Medical coding is the unsung hero of healthcare administration, the vital process that translates medical services, procedures, and diagnoses into a universal language for billing, reimbursement, research, and so much more. If you’ve ever wondered how a doctor’s visit turns into an insurance claim, you’re about to find out!
What is Medical Coding? Defining the Process and Its Importance
At its core, medical coding is the transformation of healthcare diagnoses, procedures, medical services, and equipment into alphanumeric codes. Imagine a physician documenting a patient’s visit – the symptoms, the diagnosis, the treatment plan, the procedures performed. Medical coders meticulously review this documentation and assign standardized codes using specific classification systems.
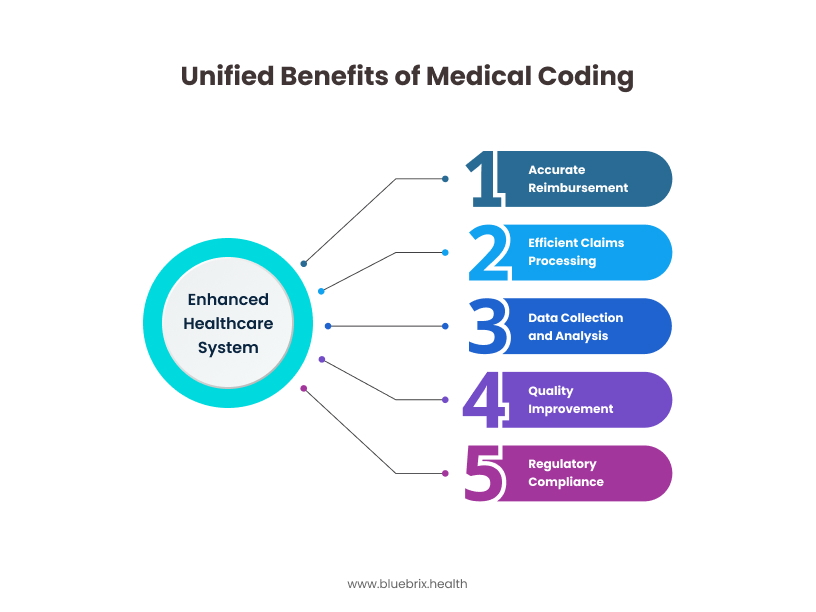
Why is this process so crucial? Well, think of it like this: without a standardized system, it would be impossible for healthcare providers to get paid accurately, for insurance companies to process claims efficiently, for public health agencies to track diseases, or for researchers to analyze health trends. Medical coding acts as the backbone of the healthcare financial and administrative infrastructure. It ensures:
- Accurate Reimbursement: By translating services into billable codes, providers receive appropriate payment from insurance companies and government payers.
- Efficient Claims Processing: Standardized codes allow for streamlined electronic claims submission and processing, reducing administrative burdens and delays.
- Data Collection and Analysis: Coded data is essential for tracking disease prevalence, identifying public health trends, evaluating the effectiveness of treatments, and conducting medical research.
- Quality Improvement: Analysing coded data can help identify areas for improvement in patient care and outcomes.
- Compliance with Regulations: Accurate coding helps healthcare organizations adhere to legal and regulatory requirements.
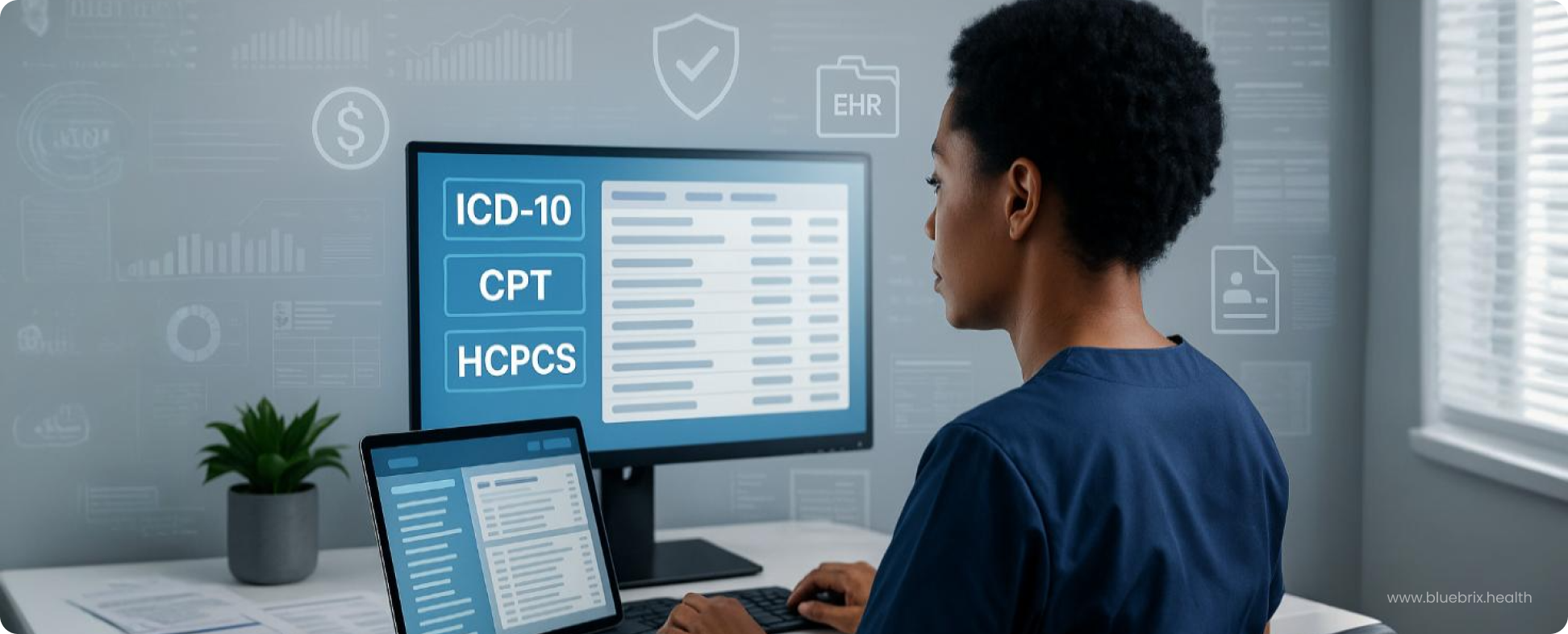
An Overview of Major Coding Systems: ICD, CPT, HCPCS
The world of medical coding revolves around three primary coding systems:
- International Classification of Diseases (ICD): Currently in its 10th revision with clinical modification (ICD-10-CM) for diagnoses used in the United States, this system is maintained by the World Health Organization (WHO) and adapted by the National Center for Health Statistics (NCHS) and the Centers for Medicare & Medicaid Services (CMS) in the US. ICD-10-CM codes describe what the patient’s illness or condition is. For inpatient hospital procedures, the US uses ICD-10-PCS (Procedure Coding System). These codes are crucial for tracking morbidity and mortality, justifying medical necessity, and facilitating reimbursement.
- Current Procedural Terminology (CPT): Developed and maintained by the American Medical Association (AMA), CPT codes describe the medical, surgical, and diagnostic services performed by physicians and other healthcare providers. These are primarily used for outpatient and physician billing. CPT includes a main body of codes and Category II (performance measurement) and Category III (emerging technology) codes. Understanding modifiers, which provide additional information about a procedure or service, is also essential in CPT coding.
- Healthcare Common Procedure Coding System (HCPCS): This system is used to report services, procedures, and supplies not included in the CPT codes. It has two levels:
- Level I: These are the CPT codes themselves.
- Level II (National Codes): These alphanumeric codes are developed and maintained by CMS and other healthcare industry groups. They cover a wide range of items and services, such as ambulance services, durable medical equipment (DME), prosthetics, orthotics, and supplies (DMEPOS), as well as certain drugs and biologicals.
These three systems work in tandem to provide a comprehensive language for describing all aspects of a patient’s healthcare encounter.
Understanding the Legal and Regulatory Landscape of Medical Coding
Medical coding operates within a complex web of laws and regulations designed to ensure data privacy, security, and the integrity of the healthcare system. Key pieces of legislation and regulations impacting medical coding include:
- Health Insurance Portability and Accountability Act of 1996 (HIPAA): This landmark legislation has significant implications for medical coding. The Privacy Rule protects the confidentiality of Protected Health Information (PHI), and coders must be mindful of not including unnecessary details in coding or billing. The Security Rule mandates safeguards for electronic PHI, which is crucial as most coding and billing processes are now electronic. The Transactions and Code Sets Rule standardized the electronic exchange of health information, including the use of specific code sets (like ICD-10, CPT, and HCPCS) for claims submission.
- False Claims Act: This act imposes liability on individuals and companies who knowingly submit false or fraudulent claims for payment to the federal government. Accurate coding is paramount to avoid violations of this act. Upcoding (using a higher-level code than the service documented) or unbundling (separating services that should be billed together) can lead to severe penalties.
- Anti-Kickback Statute and Stark Law: While not directly coding regulations, these laws influence how services are billed and coded, particularly concerning referrals and financial relationships between healthcare providers.
- Payer-Specific Rules and Guidelines: Insurance companies (both private and government payers like Medicare and Medicaid) often have their own specific coding guidelines, coverage policies, and reimbursement rules that coders must adhere to.
Navigating this legal and regulatory landscape requires continuous learning and meticulous attention to detail from medical coders.
The Importance of Accuracy and Compliance in Medical Coding
Accuracy and compliance are not just best practices in medical coding; they are fundamental requirements. Inaccurate coding can lead to a cascade of negative consequences:
- Financial Losses: Under-coding can result in lost revenue for healthcare providers, while over-coding or fraudulent coding can lead to penalties, fines, and even legal action.
- Claim Denials and Delays: Errors in coding are a major reason for insurance claim denials and delays, disrupting cash flow for providers and causing frustration for patients.
- Audit Risks: Inaccurate or non-compliant coding practices can trigger audits from payers and regulatory agencies.
- Flawed Data and Reporting: Inaccurate coding compromises the integrity of healthcare data, affecting research, public health initiatives, and quality improvement efforts.
- Reputational Damage: Consistent coding errors can damage a healthcare organization’s reputation and erode patient trust.
Therefore, rigorous training, ongoing education, regular audits, and robust internal controls are essential to ensure coding accuracy and compliance.
The Future of Medical Coding: Trends and Technologies
Medical coding is a dynamic and essential field at the intersection of healthcare, finance, and technology. Understanding its fundamental principles, the roles of medical coders, the intricacies of coding systems, the importance of legal and regulatory compliance, and the emerging trends will be crucial for anyone involved in the healthcare ecosystem. Some key trends and technologies shaping its future include AI, automation, NLP, value-based care, telehealth, remote services, data analytics etc.
Overview of Core US Medical Coding Systems
Accurate medical coding is fundamental to your organization’s financial health, compliance, and data-driven decision-making. The US system relies on three key sets:
- ICD: These alphanumeric codes, updated annually by CMS, are critical for demonstrating medical necessity, securing reimbursement, tracking public health, and informing quality initiatives. ICD-10-CM is for diagnoses across all settings and ICD-10-PCS for inpatient hospital procedures only. Mastering their use requires understanding the codebooks and the mandatory Official Guidelines.
Challenges include documentation gaps, update management, and navigating complex cases and payer rules, all requiring strategic solutions like CDI programs and technology adoption.
- CPT: Maintained by the AMA, CPT codes report medical, surgical, and diagnostic services, primarily in outpatient settings. Understanding Category I (common procedures), Category II (performance tracking), and Category III (emerging technologies) is key.
Modifiers are crucial for providing essential context to the billed service. Accurate E/M coding (for evaluation and management services) and adherence to surgical, radiology, pathology, and anesthesia-specific guidelines directly impact reimbursement and compliance.
- HCPCS (Healthcare Common Procedure Coding System): This system includes Level I (CPT) and Level II (National Codes), the latter covering services and supplies not in CPT, like DME (Durable Medical Equipment) and drugs. Level II codes, often temporary, are vital for billing these specific items and services according to payer rules.
Investing in accurate and efficient coding processes, including well-trained staff and appropriate technology, directly translates to improved revenue cycle management, reduced audit risks, and better data for strategic planning in the evolving US healthcare landscape. Understanding these core systems at a high level empowers you to make informed decisions about your coding solutions.
Coding for Behavioral Health
Unique Considerations for Behavioral Health Coding
Behavioral health coding presents distinct challenges compared to general medical coding. The subjective nature of many mental health diagnoses, the emphasis on psychotherapy and counselling, and the evolving landscape of telehealth delivery all contribute to its complexity. Unlike coding for a broken bone or a routine physical, behavioral health coding often requires a deep understanding of diagnostic criteria, the nuances of therapeutic interventions, and specific payer requirements that can differ significantly from those for physical health services. Furthermore, maintaining patient privacy and confidentiality, as mandated by HIPAA, is particularly critical in behavioral health records and coding practices.
