, demonstrating that coordinated, proactive care not only improves operational efficiency but also enhances the patient experience.
Ultimately, for behavioral health organizations, intelligent orchestration transforms fragmented care into a proactive, patient-centered system, ensuring that every individual receives the attention, support, and continuity they need.
5. Federally qualified health centers (FQHCs) & public health organizations
FQHCs and public health organizations often operate in complex environments, serving large populations with diverse medical and social needs. High patient-to-coordinator ratios, limited staffing, and the necessity to address social determinants of health make delivering consistent, high-quality care a daunting task. Without scalable systems, care gaps can widen, and high-risk patients may not receive the attention they need in time.
Intelligent care coordination offers a practical solution to these challenges. By leveraging AI-powered risk stratification, organizations can identify and prioritize high-risk patients, ensuring that limited resources are focused where they matter most. Routine administrative tasks, referrals, and follow-ups can be automated, freeing coordinators to handle complex cases rather than repetitive processes. Integration with community resources, social services, and telehealth platforms allows care to extend beyond the clinic walls, addressing both medical and social factors that influence outcomes.
For instance, an FQHC serving 20,000 patients implemented an automated referral and follow-up system targeting high-risk populations. Coordinators could focus on complex cases, while automation managed standard follow-ups and alerts. The results were striking: readmissions dropped by 18%, and patient satisfaction improved by 15%. This demonstrates how technology-driven orchestration enables FQHCs and public health organizations to deliver holistic, proactive care at scale, even with resource constraints.
Ultimately, for organizations serving large, vulnerable populations, intelligent care coordination is a strategic enabler that ensures every patient receives timely, equitable, and effective care.
6. Direct primary care (DPC) practices
Direct Primary Care practices pride themselves on offering highly personalized care while maintaining low overhead, but the very model that allows for closer patient relationships can also create operational challenges. Small care teams must engage patients proactively in preventive and chronic care, track outcomes accurately, and ensure continuity without the extensive administrative support available in larger systems. Balancing these demands requires smart, scalable approaches to care coordination.
Intelligent care coordination platforms help DPC practices meet these challenges head-on. Digital engagement portals give patients clear visibility into their care plans, upcoming appointments, and lab results, empowering them to take an active role in their health. Automated reminders for preventive screenings, medication adherence, and follow-ups reduce missed opportunities, while analytics tools allow clinicians to track clinical outcomes and patient engagement efficiently.
Consider a DPC practice leveraging blueBriX to manage patient engagement and coordination. Automated health reminders are sent directly to patients, lab results are monitored in real time, and referrals to specialists are coordinated seamlessly. Within months, patient engagement increased by 25%, and adherence to preventive care improved by 30%. These results demonstrate that even small care teams can deliver highly personalized, measurable, and proactive care, translating directly into healthier patients and a stronger, more efficient practice.
For DPC practices, intelligent care coordination transforms the challenge of limited resources into an opportunity to provide exceptional, patient-centered care at scale, creating measurable value for both patients and providers.
7. Global healthcare networks
For multinational healthcare networks, care coordination comes with a unique set of challenges. Providers must manage patient care across multiple countries or regions, integrating diverse health records and telehealth platforms while adhering to varying regulatory requirements. Without a cohesive system, patients, especially those who travel or live abroad, can experience gaps in care, inconsistent treatment plans, and delays in follow-ups. Maintaining quality and compliance across borders requires both sophistication and flexibility.
Intelligent care coordination platforms enable global healthcare networks to overcome these complexities. A centralized orchestration system can integrate multi-language and multi-region data, allowing care teams across continents to access consistent patient information in real time. Dashboards provide a holistic view of care delivery, tracking progress, outcomes, and engagement for patients wherever they are. At the same time, compliance features ensure adherence to HIPAA, GDPR, and other international privacy and security regulations, giving providers peace of mind while delivering seamless care.
