Healthcare leaders constantly see their teams pushed to the limit. Calendars are packed, staff are multitasking all day, and everyone looks overwhelmed. Yet, despite the effort, clinical outcomes, operational efficiency, and productivity often remain flat. This disconnect leaves many leaders wondering why their organization isn’t seeing the return they expect from such a hard-working workforce.
The real issue isn’t effort. It’s underutilization that hides inside fragmented workflows and multi-system complexity. For example, nearly half of healthcare data goes unused in daily decision-making, and staff lose hours each week jumping between EHRs, spreadsheets, chat threads, and manual follow-ups. Add the ongoing physician and nursing shortages, and the strain becomes even more visible.
It’s easy to assume that adding more staff will balance the workload, but hiring into broken workflows often creates more complexity rather than relief. More people mean more communication loops, more handoffs, and more opportunities for tasks to fall through the cracks. Leaders expect productivity to rise, but instead, the same structural problems multiply across a larger team.
This gap between visible effort and actual performance is what silently drains ROI. Organizations lose hours of staff time not because teams lack skill or commitment, but because the system doesn’t give them a clear, consistent way to work. And without that structure, even small inefficiencies grow into major operational losses over time.
Recognizing this hidden crisis is the turning point. This is why the conversation must start with understanding what actually drives underutilization in care teams. That’s the foundation for everything that follows.
The root causes of underutilization in modern care teams
Many healthcare leaders assume underutilization happens because teams are short staffed or not working fast enough. In reality, the biggest blockers come from inside everyday operations. When roles aren’t clearly defined, when people work across too many systems, or when team members depend on scattered communication, productivity drops no matter how skilled your staff is.
Imagine asking three different people to follow up on the same patient because nobody is sure who owns the task. Or picture a clinician switching between multiple EHRs just to confirm a medication list. These small inefficiencies pile up across the day and quietly drain your team’s time and energy.
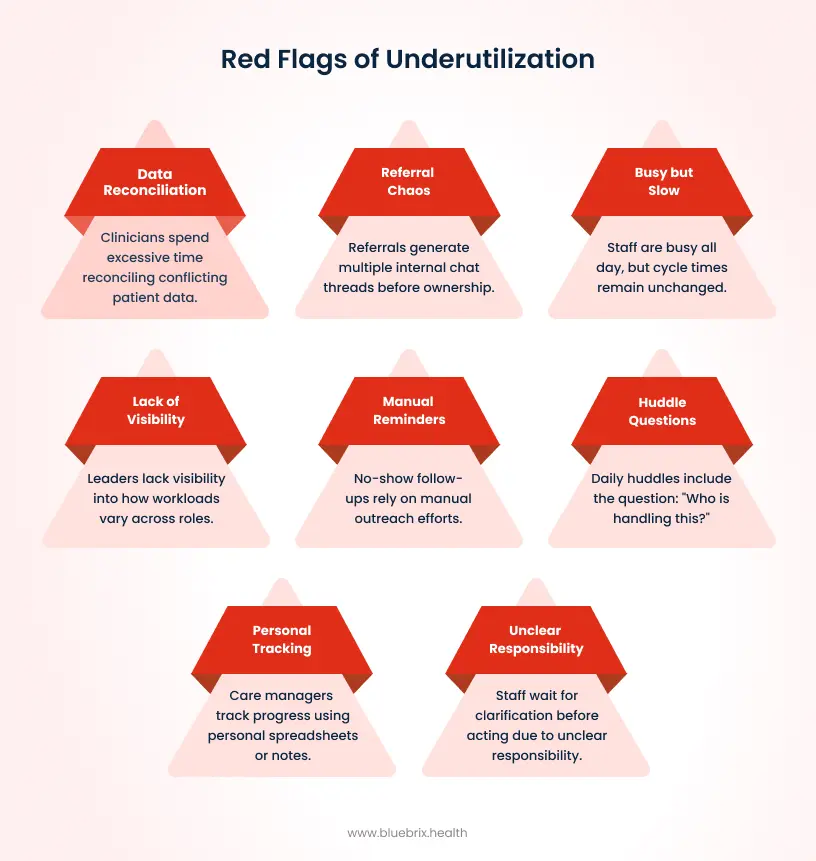
To understand this better, let’s break down the specific workflow issues that fuel underutilization and make teams feel overwhelmed despite working hard.