Common Mental Health Disorders and Relevant ICD-10-CM Codes
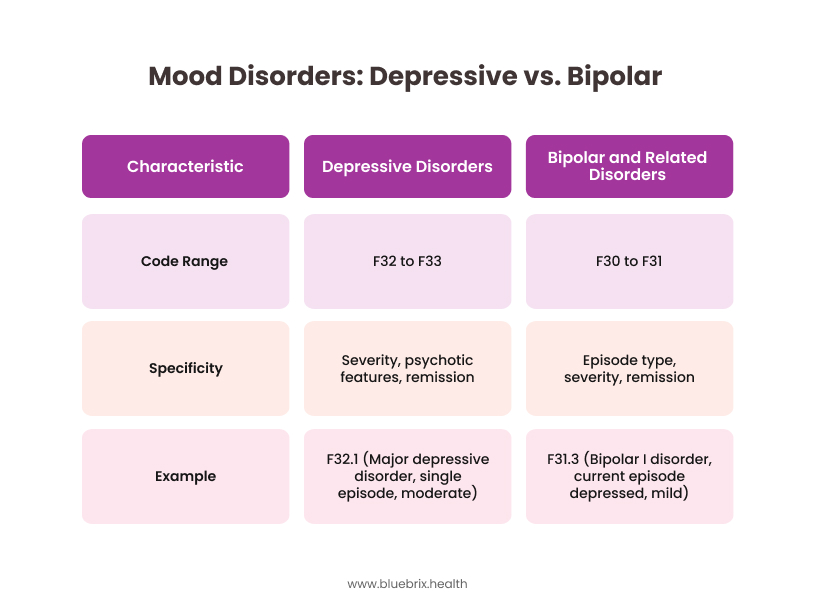
Accurate diagnosis coding is the foundation of compliant behavioral health billing. The ICD-10-CM Chapter V (Mental, Behavioral and Neurodevelopmental disorders) provides the framework for classifying these conditions. Here’s a look at some common categories and examples relevant to your coding solutions:
Anxiety Disorders:
- Generalized Anxiety Disorder: Typically coded as F41.1.
- Panic Disorder: Codes include F41.0 (panic disorder [episodic paroxysmal anxiety]) with or without agoraphobia (F40.0). Specificity can involve the frequency and severity of panic attacks.
- Other anxiety disorders like social anxiety disorder (F40.1), specific phobias (F40.2), and obsessive-compulsive disorder (F42) have their own distinct codes.
Psychotic disorders:
- Schizophrenia is categorized under F20, with subtypes like F20.0 (Paranoid schizophrenia), F20.1 (Disorganized schizophrenia), and F20.9 (Schizophrenia, unspecified). The specific subtype and the course of the illness (e.g., continuous, episodic with progressive deficit) are important coding elements.
- Other psychotic disorders include schizoaffective disorder (F25) and delusional disorder (F22).
Substance use disorders:
- These are coded under F10-F19, with the specific substance identified (e.g., F10 for alcohol, F12 for cannabis) and further specification for the pattern of use (e.g., abuse, dependence), associated complications, and remission status. For example, F10.20 (Alcohol dependence, uncomplicated) differs significantly from F10.231 (Alcohol dependence with withdrawal, with perceptual disturbances).
Personality Disorders:
- These are found under F60-F69, with distinct codes for each type, such as F60.3 (borderline personality disorder) and F60.0 (Paranoid personality disorder).
CPT Codes Specific to Psychiatric Services
While Evaluation and Management (E/M) codes are used in behavioral health, several CPT codes are specific to psychiatric services, reflecting the unique nature of these interventions:
Psychotherapy:
- Individual Psychotherapy: (+ Add on code)
- 90832 – Psychotherapy, 30 minutes with patient
- + 90833 – Psychotherapy, 30 minutes with patient when performed with an evaluation and management service (List separately in addition to the code for primary procedure)
- 90834 – Psychotherapy, 45 minutes with patient
- + 90836 – Psychotherapy, 45 minutes with patient when performed with an evaluation and management service (List separately in addition to the code for primary procedure), (Use 90836 in conjunction with 99202-99255, 99304-99316, 99341-99350) (Use 90838 in conjunction with 99202-99255, 99304-99316, 99341-99350)
- 90837 – Psychotherapy, 60 minutes with patient
- + 90838 – Psychotherapy, 60 minutes with patient when performed with an evaluation and management service (List separately in addition to the code for primary procedure).
- Psychoanalysis – 90845
- Family Psychotherapy: Codes 90846 (without the patient present), 50 Minutes
- Family Psychotherapy: Codes 90846 (without the patient present), 90847 -Family psychotherapy (conjoint psychotherapy) (with patient present), 50 minutes.
- Multiple-family group psychotherapy – Code 90849
- Group Psychotherapy: Code 90853 reports group therapy sessions. (Use 90853 in conjunction with 90785 for the specified patient when group psychotherapy includes interactive complexity)
Psychiatric Diagnostic Evaluations:
- Code 90791 is for a psychiatric diagnostic evaluation without medical services, while 90792 is for an evaluation that includes medical services. The choice depends on whether a physical exam or other medical assessments are part of the initial evaluation.
Medication Management:
- Codes 90863 (Pharmacologic management, including prescription and review of medication, with no more than minimal medical psychotherapy) and E/M codes (if significant evaluation and management services are provided beyond medication management) are used. The level of E/M code depends on the complexity of the patient’s condition and the time spent.
Specialized Treatment Modalities:
- Codes like 90901 (Biofeedback training by any modality) and 90880 (Hypnosis) exist for these specific interventions, requiring documentation that supports the use of these modalities.
Crisis Intervention Services:
- As mentioned earlier, 90839 and 90840 are used for psychotherapy for crisis. Other crisis intervention codes might apply depending on the setting (e.g., hospital emergency department).
Documentation Requirements for Behavioral Health Coding
Robust and specific documentation is paramount for accurate behavioral health coding and to support the medical necessity of services. Key elements include:
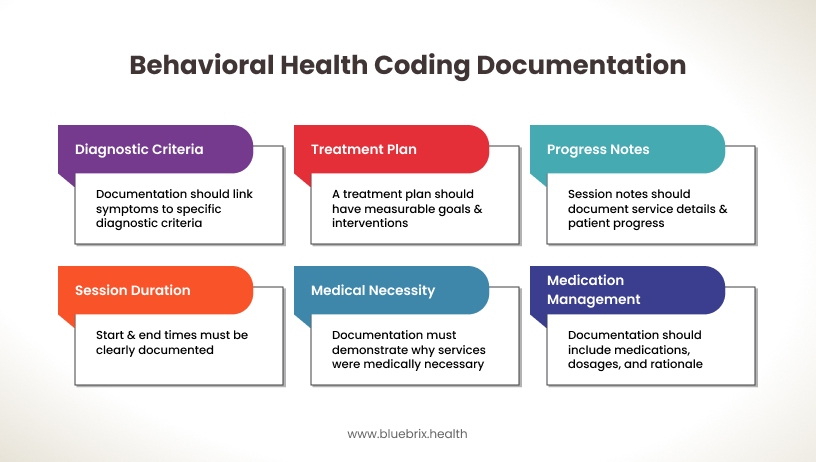
- DSM-5 (or most current edition) Diagnostic Criteria: Documentation should clearly link the patient’s symptoms and history to the specific diagnostic criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders.
- Treatment Plan: A well-defined treatment plan with measurable goals, objectives, and interventions is essential.
- Progress Notes: Each session note should document the date and time of service, the type of service, the content of the session (interventions used, patient’s response), progress towards treatment goals, and any changes to the treatment plan.
- Session Duration: For time-based psychotherapy codes, the start and end times of the session must be clearly documented.
- Medical Necessity: The documentation must clearly demonstrate why the services provided were medically necessary for the treatment of the patient’s condition.
- For Medication Management: Documentation should include the medications prescribed, dosages, frequency, and the rationale for medication management, including monitoring of side effects and efficacy.
Navigating Payer-Specific Rules and Guidelines for Behavioral Health Services
Payer rules for behavioral health services can be particularly complex and vary significantly among commercial insurers, Medicaid, and Medicare. Key considerations include:
- Prior Authorization: Many payers require prior authorization for certain behavioral health services, especially for intensive or long-term treatment. Understanding these requirements and obtaining necessary authorizations is crucial for avoiding claim denials.
- Coverage Limitations: Payers may have limitations on the number of sessions covered per year, the types of providers they credential for behavioral health services, and the specific diagnoses or treatment modalities they cover.
- Medical Necessity Criteria: While based on DSM criteria, payers may have their own interpretations of medical necessity for behavioral health services.
- Telehealth Coverage: Coverage for telehealth services in behavioral health can vary widely. It’s essential to understand each payer’s specific policies regarding eligible services, originating and distant site requirements, and the use of specific telehealth modifiers (e.g., GT, GQ, 95).
- Documentation Requirements: Payers may have specific documentation requirements beyond general coding guidelines for behavioral health services.
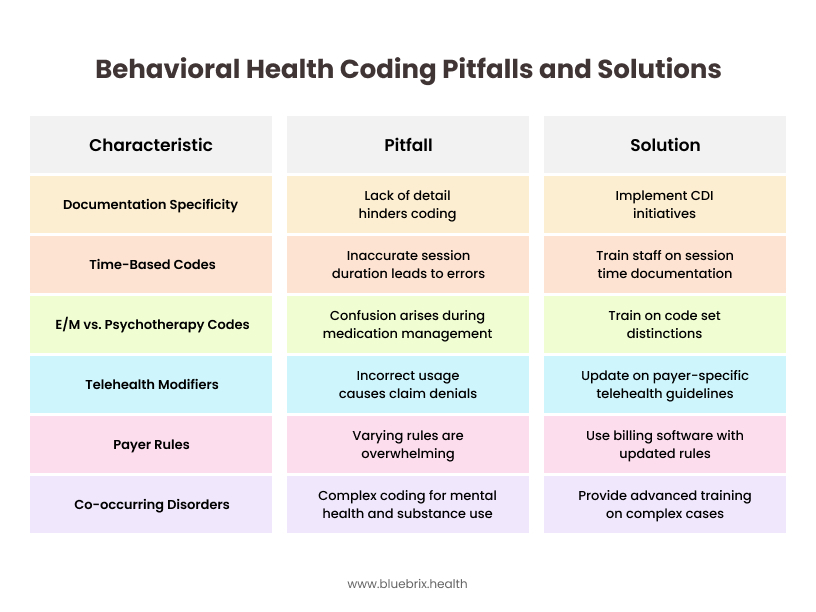
Common Coding Challenges in Behavioral Health and How to Overcome Them
Behavioral health coding presents several common pitfalls:
Telehealth and Behavioral Health Coding Considerations
The increasing adoption of telehealth in behavioral health has introduced new coding considerations:
- Place of Service (POS) Codes: Using the correct POS code (e.g., 02 for telehealth provided other than in the patient’s home, 10 for telehealth provided in the patient’s home) is crucial.
- Telehealth Modifiers: As mentioned, specific modifiers (e.g., GT, GQ, 95) may be required by payers to indicate that the service was provided via telehealth.
- Payer Coverage Policies: It’s essential to verify which behavioral health services are covered via telehealth by each payer, as policies can vary.
- State Regulations: Some states have specific regulations regarding telehealth delivery, which may impact coding and billing.
By addressing these unique considerations, challenges, and the evolving landscape of telehealth, healthcare decision-makers can implement effective medical coding solutions that ensure accurate reimbursement, compliance, and ultimately, support the delivery of quality behavioral health services to those in need. Investing in specialized training, staying updated on payer rules, and leveraging technology are key strategies for success in this complex but vital area of healthcare.
Primary Care Coding Essentials
Primary care serves as the frontline of healthcare, addressing a broad spectrum of patient needs. Accurate and efficient coding in this setting is paramount for the financial stability of practices and for providing valuable data on the health of communities. Let’s break down the key elements.
Primary care encompasses a wide array of services aimed at promoting health, preventing illness, managing acute and chronic conditions, and coordinating care. Common services encountered in primary care settings include:
- Routine Check-ups and Physical Exams: These preventive visits focus on screening, health education, and early detection of potential issues.
- Acute Illness Visits: Addressing sudden onset conditions like infections, injuries, or pain.
- Chronic Disease Management: Ongoing care for conditions like diabetes, hypertension, asthma, and heart disease.