Consider a multinational network managing chronic disease programs for expatriates. AI flags patients missing follow-ups, ensuring timely intervention. Telehealth sessions are automatically scheduled regardless of time zones, and care plans remain consistent across regions. The outcome is a tangible reduction in hospitalizations and sustained high patient satisfaction, demonstrating that geographic complexity doesn’t have to compromise quality.
For global healthcare networks, intelligent care coordination transforms fragmented, cross-border operations into a seamless, efficient, and compliant system, ensuring patients receive continuous, high-quality care no matter where they are in the world.
From small DPC clinics to global networks, care coordination becomes proactive, measurable, and intelligent when powered by orchestration platforms.
No matter the care setting, intelligent orchestration platforms like blueBriX:
- Align workflows across providers, departments, and locations
- Reduce manual effort and administrative overhead
- Enable data-driven decision-making at scale
- Improve patient outcomes, engagement, and satisfaction
The future of care coordination
Healthcare is rapidly evolving, and care coordination is no exception. Traditional reactive models are giving way to proactive, AI-driven, and patient-centered orchestration, allowing organizations to manage complex care networks efficiently and improve outcomes.
AI-powered predictive workflows
Objective: Leverage artificial intelligence to anticipate patient needs, identify risks, and recommend interventions before issues escalate.
Key applications:
- Risk prediction: AI analyzes clinical, behavioral, and social data to identify patients at risk of hospitalization, readmission, or care gaps.
- Next-best-action recommendations: Suggest interventions such as medication adjustments, referrals, or lab monitoring.
- Resource optimization: Assign care coordinators where they can have the most impact, based on patient complexity and risk.
Example:
A chronic kidney disease patient flagged by predictive analytics for declining eGFR receives an early nephrology referral, avoiding emergency hospitalization.
Organizations using AI in care coordination can reduce high-risk patient admissions by up to 25%.
Workflow automation
Objective: Reduce manual tasks and free care coordinators to focus on interventions that require human expertise.
Key applications:
- Automated reminders for appointments, medications, and preventive care
- Automated referral tracking and completion alerts
- Digital documentation and compliance reporting
- Notifications for care plan deviations
Automation does not replace coordinators. It augments their effectiveness, ensuring high-risk patients never fall through the cracks.
Virtual and patient-led coordination
Objective: Empower patients to participate in and manage their care through digital platforms.
Key applications:
- Patient portals and mobile apps for viewing care plans, lab results, and medications
- Interactive questionnaires and symptom trackers for real-time reporting
- Telehealth check-ins to reduce travel burden and improve engagement
Example:
When a post-surgical patient uses a mobile app to report wound healing progress, the care team receives automated alerts if complications arise, enabling timely intervention without in-person visits.
Impact: Patients who are engaged digitally show:
- 20–30% higher adherence to care plans
- Reduced unnecessary clinic visits
- Increased satisfaction and trust in the care team
Interoperability across networks
Objective: Seamlessly integrate data and workflows across multiple care sites, payers, and third-party solutions.
Key applications:
- Integration with EHRs, billing systems, telehealth platforms, and social service networks
- Shared dashboards for care teams across locations
- Secure data exchange while maintaining HIPAA/GDPR compliance
Example:
An ACO with multiple clinics can use orchestration software to unify patient records across all facilities, enabling consistent care planning and performance tracking.
Interoperability is critical for reducing duplication, improving outcomes, and supporting value-based care contracts.
Global and cross-border coordination
Objective: Extend care coordination to international or multi-region patient populations.
Key applications:
- Coordination for patients who travel or live abroad
- Integration with international health records and telehealth services
- Multilingual support and culturally tailored care plans
Example:
An expatriate patient with chronic diabetes receives coordinated care from a global network, ensuring continuity of treatment across countries.
Impact: Expands reach for organizations, supports international patient engagement, and reduces care gaps in mobile populations.