- Fragmented workflows slow everyone down. When staff jump between tools for scheduling, documentation, follow-ups, and referrals, they lose momentum and focus. A medical assistant who spends ten minutes just finding the right spreadsheet update has already lost valuable time they could have spent on patient care.
- Multi-EHR complexity is another major drain. Clinicians often wait for corrected data from different systems or spend hours reconciling conflicting information. This is mentally exhausting and delays care decisions.
- Lack of ownership leads to tasks slipping through the cracks. When responsibilities are shared but not assigned, everyone assumes someone else will handle it. That’s how missed follow-ups and delayed referrals happen.
- Low-value admin work chips away at the day. Staff spend a large portion of their time doing manual reminders, verifications, or data cleanup instead of using their clinical skills.
- Visibility gaps mean some team members burn out while others have unused capacity. Without a clear view of workload distribution, leaders can’t allocate resources effectively.
These challenges show one thing clearly: the problem isn’t the people. It’s the system around them. To fix this, teams need structured clarity in the form of clear mandates.
Clear mandates and how they solve ambiguity
Clear mandates give healthcare teams the structure they’ve been missing. Instead of relying on assumptions, hallway conversations, or scattered messages, tasks are assigned automatically based on rules tied to each role. This removes the ambiguity that often slows teams down and replaces it with predictable, accountable workflows.
What clear mandates really mean
A clear mandate isn’t just a written instruction. It is a system-enforced rule that assigns the right task to the right person at the right moment. For example, in the VA’s STRIDE program, mobility-related tasks were assigned automatically to physical therapists or nursing staff based on predefined criteria. Staff didn’t need to clarify responsibilities or chase updates. The system ensured that every task had a correct and immediate owner. This level of clarity removes the “Who’s handling this?” question that often interrupts daily work.
How clear mandates improve accountability
When a task is tied to a single owner, it stops getting lost in group chats, shared inboxes, or spreadsheets. Staff no longer need to sift through messages to figure out what’s expected of them. Leaders also gain visibility into progress without constantly following up. This means instead of a follow-up reminder floating in an email thread, the system assigns it directly to the care coordinator responsible, logs the deadline, and tracks completion. Accountability becomes natural, not forced.
Why clear mandates reduce errors and rework
With clear, standardized handoffs, teams avoid the mistakes that happen when roles overlap or communication splinters. When staff no longer need to double-check who should act or redo tasks that someone else has already started, they work with more confidence and less cognitive load.
Hospitals using mandate-driven workflows have seen fewer missed steps, smoother transitions between roles, and more consistent outcomes because work moves predictably from one person to the next.
By removing ambiguity, clear mandates create the structure teams need to execute reliably. But mandates reach their full potential only when paired with integrated workflows that unify data and eliminate manual coordination.
Integrated workflows: the support system behind high performance
Clear mandates tell teams who is responsible. Integrated workflows make sure the work itself moves smoothly, without delays or manual coordination. When data, tasks, and documentation flow through one unified system, staff can finally focus on patient care instead of fixing the process around it.
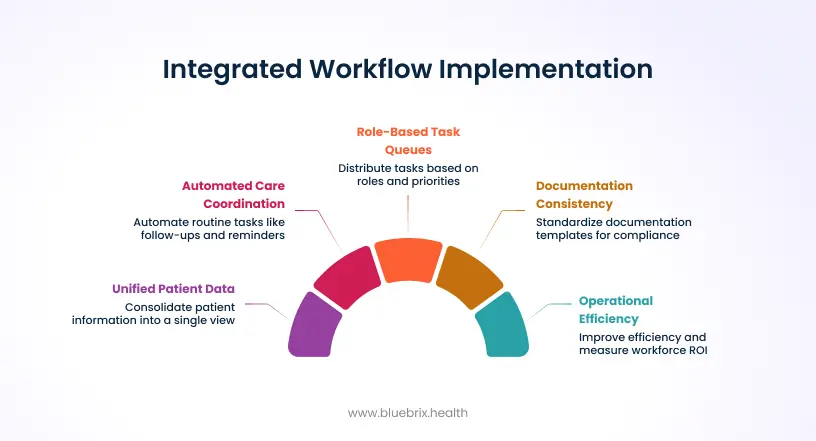
Integrated workflows strengthen the workforce by bringing four major capabilities together.