- Vaccinations and Immunizations: Administering vaccines to prevent infectious diseases.
- Screenings: Performing tests for early detection of diseases like cancer, diabetes, and high cholesterol.
- Minor Procedures: Such as wound care, injections, and simple biopsies.
- Health Education and Counselling: Providing guidance on lifestyle modifications, disease management, and mental wellness.
- Referrals and Coordination of Care: Connecting patients with specialists and ensuring seamless transitions of care.
The coding for these diverse services relies heavily on Evaluation and Management (E/M) codes, Preventive Medicine codes, and specific codes for procedures, vaccinations, and other interventions.
E/M Coding in the Primary Care Setting: Levels and Documentation
Evaluation and Management (E/M) codes are the pillars of primary care coding, representing the cognitive labor a provider expends in evaluating and managing a patient’s health. Selecting the correct E/M code (99202-99215 for office/outpatient visits for new and established patients, respectively, and other codes for different settings like hospital or nursing facility) is critical for accurate reimbursement.
- Levels of Service: E/M codes are differentiated by the level of service provided, based on the complexity of the patient’s condition and the amount of work performed by the provider. For office/outpatient visits (the most common in primary care), the key determining factors are:
- Medical Decision Making (MDM): This is now the primary factor for code selection for these visit types. MDM involves the number and complexity of problems addressed, the amount and/or complexity of data to be reviewed and analyzed, and the risk of complications and/or morbidity or mortality associated with the patient’s problem(s), the diagnostic procedure(s), and/or the management options selected.
- Total Time: For these specific office/outpatient codes, providers can also choose to code based on the total time spent on the day of the encounter, including face-to-face and non-face-to-face time (e.g., reviewing tests, preparing orders).
- Documentation: Clear and concise documentation is essential to support the level of E/M code billed. Key elements to document include:
- Chief Complaint: The patient’s primary reason for the visit.
- History: Relevant information about the present illness, past medical history, family history, and social history. The level of history documented should be pertinent to the patient’s presenting problem(s).
- Examination: A medically appropriate examination relevant to the patient’s issue(s). While the specific elements are not as prescriptive as in the past for office/outpatient visits, the documentation should clearly reflect the extent and focus of the exam.
- Medical Decision Making: The documentation should clearly articulate the complexity of the problems addressed, the data reviewed (e.g., lab results, imaging), the assessment, and the plan of care, including any alternative diagnoses considered. If coding by time, the total time spent should be documented.
- Diagnosis: The primary and any secondary diagnoses addressed during the encounter, coded using ICD-10-CM.
Preventive Medicine Services Coding
Preventive care is a cornerstone of primary care, and specific CPT codes (99381-99397 for new and established patients, categorized by age) are used to report these services.
- Scope of Preventive Services: These codes cover comprehensive preventive medicine evaluations, including a history, examination, counselling, anticipatory guidance, and risk factor reduction interventions.
- Age-Based Coding: The appropriate code is selected based on the patient’s age.
- Separate E/M for Significant Problem: If a significant and separately identifiable problem is addressed during a preventive visit, an additional E/M code (with modifier -25 appended to the E/M code) may be reported, provided the documentation supports both the preventive service and the problem-oriented visit. The problem addressed must go beyond the typical scope of a preventive service.
- Screening Tests: Many preventive visits include or result in orders for screening tests (e.g., mammograms, colonoscopies, lipid panels). These tests are coded separately using the appropriate CPT or HCPCS codes.
Vaccination and Immunization Coding
Administering vaccines is a frequent service in primary care, and coding involves both the administration of the vaccine and the vaccine product itself.
- Vaccine Administration Codes: CPT codes in the 90460-90480 range are used to report the administration of vaccines. These codes often differentiate based on the route of administration (e.g., intramuscular, subcutaneous, oral) and whether counseling was provided. There are specific codes for the first vaccine/toxoid administered and for each additional vaccine/toxoid.
- Vaccine Product Codes: The vaccines themselves are reported using specific HCPCS Level II codes (often in the ‘P’ & ‘9’ series, e.g., P2034 for influenza virus vaccine, quadrivalent).
- Documentation: Accurate documentation should include the date of administration, the name and manufacturer of the vaccine, the lot number, the route and site of administration, and any counselling provided.
Common Primary Care Diagnoses and Their ICD-10-CM Codes
Primary care encounters address a vast array of conditions. Some common diagnostic categories and examples of frequently used ICD-10-CM codes include:
- Hypertension: I10 (Essential (primary) hypertension), I11 (Hypertensive heart disease), I12 (Hypertensive chronic kidney disease). Specificity often involves the stage of hypertension and any associated organ damage.
- Diabetes Mellitus: E11 (Type 2 diabetes mellitus), E10 (Type 1 diabetes mellitus), E13 (Other specified diabetes mellitus). Codes require specification of complications (e.g., retinopathy, neuropathy, nephropathy) and control status.
- Hyperlipidemia: E78.00 (Pure hypercholesterolemia), E78.1 (Pure hyperglyceridemia), E78.5 (Hyperlipidemia, unspecified).
- Acute Respiratory Infections: J00 (Acute nasopharyngitis [common cold]), J01.XX (Acute sinusitis), J02.X (Acute pharyngitis), J03.XX (Acute tonsillitis), J20.X (Acute bronchitis). Specificity often involves the causative organism if known.
- Musculoskeletal Conditions: M54.X (Dorsalgia), M25.5XX (Pain in joint), M79.7 (Fibromyalgia). Laterality (left, right) and specific joint involvement are often required.
- Mental Health Conditions: F41.9 (Anxiety disorder, unspecified), F32.9 (Major depressive disorder, single episode, unspecified), Z71.3 (Dietary counselling and surveillance). Primary care often manages common mental health conditions or provides initial screening and referral.
- Injuries: S codes (e.g., S83.50XA Sprain of unspecified collateral ligament of right knee, initial encounter). Specificity involves the type of injury, location, laterality, and encounter status (initial, subsequent, sequela).
- Signs and Symptoms: R codes (e.g., R03.0 Elevated blood-pressure reading, without diagnosis of hypertension, R51 Headache). These are often used when a definitive diagnosis has not yet been established.
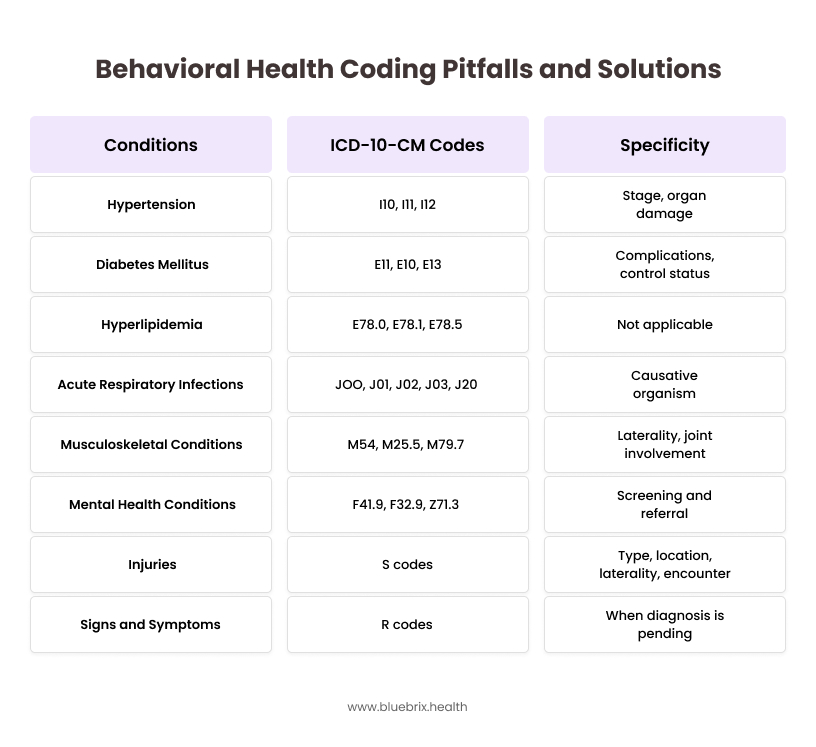
Accurate coding requires selecting the most specific ICD-10-CM code that reflects the patient’s condition based on the available documentation.
Coding for Chronic Disease Management
Managing chronic conditions is a significant part of primary care. Coding for these encounters often involves:
- E/M Codes: As the primary service for ongoing management. The level of E/M code should reflect the complexity of the patient’s condition, the number of comorbidities, the data reviewed, and the management plan.
- Chronic Condition-Specific ICD-10-CM Codes: As listed above (e.g., for diabetes, hypertension). Accurate coding often requires documenting the status and any complications of the chronic condition.
- Category II Codes: These supplemental tracking codes can be used to report data related to the management of chronic conditions, such as blood pressure control or HbA1c levels. While not directly impacting reimbursement, they can be used for quality reporting initiatives.
- Care Management Codes: For more intensive chronic care management services that involve significant non-face-to-face time (e.g., care coordination, patient education), specific CPT codes (e.g., 99490, 99491) may be applicable, provided specific requirements are met.
Referral and Consultation Coding in Primary Care
Primary care physicians often refer patients to specialists or provide consultations requested by other providers. Coding for these scenarios has specific rules:
- Referrals: When a primary care physician refers a patient to a specialist, the primary care visit is coded using an appropriate E/M code based on the services provided during that encounter. The referral itself is not a separately billable service by the referring physician.
- Consultations (Office or Other Outpatient): CPT codes for office or other outpatient consultations (99242-99245) are rarely used now by most payers, including Medicare. Typically, when a specialist sees a patient at the request of a primary care physician, the specialist bills an appropriate new or established patient E/M code. The primary care physician would bill for their own services provided to the patient.
- Interprofessional Telephone/Internet/Electronic Health Record Consultations: CPT codes (99446-99449, 99451, 99452) exist for physician-to-physician consultations that occur via phone, internet, or EHR. These codes have specific time requirements and are typically used when the primary care physician seeks advice from a specialist without the patient being seen by the specialist.
Understanding these nuances of referral and consultation coding is essential for accurate billing and avoiding confusion.
By focusing on these essential aspects of primary care coding, healthcare decision-makers can ensure their coding solutions are optimized for accuracy, efficiency, and compliance, ultimately supporting the vital role primary care plays in the US healthcare system. Investing in well-trained coding staff, staying updated on coding guidelines, and leveraging technology are key to navigating the complexities of primary care coding effectively.
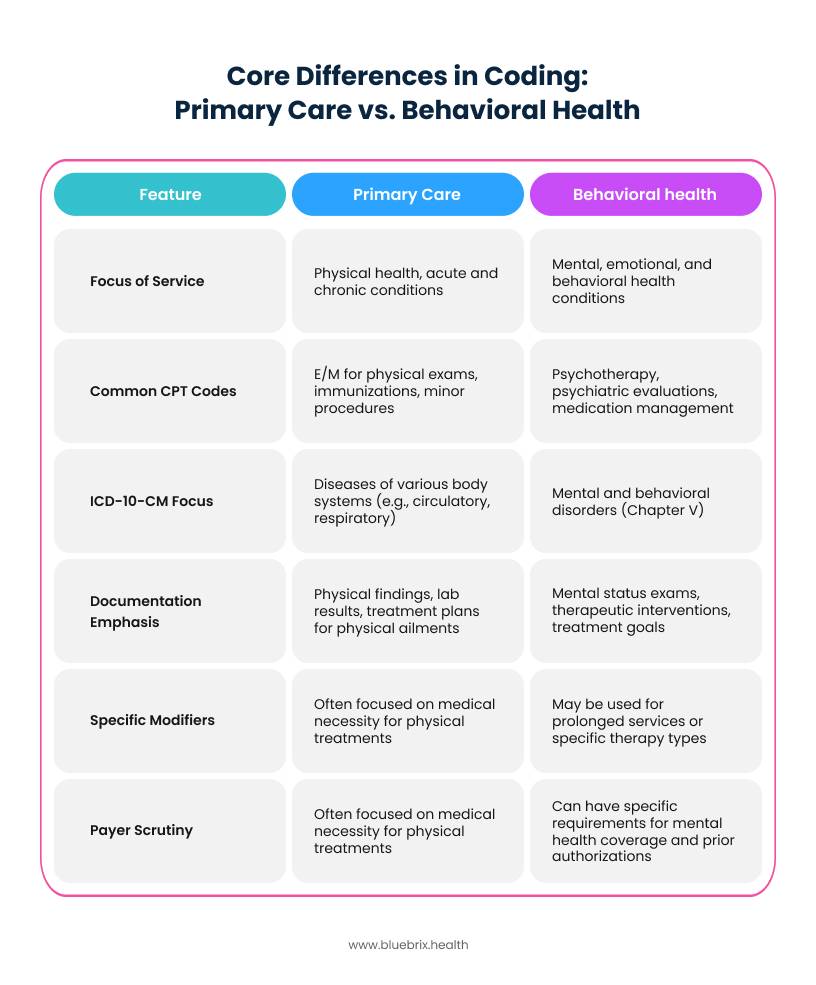
Core Differences in Coding: Primary Care vs. Behavioral Health
Coding for Emergency Department (ED) Professional and Facility Services
Navigating the intricacies of medical coding in the ED requires a nuanced understanding of both professional and facility services. Accurate coding ensures appropriate reimbursement, compliance, and efficient revenue cycle management.