Role of intelligent orchestration platforms
Platforms like blueBriX are central to the future of care coordination. They combine:
- AI and predictive analytics for proactive interventions
- Automation to streamline workflows and reduce human error
- Patient engagement tools for virtual and self-managed care
- Third-party integrations for interoperability across any network or care model
Future-ready care coordination moves from reactive task management to intelligent orchestration enabling measurable outcomes, operational efficiency, and patient satisfaction at scale.
Key takeaways for future-ready care coordination
- Proactive care saves lives and reduces costs: Early intervention reduces hospitalizations and complications.
- Automation enhances efficiency: Coordinators focus on value-added tasks rather than chasing paperwork.
- Patients are active participants: Digital engagement tools increase adherence and satisfaction.
- Data-driven orchestration is essential: Real-time insights and AI recommendations improve decision-making.
- Global reach is possible: Seamless coordination across borders supports expanding care models.
How blueBriX powers intelligent care coordination
The way we manage patient care is evolving fast. It can’t just be about checking boxes anymore; it has to be smart, integrated, and predictive. The future of healthcare demands a platform that can handle complex workflows, unify scattered systems, put AI to work, and keep patients actively engaged. blueBriX is that platform. It’s designed to stop the gaps, streamline the chaos, and give your teams the power to coordinate care efficiently and drive dramatically better patient outcomes.
1. Native and third-party integration
If your care teams are logging into five different systems, flipping between screens, and praying the data they’re looking at is the latest version, you have fragmented care. Silos aren’t just an inconvenience; they are a risk. Our primary goal is to make sure every system involved in a patient’s journey is talking to every other system, all the time.
How blueBriX makes it work:
- EHR unification: Stop the swivel-chair effect. blueBriX connects multiple Electronic Health Records (EHRs), even different ones across a health system, to give you one single source of truth for every patient.
- 3rd party tools: We seamlessly bring in data from essential third-party tools like telehealth platforms, remote monitoring devices, lab systems, and advanced analytics tools. You get the whole picture, not just the pieces your EHR manages.
- APIs and interoperability standards: We rely on robust industry standards like HL7 and FHIR. This isn’t just about compliance; it’s about ensuring data flows are secure, accurate, and ready to scale with you.
Real-world impact:
Imagine a patient recovering at home after a heart procedure. Their care coordinator needs to see the lab results from the hospital’s system, the vitals coming from their home monitoring device, and the notes from their recent telehealth check-in. Before blueBriX, that meant three logins and a lot of cross-referencing. Now, all that information flows into one unified view in real-time. The coordinator acts faster, errors are virtually eliminated, and the patient gets proactive, timely care.
The foundation of trust: absolute data governance
Unifying disparate patient data is only valuable if it is governed securely. Beyond simple compliance, the platform must guarantee absolute data integrity and security as a strategic baseline. This includes granular, built-in access controls, automatic audit trails, and adherence to global standards (like HIPAA and FHIR), ensuring that a single source of truth is also a single source of compliance and trust.
Integration eliminates silos, ensuring that care teams act on the most accurate and up-to-date information.
2. AI-driven decision support
Care coordination is too often reactive. A patient has a problem, and the team scrambles to fix it. But what if you could see problems coming before they happen? blueBriX transforms the sheer volume of patient data from an overwhelming burden into your greatest asset by embedding Artificial Intelligence directly into the workflow. The goal is simple: turn data into actionable insights that anticipate needs and guide perfect interventions.
How blueBriX amplifies your team:
- Predictive risk stratification: Our system constantly analyzes the unified patient data to flag high-risk individuals. We don’t just identify patients with chronic conditions; we pinpoint the ones whose condition is actively deteriorating, allowing you to intervene before a preventable issue becomes an expensive, emergency hospitalization.
- Next-best-action recommendations: The AI doesn’t just show you a risk score—it tells you what to do about it. Care coordinators receive automated, evidence-based suggestions for the next ideal step: a specific referral, a medication adherence check, or a preventive diagnostic test. It’s like having a clinical expert guiding every decision.