Unified patient data across systems
Instead of jumping between multiple EHRs, staff see all patient information in one place. This single view removes the confusion caused by conflicting records and reduces the hours clinicians spend verifying details. This means a clinician reviewing lab results doesn’t need to open three systems or wait for a coordinator to confirm which version is correct. Everything is already unified. With clearer data comes faster, more confident decision-making.
Automated, end-to-end care coordination
Integrated care coordination workflows take over routine but essential tasks like follow-ups, reminders, referral tracking, and escalation. This automation frees teams from doing repetitive work manually and helps them focus on tasks that genuinely require their expertise. For example, when a referral is overdue, the system automatically sends patient reminders and escalates to the right team member without anyone having to chase it. This shifts teams from reactive to proactive operations.
Role-based task queues that keep work moving
Each staff member gets a dynamic task queue based on their role, priorities, and real-time workload. This eliminates idle time, reduces bottlenecks, and distributes tasks more evenly across the team. That means lab follow-ups automatically land in the lab coordinator’s queue. Medication reconciliation flows to the nurse responsible. No one waits for direction. This gives leaders predictable throughput and prevents overload.
Documentation consistency that supports compliance
Integrated workflows standardize documentation templates and ensure each required field is captured. That consistency reduces mistakes, accelerates billing, and improves audit readiness. Teams don’t need to remember every detail because the workflow guides them through the structure.
Integrated workflows take the clarity created by mandates and turn it into real operational efficiency. Once these workflows are in place, organizations can start measuring how much capacity, time, and value they’re gaining. That’s where workforce ROI becomes visible, which is what we focus on the next section.
Measuring workforce ROI: the real impact of better utilization
Once clear mandates and integrated workflows are in place, the impact becomes measurable almost immediately. Leaders can see exactly how time is being saved, how capacity is expanding, and where care quality and financial outcomes are improving. Instead of relying on assumptions, organizations finally have concrete proof of what better utilization delivers.
Hours recovered across care teams
- Automation and structured workflows reduce the manual work that typically slows staff down.
- Clinicians regain time from documentation and data verification.
- Administrative teams spend less time coordinating follow-ups or managing back-and-forth communication.
These reclaimed hours translate directly into more patient-facing time and faster operational cycle times.
Higher patient panel capacity without additional hiring
When teams no longer lose hours to fragmented systems, they can support more patients with the same staffing levels. Clinicians manage larger patient panels with less strain, and administrative teams handle more referrals and follow-ups because the routine work is automated. This allows organizations to grow without immediately increasing headcount.
Fewer no-shows and closed care gaps
Automated reminders, real-time alerts, and integrated patient tracking reduce missed appointments and overlooked interventions. Teams no longer spend hours trying to manually manage care gaps, because the system keeps outreach and follow-ups on track. The improvement shows up in both patient outcomes and operational performance.
Reduced denial rates and documentation errors
With standardized templates and unified data, documentation becomes more accurate and consistent. Claims go out cleaner, denials decrease, and reimbursements arrive faster. Teams waste less time fixing incomplete notes or reworking claims.
Lower turnover and higher staff satisfaction
When work is clear, structured, and balanced, teams feel supported rather than overwhelmed. This reduces burnout and turnover, which in turn lowers recruiting and training costs. A stable and well-supported workforce delivers better care and stronger operational continuity.
These outcomes prove that workforce ROI isn’t theoretical. It’s visible and measurable when organizations remove ambiguity, automate routine work, and unify their workflows. The next step is understanding how a platform like blueBriX brings these capabilities together in practice.
The anatomy of a high-performance system
A platform like blueBriX turns the concepts of clear mandates and integrated workflows into everyday reality. Instead of relying on manual coordination, fragmented systems, and scattered communication, blueBriX automates the structure your teams need to work efficiently and confidently.
- blueBriX supports clear mandates by assigning tasks automatically based on role, rules, and workflow logic. Whether it’s a referral follow-up, an overdue care gap, or an insurance verification, every task is routed directly to the right person without guesswork. This gives teams clarity and eliminates the back-and-forth that usually slows work down.
- At the same time, the platform integrates data across multiple EHR systems, pulling everything into a single, reliable view. Clinicians don’t need to compare records or wait for someone to reconcile conflicting information. Coordinators don’t lose hours cleaning up data before taking action. blueBriX removes that friction so decisions move faster.
- Role-based task queues keep work flowing. Each staff member gets a real-time list of what needs attention, in the right order, based on their responsibilities and capacity. Leaders gain visibility into workloads and can spot bottlenecks early, preventing overload before it happens.