Unique Considerations in ED Professional and Facility Coding
In the ED, services are bifurcated into:
- Professional Services: Rendered by physicians or qualified healthcare professionals, encompassing evaluation and management (E/M), procedures, and interpretations. For professional services, E/M levels are based on the complexity of medical decision-making.
- Facility Services: Provided by the hospital, covering the use of ED space, nursing services, supplies, and equipment. For facility services, levels are determined by resource utilization (based on ACEP guidelines).
Professional and facility services require separate coding and billing, even though they pertain to the same patient encounter.
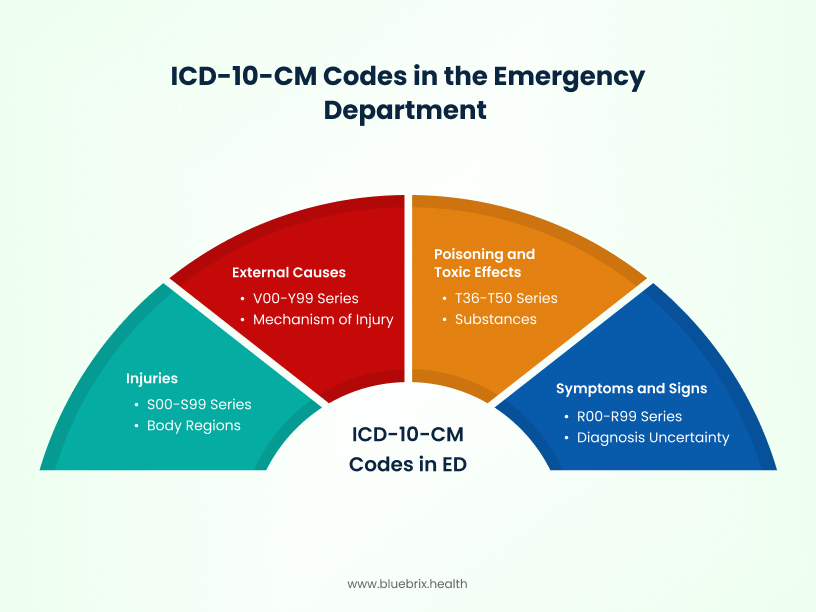
Relevant ICD-10-CM Codes in the ED
Accurate diagnosis coding is pivotal. Common ICD-10-CM codes in the ED include:
- Injuries: S00–S99 series, detailing specific body regions and injury types.
- Poisoning and Toxic Effects: T36–T50 series, specifying substances and intent.
- Symptoms and Signs: R00–R99 series, used when a definitive diagnosis isn’t established.
- External Causes: V00–Y99 series, providing context such as mechanism of injury or place of occurrence. While not nationally mandated, some payers or state programs may require these codes.
Specific CPT Codes for ED Services
Professional Services CPT codes 99281–99285 are designated for ED E/M services:
- 99281: Self-limited or minor problem.
- 99282: Low complexity.
- 99283: Moderate complexity.
- 99284: Moderate to high complexity.
- 99285: High complexity.
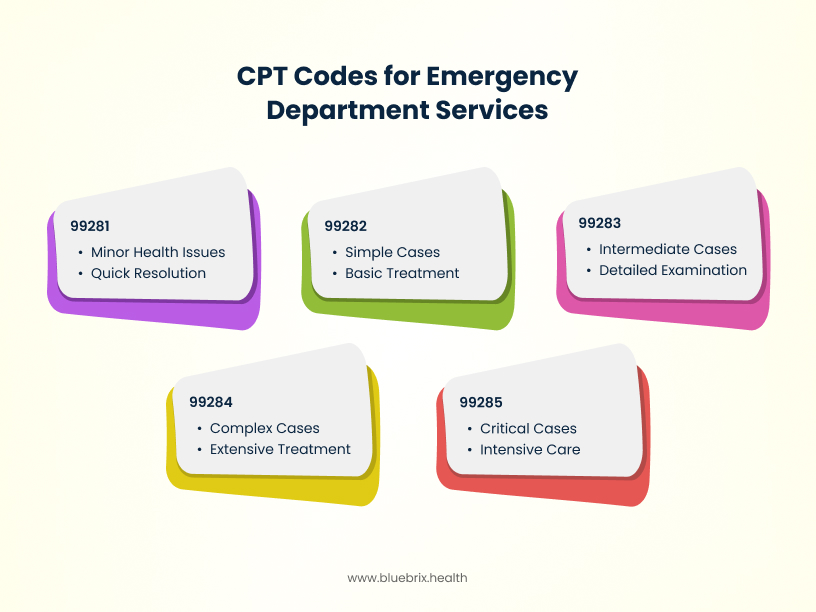
These codes are selected based on the complexity of medical decision-making, history, and examination.
Facility Services
Facility E/M levels are determined by hospital-defined guidelines, often based on resource consumption, such as diagnostics, and interventions.
Documentation Requirements for ED Professional and Facility Services
Comprehensive documentation supports code selection and compliance:
- Chief Complaint: Reason for the visit.
- History: Including history of present illness, past medical, family, and social history.
- Review of Systems: Systematic inquiry about symptoms.
- Physical Examination: Objective findings.
- Medical Decision-Making: Assessment, differential diagnoses, and plan.
- Procedures: Detailed notes on any procedures performed.
Navigating Payer-Specific Rules and Guidelines for ED Professional and Facility Services
Payer policies can vary significantly:
- Medicare: Follows CMS guidelines; for instance, during the COVID-19 Public Health Emergency, CMS allowed ED E/M codes (99281–99285) for telehealth services.
- Medicaid: Policies differ by state; it’s essential to consult state-specific guidelines.
- Private Insurers: May have unique requirements for documentation, coding, and billing. Always verify with individual payers.
Common Coding Challenges in ED Professional and Facility Services and How to Resolve Them
- Upcoding or Downcoding
Challenge: Assigning an incorrect Evaluation and Management (E/M) level—either higher (upcoding) or lower (downcoding)—can lead to compliance issues and revenue loss.
Solution: A specialized EHR can incorporate built-in coding assistance tools that analyze documentation in real-time, suggesting appropriate E/M levels based on the recorded history, examination, and medical decision-making. This ensures accurate code selection aligned with the services provided. - Incomplete Documentation
Challenge: Missing or insufficient documentation can result in claim denials and hinder continuity of care.
Solution: An ED-focused EHR can offer structured templates and prompts tailored to emergency care workflows, ensuring that all necessary information—such as chief complaints, history of present illness, and clinical findings—is thoroughly captured during the patient encounter. - Modifier Misuse
Challenge: Incorrect application of modifiers can affect reimbursement and trigger audits.
Solution: Advanced EHR systems can provide decision support by alerting users to potential modifier errors and offering guidance on correct usage based on the context of the services rendered. This proactive approach minimizes billing inaccuracies. - Telehealth Coding Confusion
Challenge: The rapid expansion of telehealth services has introduced complexities in coding, especially regarding appropriate code selection and modifier usage.
Solution: Modern EHRs can be configured to distinguish between in-person and telehealth encounters, automatically applying the correct place of service codes and modifiers (e.g., Modifier 95 for synchronous telemedicine services). This ensures compliance with payer-specific telehealth billing requirements. - Navigating Payer-Specific Rules and Guidelines
Challenge: Variations in payer policies can complicate coding and billing processes.
Solution: An intelligent EHR can integrate payer-specific rules, providing real-time alerts and guidance to ensure that documentation and coding align with individual payer requirements. This adaptability reduces claim rejections and accelerates reimbursement cycles.
Coding for Surgical Day Services (SDS)
Navigating the complexities of medical coding in Surgical Day Services (SDS) requires a nuanced understanding of both clinical procedures and administrative protocols. Accurate coding ensures appropriate reimbursement, compliance, and efficient revenue cycle management.
Unique Considerations in SDS Coding
SDS, often referred to as outpatient or same-day surgery, involves procedures that don’t require overnight hospitalization. The coding landscape here differs from inpatient settings due to:
- Procedure Complexity: SDS encompasses a wide range of procedures, from minor interventions to complex surgeries, necessitating precise code selection.
- Resource Utilization: Billing must reflect the resources used, including anesthesia, operating room time, and post-operative care.
- Bundled Payments: Many payers adopt bundled payment models for SDS, emphasizing the importance of accurate and comprehensive coding.
Relevant ICD-10-CM Codes in SDS
ICD-10-CM codes capture the patient’s diagnosis, justifying the medical necessity of the surgical procedure. Common codes in SDS include:
- M17.11: Unilateral primary osteoarthritis, right knee
- K80.20: Calculus of gallbladder without cholecystitis without obstruction
- N40.1: Benign prostatic hyperplasia with lower urinary tract symptoms
Accurate diagnosis coding is crucial for reimbursement and statistical tracking.
Specific CPT Codes for SDS Procedures
CPT codes describe the surgical procedures performed. Examples include:
- 29881: Arthroscopy, knee, surgical; with meniscectomy (medial or lateral)
- 47562: Laparoscopy, surgical; cholecystectomy
- 52235: Cystourethroscopy with fulguration of bladder tumor(s); 0.5 cm or less
Selecting the correct CPT code ensures accurate billing and reflects the services provided.
Documentation Requirements for SDS
Comprehensive documentation supports code selection and compliance:
- Preoperative Diagnosis: Initial diagnosis prompting surgery.
- Postoperative Diagnosis: Findings after the procedure.
- Procedure Details: Specifics of the surgery performed.
- Anesthesia Records: Type and duration of anesthesia used.
- Operative Report: Detailed narrative of the surgical procedure, including techniques and findings.
Accurate and detailed documentation is essential for coding, billing, and legal purposes.
Navigating Payer-Specific Rules and Guidelines for SDS Coding
Payer policies can vary significantly:
- Medicare: Follows the National Correct Coding Initiative (NCCI) edits to prevent improper payments.
- Medicaid: Policies differ by state; it’s essential to consult state-specific guidelines.
- Private Insurers: May have unique requirements for documentation, coding, and billing. Always verify with individual payers.
Staying updated with payer-specific guidelines ensures compliance and optimizes reimbursement.
Common Coding Challenges in SDS and Solutions
- Modifier Misuse: Incorrect application can lead to claim denials.
Solution: Provide clear guidelines and examples for proper modifier usage. - Incomplete Documentation: Missing elements can result in claim denials.
Solution: Implement standardized templates and thorough training. - Upcoding or Downcoding: Assigning a higher or lower CPT code than warranted.
Solution: Regular audits and provider education to ensure accurate code selection. - Payer Policy Variations: Differences in coverage and billing requirements.
Solution: Maintain a centralized database of payer-specific guidelines and updates.
Effective medical coding in Surgical Day Services is multifaceted, requiring attention to detail, adherence to guidelines, and continuous education. By understanding the nuances of SDS coding, staying abreast of updates, and implementing robust documentation practices, healthcare organizations can optimize reimbursement and maintain compliance.
Additional Considerations for SDS Coding
1. Anesthesia Coding
Anesthesia services are integral to many SDS procedures. Accurate coding requires:
- CPT Codes: Anesthesia codes (00100–01999) should reflect the specific procedure and anatomical site.
- Modifiers: Use appropriate modifiers (e.g., AA for services personally performed by an anesthesiologist, QK for medical direction of two, three, or four concurrent anesthesia procedures).
- Time Reporting: Document total anesthesia time in minutes, as many payers reimburse based on time units.
2. Pathology and Laboratory Services
Specimens collected during SDS procedures often require separate coding:
- CPT Codes: Codes 80047–89398 cover a range of laboratory and pathology services.
- Diagnosis Linking: Ensure that diagnosis codes justify the medical necessity of the tests performed.
3. Postoperative Care and Global Periods
Understanding global surgical packages is crucial:
- Global Periods: Many procedures have a 0, 10, or 90-day global period during which related postoperative care is included in the initial payment.
- Modifiers: Use modifiers like 24 (unrelated E/M service during postoperative period) or 79 (unrelated procedure during postoperative period) when appropriate.