- Pattern recognition for prevention: Beyond individual patients, the platform detects subtle trends and patterns across populations. This intelligence helps you understand why complications occur, allowing you to adjust clinical protocols and prevent similar issues for hundreds of other patients.
Real-world impact:
Consider a patient managing diabetes. Their AI-powered dashboard suddenly flashes an alert, flagging a subtle but concerning pattern of declining blood sugar control based on their remote monitoring device and recent lab results. blueBriX doesn’t wait; it prompts the care coordinator to immediately schedule a telehealth visit to discuss medication adherence and dietary habits. This proactive, five-minute intervention prevents an emergency room visit or potential hospitalization, saving time, money, and sparing the patient from a severe health event.
blueBriX’s AI is the ultimate force multiplier. It doesn’t replace human intuition or clinical expertise; it amplifies it, enabling your organization to shift from reactive to truly proactive care.
3. Workflow automation
Care coordination teams are constantly drowning in paperwork, phone calls, and repetitive tasks. This administrative overload doesn’t just burn out staff. It creates dangerous delays and inconsistency in patient care. The goal of blueBriX’s automation isn’t to replace your team; it’s to liberate them from the monotony so they can focus their expertise where it truly matters: complex, high-touch patient support.
How blueBriX eliminates friction:
- Routine tasks on auto-pilot: We take the burden of repetitive, predictable work off your team’s plate. This includes automated referral tracking, sending timely appointment reminders, and scheduling routine follow-up messages directly to patients. Everything that can be consistent and fast, is.
- Built-in accountability: Care gaps often happen when a task falls through the cracks. blueBriX uses smart task assignment that automatically routes work to the right person. If a critical task isn’t completed on time, our escalation workflows immediately notify a supervisor, ensuring no patient is ever forgotten.
- Compliance without the headache: Staying compliant and documenting everything takes up valuable time. Our system automates routine compliance reporting and documentation, generating the required records as care progresses. This means your team is always audit-ready without spending hours on retrospective charting.
Real-world impact:
Imagine a large, multi-specialty clinic. Referrals are a constant source of frustration and delay. By implementing blueBriX, the entire process is automated: a primary care provider enters the referral, and the system automatically tracks its acceptance, sends the patient reminders, and confirms the specialist appointment. The result? The clinic sees referral completion time drop by 50%, patients are happier because nothing slips through the net, and coordinators can dedicate their newfound time to managing only the most challenging, complex cases.
The hidden ROI: retaining your expert talent
Intelligent orchestration offers a vital, unquantifiable return: staff retention. By eliminating the administrative swamp which often includes the redundant documentation, chasing of referrals, and manual follow-ups, technology frees your high-value coordinators to practice at the top of their license. The platform serves as a powerful tool to prevent burnout, ensuring your most experienced team members focus their compassion and expertise on complex care, not on frustrating paperwork.
Automation ensures that every step of the care process is executed consistently and on time, drastically reducing human error and allowing your care teams to practice at the very top of their license.
4. Real-time dashboards and reporting
If you’re making critical business and clinical decisions based on data that’s weeks or months old, you’re driving by looking in the rearview mirror. Intelligent care coordination requires live visibility into patient status, team performance, and financial metrics. blueBriX ensures that every stakeholder from the frontline coordinator to the CEO, is working from a single, up-to-the-minute truth.
How blueBriX delivers clarity:
- Custom dashboards: We provide purpose-built, live dashboards. Coordinators see their daily workload and patient alerts; managers see team performance and bottlenecks; and leadership gets an instant pulse on organizational KPIs. There’s no more waiting for end-of-quarter reports to see how you’re doing.
- Customizable reports: Our reports aren’t just generic data dumps. They are customizable to focus on the metrics that drive modern healthcare success, including Value-Based Care performance, readmission rates, and key patient engagement scores. You can prove your value with hard data.