- Documentation becomes more consistent too. blueBriX provides templates and workflow guidance that help staff capture required information accurately. This reduces claim errors, supports compliance, and shortens the revenue cycle.
- Finally, the platform gives leaders a clear window into performance. Real-time analytics show productivity levels, task completion rates, and capacity trends. This helps leaders understand where improvement is needed and where teams are excelling.
In short, blueBriX doesn’t just lighten the workload. It creates a fully integrated environment where staff can work at their best without being weighed down by fragmented processes. This sets the stage for the real-world scenario in the next section.
Real-world scenario: How a behavioral health group fixes underutilization?
A multi-location behavioral health group was struggling with slow, disjointed operations. Teams worked across four different EHR systems, and critical updates lived in emails, spreadsheets, and chat messages. Every day, staff spent valuable time clarifying information, retracing steps, and verifying conflicting records. This made it difficult to keep up with rising patient volume despite having skilled clinicians and care managers.
Leadership initially believed they had a staffing shortage. But deeper analysis showed something else: The workforce wasn’t lacking capacity. It was lacking the infrastructure to use that capacity effectively.
Routine tasks required comparing records, confirming details through side channels, and manually tracking progress. Staff appeared busy, yet a large portion of their day was being consumed by system navigation rather than meaningful care coordination. Productivity remained flat not because teams weren’t working hard, but because fragmentation prevented their effort from translating into throughput.
This was the turning point. The organization saw that underutilization wasn’t a people problem. It was a workflow design problem.
What improved after implementing clear Mandates and integrated workflows?
After the organization adopted a system built around clear mandates, task ownership became explicit instead of assumed. Follow-ups, referrals, escalations, and outreach were automatically routed to the correct role based on patient context and priority. This eliminated the ambiguity that previously caused work to circulate between staff or stall while waiting for clarification.
Integrated workflows created an equally meaningful shift. Patient data from all four EHR systems was unified into a single, validated record, removing the need for constant reconciliation. Instead of spending hours each week verifying information, care managers and clinicians could act immediately with confidence.
Routine coordination tasks that once depended on emails, spreadsheets, or manual reminders now ran automatically. Overdue outreach, escalation triggers, and pending referrals were handled by the workflow engine, freeing staff from repetitive administrative labor.
Within weeks, cycle times shortened, task backlogs shrank, and frontline teams recovered hours that had been previously lost to fragmentation. Productivity increased not by adding staff, but by finally giving the existing workforce a system that allowed them to operate at full capacity.
What shifted with clear mandates and integrated workflows?
When the organization adopted a system that enforced clear mandates, task routing stopped depending on informal communication. Activities such as outreach, referral tracking, and post-visit follow-up were instantly assigned based on role, priority, and patient context. This eliminated ambiguous ownership and prevented work from circulating between staff.
Integrated workflows had an equally significant impact. Patient data from all four EHRs was synchronized into a single, validated record. This removed the need for reconciliation and allowed both clinicians and care managers to make decisions based on consistent, up-to-date information. Instead of spending their mornings untangling data discrepancies, teams could begin acting on patient needs immediately.
The result: measurable utilization gains without adding staff
The shift was visible within weeks. Time previously lost to verification, coordination, and manual tracking was reclaimed. Cycle times shortened because tasks no longer stalled between handoffs. Care managers were able to manage higher caseloads without compromising patient engagement, and the organization saw a meaningful reduction in missed follow-ups and unresolved care gaps.
Financial outcomes improved as well. Standardized workflows reduced documentation variability, leading to cleaner claims and fewer avoidable denials. With more predictable workloads and fewer operational frustrations, staff retention stabilized, creating continuity that had been difficult to maintain before.
The experience confirmed an important truth: underutilization often has little to do with effort or staffing volume. It is a function of workflow design. When that design is corrected, existing teams consistently outperform expectations.
The Cost of Inaction
Ambiguity isn’t just inefficient; it introduces clinical and financial risk.
When ownership is unclear, or when data must be manually reconciled:
- High-risk patients experience delays in follow-up.
- Referrals stall because no single role is accountable.
- Care gaps stay open longer than they should.
- Documentation variability leads to preventable denials.
- No-shows increase because reminders aren’t systematically triggered.
- Staff burnout rises as teams compensate for broken processes.
Fragmentation compounds over time. What begins as a small operational inconvenience becomes a system-wide capacity loss that directly affects patient outcomes and organizational sustainability.