4. Supply and Implant Coding
Accurate reporting of supplies and implants ensures appropriate reimbursement:
- HCPCS Codes: Use Level II HCPCS codes (e.g., C-codes for CMS) to report implants and certain supplies.
- Invoice Documentation: Maintain detailed records and invoices for high-cost items, as some payers require this for reimbursement.
5. Use of Modifiers for Multiple Procedures
When multiple procedures are performed:
- Modifier 51: Indicates multiple procedures performed during the same session.
- Modifier 59: Denotes distinct procedural services, used when procedures are not normally reported together but are appropriate under the circumstances.
6. Telehealth Preoperative and Postoperative Visits
With the rise of telehealth:
- Coding: Use appropriate E/M codes with telehealth modifiers (e.g., 95) for virtual visits.
- Documentation: Ensure that virtual visits are thoroughly documented, including patient consent and technology used.
7. Quality Reporting and Compliance
Participation in quality programs affects coding:
- MIPS Reporting: Accurate coding supports reporting for the Merit-based Incentive Payment System (MIPS).
- Audits: Regular internal audits help maintain compliance and identify areas for improvement.
Incorporating these additional considerations into your SDS coding practices can enhance accuracy, ensure compliance, and optimize reimbursement. Leveraging specialized EHR systems, staying updated with payer-specific guidelines, and investing in continuous staff education are pivotal steps toward achieving excellence in surgical day services coding.
Coding for Inpatient Diagnosis-Related Group (IPDRG)
Inpatient Diagnosis-Related Group coding not only influences hospital revenue but also impacts quality metrics, compliance, and operational efficiency. For healthcare decision-makers, mastering IPDRG coding is pivotal to navigating the complexities of inpatient care reimbursement.
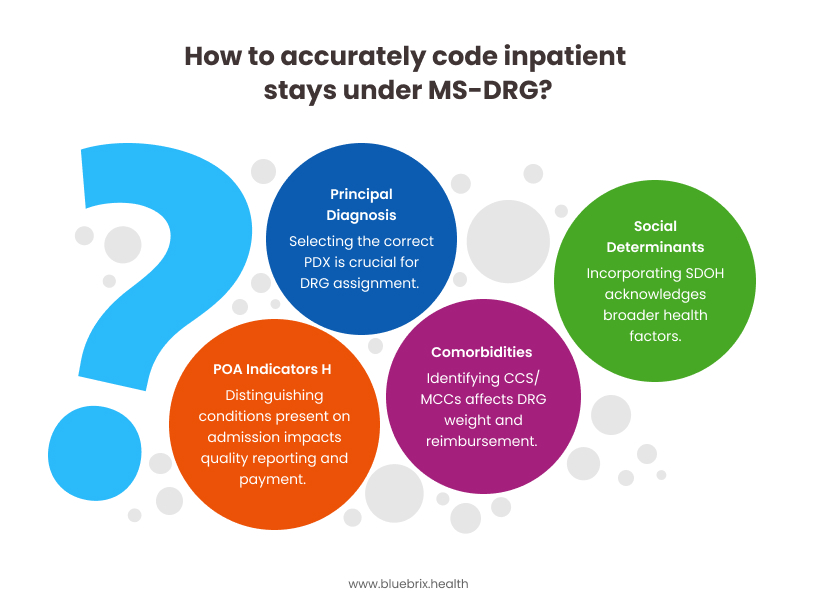
Unique Considerations in IPDRG Coding
IPDRG coding, under the Medicare Severity Diagnosis-Related Group (MS-DRG) system, classifies inpatient stays based on diagnoses, procedures, age, comorbidities, and discharge status. Key considerations include:
- Principal Diagnosis (PDx) Selection: Accurate identification of the PDx is crucial, as it determines the DRG assignment. For complex cases, such as patients with multiple comorbidities, selecting the appropriate PDx requires thorough clinical evaluation and documentation.
- Complications and Comorbidities (CC/MCC): The presence of CCs or Major CCs (MCCs) can elevate the DRG weight, affecting reimbursement.
- Present on Admission (POA) Indicators: Correctly identifying conditions present at the time of admission is essential to distinguish hospital-acquired conditions, impacting both quality reporting and payment.
- Social Determinants of Health (SDoH): Incorporating SDoH into coding practices acknowledges the broader factors influencing patient health and can affect DRG assignment.
Relevant ICD-10-CM Codes for IPDRG
ICD-10-CM codes capture the patient’s diagnoses and are foundational to DRG assignment. Common examples include:
- I50.9: Heart failure, unspecified
- E11.9: Type 2 diabetes mellitus without complications
- J18.9: Pneumonia, unspecified organism
Accurate and specific coding ensures appropriate DRG classification and reimbursement.
Specific CPT Codes in IPDRG
While CPT codes are primarily used for outpatient services, they play a role in inpatient settings, particularly for:
- Professional Services: Physician evaluations and procedures during inpatient stays.
- Ancillary Services: Radiology, pathology, and other diagnostic services.
However, inpatient facility billing predominantly utilizes ICD-10-PCS codes for procedures.
Documentation Requirements for IPDRG
Comprehensive documentation is vital for accurate IPDRG coding:
- Detailed Clinical Notes: Clear articulation of diagnoses, procedures, and patient responses.
- Operative Reports: Specifics of surgical interventions, including techniques and findings.
- Discharge Summaries: Summarization of the hospital stay, treatments provided, and patient outcomes.
Implementing Clinical Documentation Improvement (CDI) programs can enhance documentation quality, ensuring accurate DRG assignment.
Navigating Payer-Specific Rules and Guidelines for IPDRG
Different payers may have unique requirements:
- Medicare: Adheres to MS-DRG guidelines, with specific policies on POA indicators and hospital-acquired conditions.
- Medicaid: State-specific DRG systems may apply, necessitating familiarity with local regulations.
- Commercial Insurers: May use proprietary DRG systems or variations, requiring careful review of contract terms.
Staying abreast of payer-specific guidelines is essential to ensure compliance and optimize reimbursement.
Common Coding Challenges in IPDRG and How to Overcome Them
- Incorrect PDx Assignment: Misidentifying the principal diagnosis can lead to inappropriate DRG assignment.
Solution: Enhance coder training and utilize CDI specialists to validate PDx selection. - Incomplete Documentation: Lack of specificity can result in undercoding and revenue loss.
Solution: Implement structured documentation templates and regular audits. - POA Indicator Errors: Incorrect POA status can affect quality metrics and reimbursement.
Solution: Educate clinical staff on accurate POA documentation and coding. - Upcoding Risks: Assigning higher-weighted DRGs without sufficient documentation can trigger audits.
Solution: Establish internal compliance checks and promote ethical coding practices.
Other important aspects of IPDRG coding:
- Integration of Technology – Leveraging advanced coding software and Computer-Assisted Coding (CAC) systems can enhance accuracy and efficiency in DRG assignment.
- Continuous Education – Regular training sessions for coding staff on updates to ICD-10-CM/PCS codes and DRG guidelines are crucial for maintaining coding proficiency.
- Quality Reporting – Accurate DRG coding contributes to hospital quality metrics, influencing public reporting and reimbursement under value-based purchasing programs.
Mastering IPDRG coding is imperative for healthcare organizations aiming to optimize reimbursement, ensure compliance, and deliver high-quality patient care. By focusing on accurate documentation, staying informed about payer-specific guidelines, and investing in continuous education and technology, healthcare leaders can navigate the complexities of inpatient coding with confidence.
Coding for E/M Inpatient and Observation Services
Evaluation and Management (E/M) coding is pivotal in accurately capturing the complexity and resource utilization of patient encounters in inpatient and observation settings. With recent updates to coding guidelines, it’s essential to grasp the nuances that impact documentation, compliance, and reimbursement.
Unique Considerations for Inpatient and Observation Services E/M Coding
1. Merged Code Sets
As of January 1, 2023, the American Medical Association (AMA) revised the E/M codes, merging hospital inpatient and observation care services into a single code set. This consolidation aims to simplify coding and reduce redundancy.
2. Code Selection Based on MDM or Time
The level of E/M service is determined by either:
- Medical Decision Making (MDM) – Assessed based on the complexity of establishing diagnoses, the amount and complexity of data to be reviewed, and the risk of complications or morbidity.
- Total Time – Includes all time spent on the date of the encounter, encompassing both face-to-face and non-face-to-face activities.
3. Elimination of History and Exam as Key Components
While a medically appropriate history and physical examination are still necessary, they no longer influence code selection. This shift emphasizes the importance of MDM and time in determining the appropriate E/M level.
Relevant ICD-10-CM Codes for Inpatient and Observation Services E/M
ICD-10-CM codes are utilized to document diagnoses and are crucial for justifying the medical necessity of services rendered. Common codes in inpatient and observation settings include:
- I10: Essential (primary) hypertension
- E11.9: Type 2 diabetes mellitus without complications
- J18.9: Pneumonia, unspecified organism
Accurate diagnosis coding ensures appropriate DRG assignment and reimbursement.
Specific CPT Codes for Inpatient and Observation Services E/M
The consolidated E/M codes for inpatient and observation services are:
- Initial Hospital Inpatient or Observation Care: 99221–99223
- Subsequent Hospital Inpatient or Observation Care: 99231–99233
- Hospital Inpatient or Observation Care Services (Same-day Admit & Discharge Services):99234–99236
- Hospital Inpatient or Observation Discharge Day Management: 99238–99239
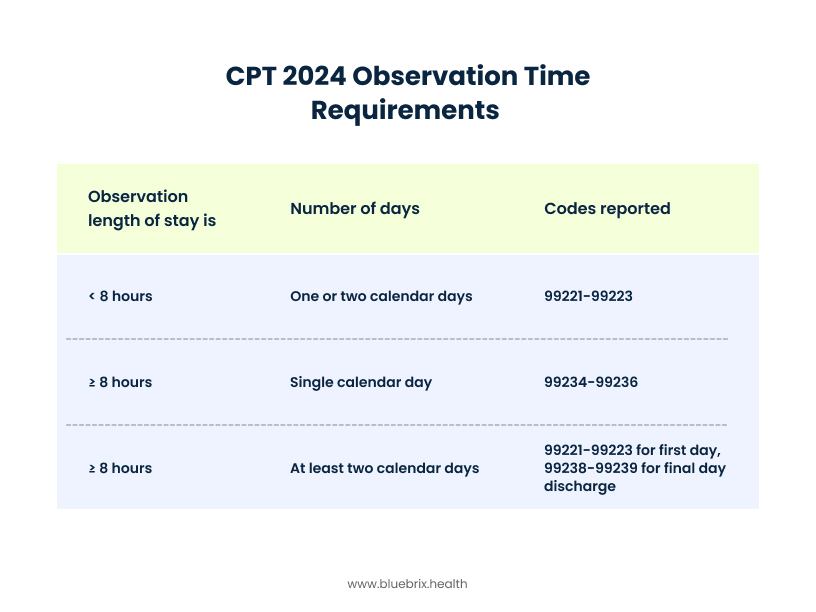
These codes are selected based on MDM complexity or total time spent on the date of the encounter.
Documentation Requirements for Inpatient and Observation Services E/M
Effective documentation is critical for accurate coding and compliance:
- Medical Necessity: Clearly articulate the reason for the encounter and the necessity of services provided.
- MDM Element: Detail the complexity of problems addressed, data reviewed, and risk assessment.
- Time Tracking: If coding based on time, document all activities performed on the date of the encounter, including non-face-to-face services.
Navigating Payer-Specific Rules and Guidelines for Inpatient and Observation Services E/M
Understanding payer-specific requirements is essential:
- Medicare: Adheres to the AMA’s revised E/M guidelines, with specific policies on prolonged services and split/shared visits.
- Commercial Payes: May have variations in adopting the revised guidelines; it’s crucial to verify individual payer policies.
Staying informed about these nuances ensures compliance and optimal reimbursement.
Common Coding Challenges and Solutions in Inpatient and Observation Services E/M
Distinguishing Between Inpatient and Observation Stats
Challenge: Misclassification can lead to incorrect coding and reimbursement issues.
Solution: Ensure clear documentation of the patient’s status and apply the appropriate E/M codes.
Accurate Time Documentation
Challenge: Incomplete or inaccurate time tracking can result in incorrect code selection.
Solution: Implement standardized time-tracking protocols within EHR systems to capture all relevant activities on the date of service.
Understanding MDM Complexity
Challenge: Misjudging the complexity level can lead to undercoding or overcoding.
Solution: Provide ongoing training for providers and coders on MDM criteria and utilize decision-support tools within EHRs.
Additional Considerations
Split/Shared Visits
In scenarios where both a physician and a non-physician practitioner (NPP) provide care, the visit is considered split/hired. As of 2024, the “substantive portion” of the visit is defined as more than half of the total time spent, determining who reports the service.