- Proactive alerts: The system doesn’t just display information; it alerts you when something needs immediate attention. You get automated notifications for critical issues like imminent care gaps, missed high-priority appointments, or compliance flags.
Real-time visibility transforms decision-making from an educated guess into a strategic imperative. When a team manager sees a sudden spike in missed follow-up calls in the southern region, they can reallocate resources today, not next month. When leadership sees a successful reduction in preventable readmissions in a specific service line, they can instantly replicate that workflow across the entire health system.
blueBriX ties intelligent integration, AI-driven foresight, and automated efficiency together into a continuous loop of learning and improvement, ensuring your organization moves from reactive management to continuous, strategic optimization.
5. Patient engagement capabilities
Even the most sophisticated care plan in the world will go useless if the patient doesn’t follow it. Care coordination shouldn’t stop at the clinic door. The new objective is simple: actively involve and empower patients in their own health journey. blueBriX extends your care team’s reach directly into the patient’s hands, making adherence easy and transparent.
How blueBriX keeps your patients active and engaged:
- Patient portals and mobile apps: We provide user-friendly patient portals and mobile apps that serve as the patient’s central command center. Here, they can view their care plan, check upcoming appointments, and access educational materials all without needing to call the office.
- Automated reminders: Adherence often comes down to simple reminders. Our system sends timely, automated alerts for medications, appointments, and preventive screenings. It’s gentle prompting that makes it easy for patients to stay on track.
- Interactive questionnaires & feedback loops: Patients can easily share key information back with their care team through interactive questionnaires. They can log symptoms, track medication adherence, and provide satisfaction scores, giving your coordinators an instant, objective view of how they are doing between visits.
- Telehealth and virtual access: Seamless integration of telehealth and virtual coaching means patients can connect with their providers from anywhere, breaking down barriers of time and distance to ensure they get support exactly when they need it.
When patients feel involved, informed, and supported, they become empowered partners in their health. This leads directly to better adherence to care plans, a dramatic reduction in preventable complications, and significantly higher patient satisfaction scores. blueBriX doesn’t just coordinate care for the patient; it helps the patient coordinate their own health.
6. Scalability across care models
Investing in a platform is a long-term decision. You need a solution that works just as well for a focused specialty clinic today as it will for a vast, integrated health network five years from now. blueBriX is built to grow with you. We don’t believe in rip-and-replace solutions; we designed the platform with a modular architecture that can expand and adapt to any challenge you face.
How we future-proof your investment:
- Non-disruptive workflows: Need to add a new specialty workflow or launch a new initiative? Our modular design means you can spin up new programs from chronic care management to behavioral health without disrupting existing, mission-critical processes. It’s seamless, plug-and-play evolution.
- Open ecosystem: As technology advances, your needs will change. blueBriX makes it easy to integrate new third-party tools, devices, and AI solutions whenever you need them. You’re never locked into a closed system.
- Supporting multiple care models: Whether you operate under a traditional Fee-for-Service model or are fully invested in complex Value-Based Care (VBC) networks and ACOs, blueBriX is engineered to support your unique business rules and documentation requirements. It’s the one foundation that powers every model, from Direct Primary Care (DPC) to global health systems.
With blueBriX, you aren’t just buying a solution for your current problems; you are acquiring a future-proof foundation that ensures your organization can remain agile, competitive, and ready for whatever the next generation of healthcare demands.
From reactive to proactive coordination
blueBriX transforms care coordination from a reactive administrative function into a proactive, intelligent, and patient-centered orchestration engine.
- Comprehensive Orchestration: Native and third-party integration ensures all care touchpoints are connected.
- Proactive Care: AI and predictive analytics allow anticipatory intervention.
- Operational Efficiency: Automation frees coordinators to focus on high-value tasks.
- Measurable Outcomes: Real-time dashboards track KPIs and VBC performance.
- Patient-Centered: Digital engagement empowers patients and caregivers.