Prolonged Servies
For encounters exceeding the typical time, prolonged service codes (e.g., G0316–G0318) may be reported in addition to the primary E/M code. Documentation must support the extended time and medical necessity.
Leveraging Technology for Enhanced Coding Accuracy for Inpatient and Observation Services E/M
Implementing purpose-built Electronic Health Record (EHR) systems can significantly improve coding accuracy and efficiency:
- Automated Time Tracing: EHRs can capture and calculate total time spent on patient care activities, facilitating accurate time-based coding.
- MDM Support Tools: Integrated decision-support features assist providers in assessing MDM complexity, ensuring appropriate code selection.
- Compliance Alerts: Real-time prompts within EHRs can flag potential documentation deficiencies or coding errors, reducing audit risks.
Navigating the complexities of E/M coding for inpatient and observation services requires a thorough understanding of updated guidelines, meticulous documentation, and awareness of payer-specific nances. By addressing common challenges and leveraging advanced EHR functionalities, healthcare leaders can drive coding accuracy, ensure compliance, and enhance financial performance.
Coding for Recurring Medical Services
Recurring medical services refer to treatments or procedures provided to patients on a regular basis, such as weekly physical therapy sessions, monthly chemotherapy, or routine dialysis. Accurate coding for these services is essential to ensure proper reimbursement and maintain compliance with payer guidelines.
Unique Considerations for Recurring Medical Services Coding
1. Frequency and Duration
Unlike one-time services, recurring treatments require meticulous tracking of frequency and duration. Each session must be documented separately, even if the procedure remains consistent.
2. Medical Necessity
Payers often scrutinize recurring services to confirm ongoing medical necessity. Comprehensive documentation supporting the need for continued treatment is crucial.
3. Authorization Requirements
Many insurers mandate prior authorization for recurring service. Failure to obtain or renew authorizations can lead to claim denial.
Relevant ICD-10-CM Codes for Recurring Medical Services
ICD-10-CM codes are used to represent diagnoses justifying the need for recurring services Examples include:
- Z51.11: Encounter for antineoplastic chemotherapy
- Z51.81: Encounter for therapeutic drug monitoring
- Z79.899: Other long-term (current) drug therapy
Accurate diagnosis coding ensures that the medical necessity for recurring services is clearly communicated to payers.
Specific CPT Codes for Recurring Medical Services
CPT codes for recurring services vary based on the type of treatment:
- Physical Therapy: 97110 (Therapeutic exercises), 97112 (Neuromuscular reeducation)
- Chemotherapy: 96413 (Chemotherapy administration, intravenous infusion technique; up to 1 hour)
- Dialysis: 90935 (Hemodialysis procedure with single physician evaluation)
Each session should be coded individually, reflecting the specific services rendered during that encounter.
Documentation Requirements for Recurring Medical Services
Thorough documentation is paramount for recurring services:
- Individual Session Note: Detailing the services provided, patient response, and any changes in treatment pans.
- Progress Report: Periodic summaries demonstrating patient progress and ongoing need for services.
- Authorization Record: Maintaining up-to-date prior authorization approvals as required by payers.
Implementing a purpose-built Electronic Health Record (EHR) system can streamline documentation processes, ensuring consistency and compliance.
Navigating Payer-Specific Rules and Guidelines for Recurring Medical Services
Payers may have unique requirements for recurring services:
- Authorization Renewals: Some insurers require periodic reauthorization for ongoing treatments.
- Utilization Limits: Limits on the number of covered sessions within a specific timeframe.
- Documentation Standards: Specific documentation elements needed to support medical necessity.
Staying informed about individual payer policies and integrating alerts within EHR systems can aid in compliance.
Common Coding Challenges in Recurring Medical Services and Solutions
Overlooking Session Documentation
Challenge: Failing to document each session separately can lead to denials.
Solution: Utilize EHR templates that prompt for session-specific details, ensuring comprehensive records.
Authorization Lapses
Challenge: Missing authorization renewals can result in unpaid claims.
Solution: Implement tracking systems within the EHR to monitor authorization statuses and alert staff of upcoming expirations.
Inconsistent Coding Practices
Challenge: Variability in coding can cause billing errors.
Solution: Standardize coding protocols and provide regular training to coding staff to maintain consistency.
Bundled Payments and Value-Based Care for Recurring Medical Services
With the shift towards value-based care, understanding how recurring services fit into bundled payment models is essential. Accurate coding and documentation support appropriate reimbursement under these models.
Telehealth Integration in Recurring Medical Services
For services delivered via telehealth, ensure the use of appropriate modifiers (e.g., 95 for synchronous telemedicine services) and adherence to payer-specific telehealth policies.
Leveraging Technology for Enhanced Coding Accuracy in Recurring Medical Services
Adopting advanced EHR systems can significantly improve the management of recurring services:
- Automated Reminders: Alerts for upcoming authorization renewals and documentation requirements.
- Integrated Coding Tools: Real-time coding assistance to ensure accurate CPT and ICD-10-CM code selection.
- Analytics and Reporting: Monitoring utilization patterns and identifying areas for improvement.
These technological solutions can enhance efficiency, reduce errors, and support compliance efforts.
Effective coding for recurring medical services is a complex but manageable aspect of healthcare administration. By understanding unique considerations, adhering to documentation requirements, navigating payer guidelines, and leveraging technology, healthcare organizations can optimize reimbursement and maintain compliance.
E/M Coding for Office and Other Outpatient (OP) Services
E/M Coding for Office and Other Outpatient (OP) Services
Evaluation and Management (E/M) coding for outpatient services encompasses the documentation and billing of patient encounters in settings such as physician offices, outpatient clinics, and urgent care centers. Accurate E/M coding is crucial for appropriate reimbursement and compliance with payer guidelines.
Unique Considerations for E/M OP Coding
- Patient Status: Differentiate between new and established patients, as coding requirements vary.
- Service Setting: Ensure the service location aligns with outpatient criteria.
- Time-Based Coding: Consider total time spent on the date of the encounter, including face-to-face and non-face-to-face activities, when selecting time-based codes.
- Medical Decision Making (MDM): Assess the complexity of MDM, which includes the number and complexity of problems addressed, data reviewed, and risk of complications.
Relevant ICD-10-CM Codes for E/M OP
ICD-10-CM codes document the patient’s diagnoses and are essential for justifying medical necessity. Common categories include:
- Z00–Z99: Factors influencing health status and contact with health services (e.g., Z00.00 – Encounter for general adult medical examination without abnormal findings).
- I10–I15: Hypertensive diseases (e.g., I10 – Essential (primary) hypertension).
- E11: Type 2 diabetes mellitus (e.g., E11.9 – Type 2 diabetes mellitus without complications).
- F32: Major depressive disorder (e.g., F32.9 – Major depressive disorder, single episode, unspecified).
Select the most specific code available to accurately represent the patient’s condition.
Specific CPT Codes for E/M OP
CPT codes for office and other outpatient E/M services are divided between new and established patients:
New Patients:
- 99202: Straightforward MDM; 15–29 minutes.
- 99203: Low complexity MDM; 30–44 minutes.
- 99204: Moderate complexity MDM; 45–59 minutes.
- 99205: High complexity MDM; 60–74 minutes.
Established Patients:
- 99211: Minimal problems; typically 5 minutes.
- 99212: Straightforward MDM; 10–19 minutes.
- 99213: Low complexity MDM; 20–29 minutes.
- 99214: Moderate complexity MDM; 30–39 minutes.
- 99215: High complexity MDM; 40–54 minutes.
For visits exceeding these times, consider add-on codes:
- +99417: Prolonged office or other outpatient E/M service(s) beyond the minimum required time.
- G2212: Medicare-specific code for prolonged services.
- Additionally, G2211 is an add-on code for office or other outpatient E/M visits that serve as the continuing focal point for all needed health care services.
Documentation Requirements for E/M OP
Effective January 1, 2021, documentation for E/M services focuses on:
- Medical Decision Making (MDM): Document the complexity based on the number and complexity of problems addressed, data reviewed, and risk of complications.
- Time: Record total time spent on the date of the encounter, including both face-to-face and non-face-to-face activities.
History and physical examination components are no longer key factors in code selection but should be documented as medically appropriate.
Navigating Payer-Specific Rules and Guidelines for E/M OP
Payer policies can vary significantly:
- Medicare: Adheres to AMA guidelines but may have specific requirements for certain codes (e.g., G2211, G2212).
- Private Insurers: May have unique documentation requirements or limitations on code usage.
It’s essential to verify payer-specific policies to ensure compliance and proper reimbursement.
Common Coding Challenges in E/M OP and How to Overcome Them
Code Selection
Challenge: Inaccurate code selection due to misunderstanding of MDM or time-based criteria.
Solution: Provide ongoing education and training for coding staff to stay current with guidelines.
Denials due to Downcoding
Challenge: Incomplete or insufficient documentation leading to downcoding or denials.
Solution: Implement thorough documentation practices and regular audits to ensure completeness.
Compliance Complexities
Challenge: Navigating varying payer requirements and staying compliant.
Solution: Maintain an up-to-date repository of payer policies and conduct regular reviews.
Accurate E/M coding for outpatient services is vital for ensuring appropriate reimbursement and maintaining compliance. By understanding the nuances of coding guidelines, documentation requirements, and payer-specific rules, healthcare providers can enhance their revenue cycle efficiency and reduce the risk of claim denials.
Coding for Ancillary Services
Ancillary services encompass a broad range of supportive healthcare services, including laboratory tests, imaging, physical therapy, and more. Accurate coding of these services is vital for appropriate reimbursement and compliance with payer guidelines.
Unique Considerations for Ancillary Services
- Service Diversity: Ancillary services cover various domains such as radiology, pathology, and rehabilitation, each with specific coding requirements.
- Integration with Primary Services: These services often support primary care, necessitating precise linkage in documentation and coding.
- Regulatory Compliance: Adherence to guidelines like the National Correct Coding Initiative (NCCI) edits is crucial to prevent claim denials.
Relevant ICD-10-CM Codes for Ancillary Services
ICD-10-CM codes are used to represent diagnoses and reasons for ancillary services. Common examples include:
- Z00.00: Encounter for general adult medical examination without abnormal findings.
- R79.89: Other specified abnormal findings of blood chemistry.
- M54.50: Low back pain, often used in physical therapy services.
Selecting the most specific and accurate diagnosis code is essential to justify the medical necessity of the ancillary service.
Specific CPT Codes for Ancillary Services
Current Procedural Terminology (CPT) codes describe the procedures and services provided. Examples pertinent to ancillary services include:
- 80050: General health panel, encompassing multiple laboratory tests.
- 93000: Electrocardiogram, routine ECG with at least 12 leads; with interpretation and report.
- 97010: Application of a modality to one or more areas; hot or cold packs.
- Accurate CPT coding ensures proper billing and reimbursement for the services rendered.
Documentation Requirements for Ancillary Services
Proper documentation is critical for supporting the medical necessity and facilitating accurate coding. Key elements include:
- Physician Orders: Clear and specific orders for the ancillary service.
- Service Details: Date, time, and nature of the service provided.
- Results and Interpretation: Findings from the service and their clinical interpretation.
Comprehensive documentation aids in justifying the service and defending against potential audits.
Navigating Payer-Specific Rules and Guidelines for Ancillary Services
Different payers may have unique requirements for ancillary services. Considerations include:
- Coverage Policies: Understanding what services are covered under specific plans.
- Preauthorization Requirements: Some services may require prior approval.
- Billing Protocols: Adhering to specific billing formats or electronic submission standards.
Staying informed about payer-specific guidelines helps in reducing claim denials and ensuring timely reimbursement.
Coding for Clinical Services
Clinical services encompass a broad range of patient care activities provided by healthcare professionals, including physicians, nurses, and allied health providers. Accurate medical coding of these services is essential for appropriate reimbursement, compliance with payer guidelines, and effective revenue cycle management.
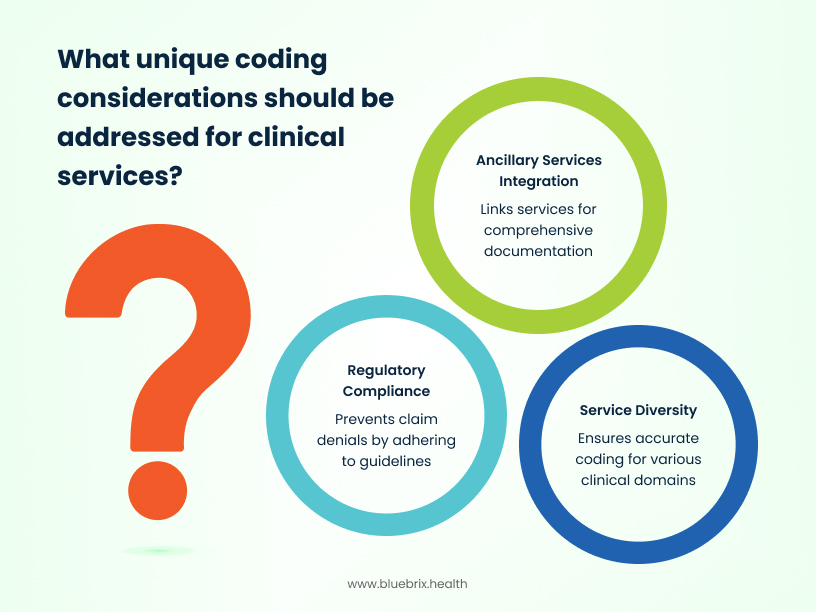
Unique Considerations for Clinical Services
- Service Diversity: Clinical services cover various domains such as primary care, specialty consultations, and preventive services, each with specific coding requirements.
- Integration with Ancillary Services: These services often support or are supported by ancillary services, necessitating precise linkage in documentation and coding.
- Regulatory Compliance: Adherence to guidelines like the National Correct Coding Initiative (NCCI) edits is crucial to prevent claim denials.
Relevant ICD-10-CM Codes for Clinical Services
ICD-10-CM codes are used to represent diagnoses and reasons for clinical services. Common examples include:
- Z00.00: Encounter for general adult medical examination without abnormal findings.
- R79.89: Other specified abnormal findings of blood chemistry.
- M54.5: Low back pain, often used in physical therapy services.
Selecting the most specific and accurate diagnosis code is essential to justify the medical necessity of the clinical service.
Specific CPT Codes for Clinical Services
Current Procedural Terminology (CPT) codes describe the procedures and services provided. Examples pertinent to clinical services include:
- 99201–99215: Office or other outpatient visits for evaluation and management.
- 99381–99397: Preventive medicine services for new and established patients.
- 99401–99404: Preventive medicine counselling and/or risk factor reduction interventions.
Accurate CPT coding ensures proper billing and reimbursement for the services rendered.
Documentation Requirements for Clinical Services
Proper documentation is critical for supporting the medical necessity and facilitating accurate coding. Key elements include:
- Patient History: Comprehensive recording of the patient’s medical, family, and social history.
- Physical Examination: Detailed findings from the physical assessment.
- Assessment and Plan: Clinical impressions and the planned course of action.
Comprehensive documentation aids in justifying the service and defending against potential audits.
Navigating Payer-Specific Rules and Guidelines for Clinical Services
Different payers may have unique requirements for clinical services. Considerations include:
- Coverage Policies: Understanding what services are covered under specific plans.
- Preauthorization Requirements: Some services may require prior approval.
- Billing Protocols: Adhering to specific billing formats or electronic submission standards.
Staying informed about payer-specific guidelines helps in reducing claim denials and ensuring timely reimbursement.
Coding in Different Healthcare Models
For healthcare decision-makers navigating the shift from traditional payment structures to value-based care, understanding how coding practices adapt and evolve is essential for financial stability, quality reporting, and overall success. The way healthcare services are paid for significantly influences how medical coding is approached and its strategic importance. The US healthcare system currently operates under a mix of payment models, with Fee-for-Service (FFS) and Value-Based Care (VBC) being the most prominent. Each model has distinct implications for coding practices and the role of accurate and comprehensive data.
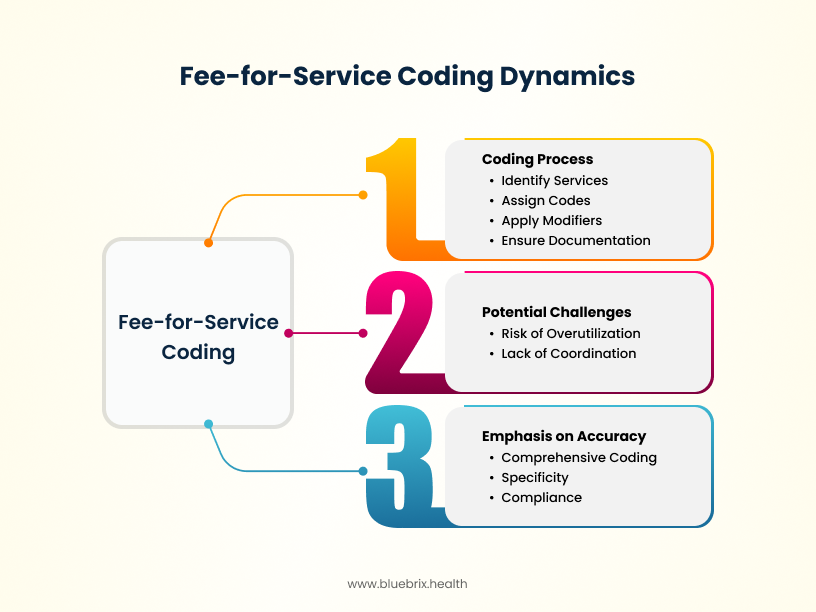
Fee-for-Service (FFS) Coding: The Traditional Approach
For decades, Fee-for-Service (FFS) has been a dominant payment model in US healthcare. Understanding its coding dynamics is crucial, even as the industry moves towards value-based models.
How FFS Coding Works: Payment per Service Rendered
In a FFS model, healthcare providers are paid a set fee for each individual service, procedure, or item they provide. This includes physician visits, tests, surgeries, and supplies. The more services rendered, the higher the reimbursement. Coding in this model directly translates the volume and complexity of these services into billable codes using ICD-10-CM for diagnoses, CPT for procedures, and HCPCS for supplies and other services.
Emphasis on Accurate and Detailed Coding to Maximize Reimbursement
Under FFS, the primary financial incentive for providers is tied to the quantity and complexity of services delivered and, consequently, accurately coded. Therefore, there’s a strong emphasis on:
- Comprehensive Coding: Ensuring all billable services are captured and coded.
- Specificity: Using the most detailed and accurate codes to reflect the level of service provided, as this often correlates with higher reimbursement.
- Compliance: Adhering to payer rules and regulations to avoid claim denials and audits.
Coding for Individual Procedures and Encounters
FFS coding focuses on the discrete healthcare encounter or procedure. Each patient visit, each diagnostic test, and each surgical intervention is coded individually. The coding process involves:
- Identifying all services performed and the diagnoses that justify them.
- Assigning the appropriate ICD-10-CM, CPT, and HCPCS codes.
- Applying relevant modifiers to provide additional context about the service.
- Ensuring documentation fully supports the codes submitted.
Potential Challenges: Risk of Overutilization and Lack of Coordination
While FFS has been the standard, it inherently carries certain challenges that coding practices can sometimes reflect:
- Risk of Overutilization: The payment-per-service model can incentivize providers to perform more services than strictly necessary, potentially leading to higher healthcare costs without necessarily improving patient outcomes. Coding accurately for all rendered services, even if questions of necessity arise, is still the primary directive under FFS.
- Lack of Coordination: FFS doesn’t always incentivize seamless care coordination between different providers or settings. Coding for individual encounters may not fully capture the holistic patient journey or the efforts involved in care coordination.
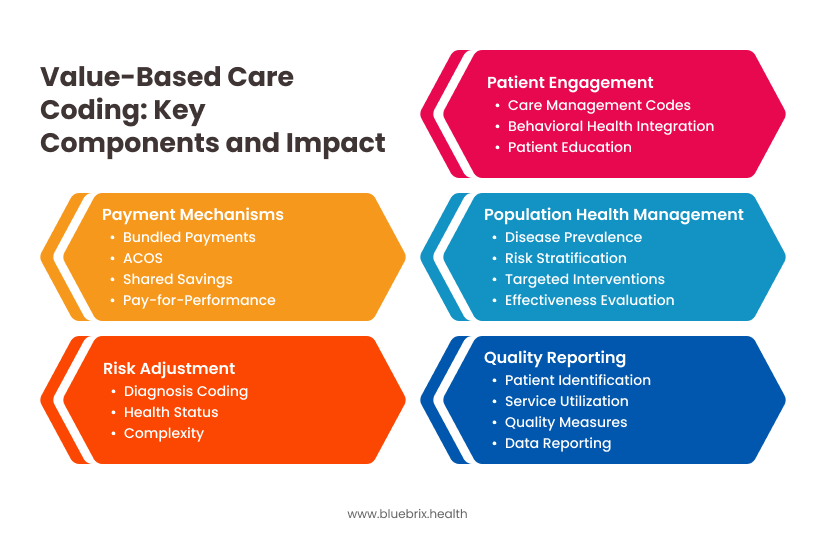
Value-Based Care (VBC) Coding: Shifting the Paradigm
Value-Based Care (VBC) models represent a fundamental shift in how healthcare is paid for, moving away from volume-based reimbursement towards payments tied to the quality and outcomes of care. This transition has significant implications for medical coding.
Shifting Focus: Quality, Outcomes, and Cost-Efficiency
Value Based Care models aim to incentivize providers to deliver high-quality care, improve patient outcomes, and manage costs effectively. Payment mechanisms in Value Based Care can include:
- Bundled Payments: A single payment for an episode of care, covering multiple services.
- Accountable Care Organizations (ACOs): Groups of providers accountable for the overall cost and quality of care for a defined patient population.
- Shared Savings Models: Providers share in any cost savings achieved while meeting quality benchmarks.
- Pay-for-Performance (P4P): Incentives based on meeting specific quality metrics.
The Role of Coding in Quality Reporting and Performance Measurement
In Value Based Care, coding becomes a critical tool for capturing the data needed for quality reporting and performance measurement. Accurate and detailed coding is essential for:
- Identifying patient populations and their health status.
- Tracking the utilization of specific services and interventions.
- Capturing data on quality measures (e.g., use of preventive services, management of chronic conditions).
- Reporting required data to payers and regulatory bodies (e.g., through the Merit-based Incentive Payment System [MIPS] or within ACO frameworks).
Importance of Accurate Diagnosis Coding for Risk Adjustment
Risk adjustment is a key component of many Value Based Care models. It involves adjusting payments based on the health status and complexity of the patient population being served. Accurate and comprehensive diagnosis coding (ICD-10-CM) is paramount for effective risk adjustment. By thoroughly documenting all relevant patient conditions, providers ensure they are appropriately compensated for managing sicker and more complex patients. This prevents providers caring for high-risk populations from being unfairly penalized in value-based arrangements.
Coding for Patient Engagement and Care Coordination Activities
Value Based Care emphasizes patient engagement and care coordination as crucial elements of high-quality, cost-effective care. Coding is evolving to capture these activities:
- Care Management Codes (e.g., CCM, TCM): CPT codes exist to bill for chronic care management (CCM) and transitional care management (TCM) services, which involve significant non-face-to-face care coordination and patient support. Accurate coding requires meeting specific time and service requirements.
- Behavioral Health Integration (BHI) Codes: As mental and physical health are increasingly recognized as interconnected, codes for integrating behavioral health services into primary care settings are becoming more important. These codes capture collaborative care and psychiatric consultative services.
- Patient Education and Counseling: While often bundled into E/M services, detailed documentation of patient education and counseling can support the overall value narrative.
How Coding Supports Population Health Management
Value Based Care inherently focuses on managing the health of a defined population. Accurate and consistent coding across that population provides valuable data for:
- Identifying trends in disease prevalence and healthcare utilization.
- Stratifying patients based on risk and needs.
- Developing targeted interventions and programs to improve population health outcomes.
- Evaluating the effectiveness of population health initiatives.
Challenges and Opportunities in Value Based Care Coding
The shift to Value Based Care presents both challenges and opportunities for medical coding:
- Complexity
- Challenges: Requires understanding of quality metrics and reporting requirements; involves risk adjustment methodologies and accurate diagnosis coding; incorporates coding for care coordination and patient engagement activities.
- Opportunities: Drives a more holistic view of patient care beyond individual encounters; enhances the strategic importance of coding within the healthcare organization; creates opportunities for coders to develop new, valuable skill sets.
- Data
- Challenges: Integrating coding data with quality, outcome, and cost data can be complex; ensuring data accuracy and consistency across patient populations; extracting and reporting data for various Value Based Care programs (e.g., MIPS, ACOs).
- Opportunities: Improves the overall quality and completeness of clinical documentation and coding; provides richer data for population health management and targeted interventions; enables better measurement of care quality and patient outcomes.
- Provider Engagement
- Challenges: Educating providers on the importance of detailed documentation for Value Based Care; aligning provider documentation habits with Value Based Care coding needs.