- Scalable: Suitable for any organization, from small clinics to global networks.
Strategic recommendations for effective care coordination
Implementing intelligent care coordination demands strategic planning, process alignment, and organizational readiness. The following recommendations help healthcare organizations maximize the benefits of orchestration platforms like blueBriX.
1. Start with a clear vision and objectives
Key Actions:
- Define the goals of care coordination (e.g., reduce readmissions, improve patient engagement, optimize VBC outcomes).
- Align objectives with organizational strategy and population health priorities.
- Communicate the vision across leadership and frontline teams.
A clearly defined vision ensures alignment, focus, and measurable success.
2. Assess current workflows and gaps
Key Actions:
- Map existing care coordination processes, referral pathways, and communication flows.
- Identify bottlenecks, duplicated tasks, and points of patient disengagement.
- Prioritize areas with the greatest impact on outcomes and efficiency.
3. Integrate technology diligently
Key Actions:
- Leverage intelligent orchestration platforms for automation, AI, and real-time dashboards.
- Ensure interoperability with EHRs, telehealth platforms, lab systems, and third-party solutions.
- Maintain compliance with HIPAA, GDPR, and other regulations.
Technology should augment human coordination, not replace it. Platforms like blueBriX integrate seamlessly, allowing teams to focus on clinical interventions rather than administrative tasks.
4. Engage patients and caregivers
Key Actions:
- Provide patients with portals, mobile apps, and communication tools to access their care plans.
- Encourage self-management, symptom tracking, and active participation in decision-making.
- Offer educational content tailored to patient literacy and needs.
5. Establish clear roles and accountability
Key Actions:
- Assign coordinators or teams to each patient based on complexity and risk.
- Define responsibilities for scheduling, follow-ups, documentation, and communication.
- Use dashboards and KPI reporting to ensure accountability and transparency.
Clear accountability reduces gaps, prevents duplication, and ensures tasks are completed on time.
6. Measure, analyze, and iterate
Key Actions:
- Define KPIs aligned with clinical, operational, and financial goals.
- Use real-time dashboards to monitor referral efficiency, care plan adherence, patient engagement, and outcomes.
- Conduct periodic reviews and adjust workflows, automation rules, and resource allocation.
7. Promote a culture of continuous improvement
Key Actions:
- Encourage feedback from care coordinators, providers, and patients.
- Celebrate successes and highlight process improvements.
- Use lessons learned to scale best practices across departments or locations.
Intelligent care coordination is a dynamic, evolving process wherein continuous evaluation and adaptation are critical to long-term success.
8. Scale thoughtfully across care models
Key Actions:
- Pilot new workflows in a single department or population before organization-wide implementation.
- Use modular orchestration platforms to add new care pathways, providers, and third-party tools without disrupting existing processes.
- Standardize reporting and KPIs for cross-department or cross-location comparison.
Strategies for effective care coordination
Organizations that combine strategy, technology, and patient engagement achieve measurable outcomes, reduced costs, and higher satisfaction across all care models.
- Alignment and vision: Start with clear goals and a shared vision.
- Process optimization: Map workflows, identify gaps, and streamline tasks.
- Technology as an enabler: Integrate AI, automation, and dashboards to support human coordination.
- Patient-centered approach: Engage patients and caregivers actively in their care.
- Accountability and measurement: Assign responsibilities and track KPIs to ensure results.
- Continuous improvement: Adapt processes based on performance and feedback.
- Scalable implementation: Roll out in phases and standardize practices for growth.
Why blueBriX matters now
Effective care coordination is no longer a luxury or a footnote. It is the single most important strategic imperative in modern healthcare.
To survive and thrive in today’s environment, organizations must do more than just manage patients; they must proactively orchestrate their entire care journey.
For every organization, from ACOs striving for shared savings, to DPCs focused on deep patient relationships, to specialized behavioral health centers, and massive global networks, intelligent care coordination is the game-changer. It is the key to turning fragmented, reactive processes into seamless, measurable, and deeply patient-centered care.
The shift is simple: move from managing tasks to mastering outcomes. That is the power blueBriX puts in your hands.
Key Takeaways
- Care Coordination is the backbone of quality care: Aligning providers, patients, and data ensures the right care is delivered at the right time.
- AI and automation enable proactive intervention: Predictive analytics, workflow automation, and real-time dashboards allow teams to act before issues escalate.
- Patient engagement drives better outcomes: Empowering patients with access to care plans, reminders, and educational resources increases adherence, reduces complications, and boosts satisfaction.
- KPIs guide continuous improvement: Measuring referral efficiency, care plan adherence, clinical outcomes, and operational metrics provides actionable insights for optimization.
- Scalable and flexible platforms are essential: Organizations must be able to integrate native and third-party solutions, adapt to new care models, and operate across regions seamlessly.
Your 5-step roadmap to intelligent care coordination
For healthcare leaders, care coordinators, and key decision-makers, transforming coordination isn’t a complex mystery—it’s a clear process. Here are the five essential steps you can take right now to move your organization toward proactive, intelligent care:
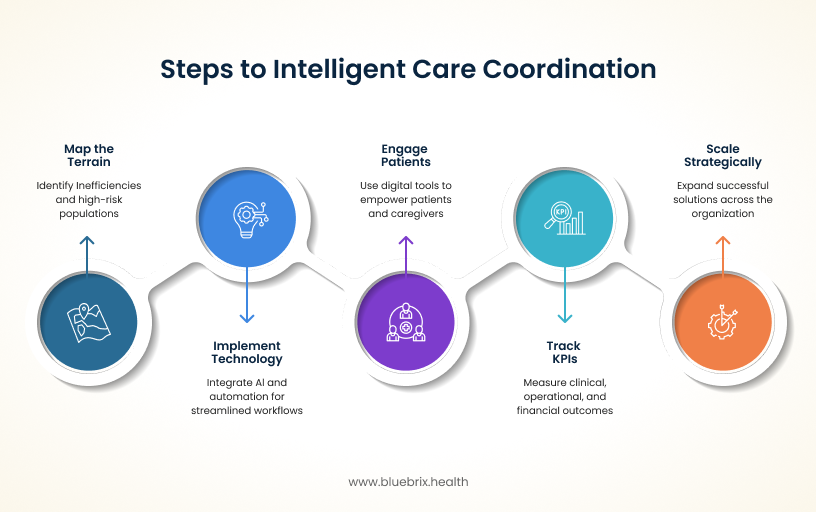
- Map the terrain and find the friction: Start with a deep dive into your current processes. Where are the bottlenecks? Where are patients falling through the cracks? Clearly identify existing inefficiencies, administrative overload, and the specific high-risk patient populations most likely to benefit from immediate support.
- Make technology your co-pilot: Stop layering patches onto old systems. Implement a true, intelligent orchestration platform like blueBriX. This isn’t just about software; it’s about embedding AI and automation to streamline workflows, eliminate manual tasks, and give everyone clear, unified data visibility.
- Turn patients into partners: The journey doesn’t end when the patient leaves the clinic. Actively use digital tools such as portals, mobile apps, and automated reminders to empower patients and their caregivers. An engaged patient is an adherent patient, and that directly translates to better outcomes.
- Focus on KPIs that matter the most: You can’t improve what you don’t measure. Establish and relentlessly track Key Performance Indicators (KPIs) across all three crucial domains – clinical (outcomes, readmissions), operational (workflow efficiency, cycle time), and financial (cost of care, VBC compliance).
- Think big, stay focused: The most successful transformations begin with confidence, not chaos. Pilot solutions with a specific department (like cardiology or behavioral health) or a defined patient population (e.g., congestive heart failure patients). Prove the ROI and refine the process, then scale strategically across the rest of the organization.