- Opportunities: Fosters greater collaboration between clinical and coding teams to achieve shared goals; highlights the direct impact of accurate documentation on reimbursement and performance.
- Evolving Landscape
- Challenges: Value Based Care coding rules and reporting requirements are still developing; keeping up with frequent changes in Value Based Care program guidelines.
- Opportunities: Allows organizations to be at the forefront of innovative payment models; can lead to more sustainable and value-driven healthcare delivery.
- Financial Impact
- Challenges: Potential for financial penalties if quality and performance targets aren’t met; risk of inaccurate risk adjustment leading to underpayment.
- Opportunities: Opportunity for increased revenue through shared savings and performance-based incentives; accurate coding supports appropriate reimbursement for managing complex patient populations.
As the US healthcare system continues its transition towards value-based care, the role of medical coding is evolving from a purely transactional function to a strategic asset. Understanding how coding supports quality reporting, risk adjustment, patient engagement, and population health management is paramount for success in these new payment models. Investing in coding expertise that goes beyond traditional FFS coding, embracing data analytics, and fostering strong collaboration between clinical and coding teams will be essential for navigating the complexities and capitalizing on the opportunities presented by value-based care.
The Medical Coding Workflow: A Step-by-Step Guide to Reimbursement
The medical coding workflow is a series of interconnected steps that transform patient encounters into billable claims. Each stage is critical, and accuracy at every point is paramount to ensure timely and appropriate reimbursement.
Patient Encounter and Documentation: The Foundation
The entire reimbursement process begins with the patient encounter. This can take various forms, from an office visit to a surgical procedure or a telehealth consultation. The linchpin of accurate coding and subsequent reimbursement is the documentation generated during this encounter by the healthcare provider (physician, nurse practitioner, therapist, etc.).
Key Elements of Quality Documentation:
- Legibility and Clarity: Notes must be easily understandable. Electronic Health Records (EHRs) have largely addressed legibility issues but clarity in language and detail remains crucial.
- Completeness: All relevant information about the patient’s condition, the services provided, and the plan of care must be documented. This includes the chief complaint, history of present illness, past medical history, physical exam findings, diagnostic tests ordered and reviewed, procedures performed, medications prescribed, and patient instructions.
- Specificity: The documentation should use precise medical terminology to accurately reflect the patient’s condition and the services rendered. Vague or ambiguous terms can lead to coding errors.
- Timeliness: Documentation should be completed promptly after the encounter to ensure accuracy and recall of details.
- Authentication: All entries must be signed and dated by the rendering provider.
Impact on Coding
The level of detail and clarity in the documentation directly dictates the coder’s ability to assign the most accurate and specific ICD-10-CM, CPT, and HCPCS codes. Poor documentation is the single biggest contributor to coding errors and subsequent claim issues.
Abstracting Relevant Information for Coding: Translating Clinical Notes
Once the patient encounter is documented, the next step is abstracting the key information needed for coding. This is where skilled medical coders come into play. They meticulously review the clinical documentation to identify:
- Diagnoses: The patient’s medical conditions, illnesses, injuries, or reasons for the encounter. This information will be translated into ICD-10-CM codes.
- Procedures and Services: The medical interventions, treatments, tests, and evaluations performed during the encounter. These will be translated into CPT and HCPCS codes.
- Supplies and Equipment: Any durable medical equipment, prosthetics, orthotics, supplies (DMEPOS), or medications administered or provided. These are typically coded using HCPCS Level II codes.
- Level of Service: For Evaluation and Management (E/M) codes, the coder will assess the complexity of the patient’s condition and the extent of the history, examination, and medical decision-making documented.
- Modifiers: The coder will look for any circumstances that require the use of modifiers to provide additional information about the service or procedure (e.g., if a procedure was performed bilaterally, if multiple procedures were performed, or if a service was reduced).
Tools and Techniques: Coders may use various tools for abstraction, including:
- EHR Systems: Many EHRs have features that facilitate coding, such as integrated code look-up tools and the ability to link diagnoses to procedures.
- Coding Software: Specialized software can assist with code selection based on keywords and documentation analysis.
- Manual Review: In some cases, especially for complex or ambiguous documentation, manual review and interpretation of the medical record are necessary.
Assigning ICD-10-CM, CPT, and HCPCS Codes: The Core of the Process
This is the heart of the medical coding workflow. Based on the abstracted information, the coder assigns the appropriate alphanumeric codes using the three main coding systems:
- ICD-10-CM: The coder must select the most specific code that accurately reflects the patient’s condition as documented. This often involves navigating the Alphabetic Index and Tabular List of the ICD-10-CM codebook and adhering to coding guidelines.
- CPT: Coders must carefully read the descriptions of CPT codes to ensure they accurately match the services documented. Understanding the different categories of CPT codes (Category I, II, and III) and the use of modifiers is crucial.
- HCPCS: Level I of HCPCS is the CPT system. Level II (National Codes) are used to report services, supplies, and equipment not covered by CPT, such as DME, drugs, and ambulance services. Coders need to be familiar with the HCPCS Level II codebook and any relevant payer-specific guidelines.
Accuracy and Compliance
At this stage, accuracy is paramount. Incorrect code assignment can lead to claim denials, underpayment, or even allegations of fraud and abuse. Coders must adhere to official coding guidelines, payer policies, and legal regulations.
Reviewing and Auditing Codes for Accuracy: Ensuring Quality
Before a claim is submitted, it’s essential to review and audit the assigned codes to identify and correct any errors. This step helps ensure the accuracy and compliance of the billing process.
- Internal Audits: Healthcare organizations should implement internal audit processes where coding is reviewed by other qualified coders or coding auditors. This can be done on a regular basis or targeted at specific providers, services, or high-risk areas.
- Coding Software Edits: Many coding software programs have built-in edits that flag potential coding errors or inconsistencies. These edits can help catch issues before claims are submitted.
- Comparison to Documentation: Auditors will compare the assigned codes to the underlying medical documentation to ensure they are supported and accurately reflect the services provided and the patient’s diagnoses.
- Compliance Checks: Audits should also assess compliance with coding guidelines, payer policies, and regulatory requirements.
Benefits of Auditing
Regular coding audits can:
- Reduce claim denials and rework.
- Improve the accuracy of reimbursement.
- Identify areas for coder training and education.
- Mitigate the risk of compliance issues.
- Provide valuable feedback to providers on documentation practices.
Claim Submission and the Billing Process: Sending the Bill
Once the coding is reviewed and deemed accurate, the claim is prepared and submitted to the appropriate payer (e.g., insurance company, Medicare, Medicaid). This is typically done electronically using standardized formats, as mandated by HIPAA.
- Claim Generation: Billing departments or practice management systems generate electronic claims based on the coded data and patient demographics.
- EDI (Electronic Data Interchange): Claims are transmitted electronically to payers through secure EDI channels.
- Claim Scrubbing: Before submission, claims often undergo a “scrubbing” process, either within the billing software or through a clearinghouse, to identify and correct any formatting errors or missing information that could lead to rejection.
- Payer Processing: Payers receive the electronic claims and process them according to their specific rules, coverage policies, and fee schedules.
Understanding Explanation of Benefits (EOBs) and Remittance Advice (RAs): Decoding Payer Responses
After processing a claim, the payer sends a response to the healthcare provider. This response is typically in the form of an Explanation of Benefits (EOB) for patients (outlining what was billed, what the payer paid, and any patient responsibility) and a Remittance Advice (RA) or Electronic Remittance Advice (ERA) for providers.
- Remittance Advice (RA/ERA): This document details the payer’s payment decisions for each claim submitted. It includes:
- Payment Amounts: The amount the payer is paying for each service.
- Denial Reasons: If a service was not paid, the RA will provide a reason code explaining the denial.
- Adjustments: Any adjustments made to the billed charges (e.g., due to contractual agreements).
- Patient Responsibility: The amount the patient may owe (e.g., copay, deductible, coinsurance).
- Analysis of RAs/ERAs: The billing department must carefully review RAs/ERAs to understand why claims were paid, underpaid, or denied. This analysis is crucial for identifying coding errors, payer issues, or the need for appeals.
Handling Denials and Appeals: Addressing Payment Issues
Claim denials are a reality in the reimbursement process. A robust system for handling denials and appeals is essential to maximize revenue and identify systemic issues.
- Identifying Denial Reasons: The first step is to understand the specific reason for the denial as indicated on the RA. Common reasons include:
- Coding Errors: Incorrect, incomplete, or non-specific codes.
- Lack of Medical Necessity: The payer determines the service was not medically necessary based on the diagnosis.
- Documentation Issues: Insufficient or missing documentation to support the billed services.
- Coverage Issues: The service is not covered under the patient’s plan.
- Authorization Issues: Required prior authorization was not obtained.
- Billing Errors: Incorrect patient information, missing provider information, etc.
- Investigating and Correcting Errors: Once the reason for denial is identified, the appropriate action must be taken. This may involve:
- Reviewing the medical documentation and coding.
- Correcting coding errors and resubmitting the claim.
- Obtaining missing documentation or authorizations.
- Verifying patient eligibility and coverage.
- The Appeals Process: If the denial is believed to be incorrect after investigation, the healthcare provider has the right to appeal the payer’s decision. The appeals process varies by payer but typically involves submitting a written appeal with supporting documentation explaining why the claim should be paid. There are often deadlines for filing appeals.
Optimizing the Workflow for Success
For US healthcare decision-makers, understanding and optimizing this entire medical coding workflow is critical. Investing in:
- Well-trained and certified medical coders.
- Robust documentation improvement (CDI) programs.
- Efficient coding and billing software.
- Regular internal audits.
- A proactive denial management process.
will lead to a more efficient revenue cycle, improved cash flow, reduced compliance risks, and ultimately, a healthier financial foundation for your organization. By focusing on accuracy and efficiency at each step, you can transform the medical coding workflow from a back-office function into a strategic driver of financial success.
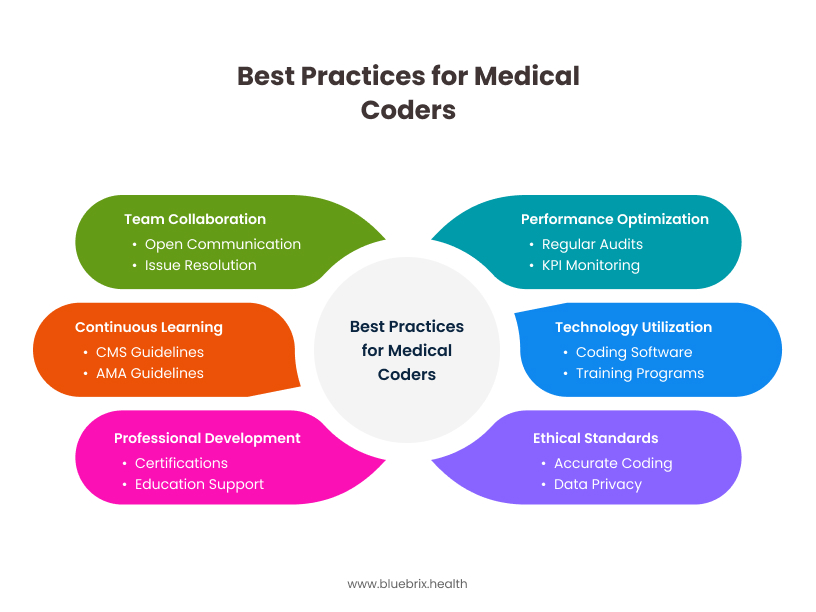 A well-supported coding team that prioritizes continuous learning, leverages technology, adheres to ethical standards, collaborates effectively, and strives for ongoing improvement is crucial for a healthy revenue cycle and regulatory compliance within your US healthcare organization.
A well-supported coding team that prioritizes continuous learning, leverages technology, adheres to ethical standards, collaborates effectively, and strives for ongoing improvement is crucial for a healthy revenue cycle and regulatory compliance within your US healthcare organization.
The Future of Medical Coding in US Healthcare: Adapting to Innovation
For US healthcare decision-makers, understanding the trajectory of medical coding is crucial for strategic planning and investment in future-proof solutions. The field is rapidly evolving, driven by technological advancements, regulatory shifts, and the ongoing pursuit of value-based care. Here are key aspects shaping the Future of Medical Coding in US Healthcare:
The Rise of Artificial Intelligence (AI) and Automation:
- AI-Powered Coding Assistance: AI and Machine Learning (ML) are increasingly being integrated into coding software. These tools can analyze clinical documentation using Natural Language Processing (NLP) to suggest the most accurate ICD-10-CM, CPT, and HCPCS codes in real-time.
- Automation of Routine Tasks: AI can automate repetitive tasks like eligibility verification, claim submission, and even initial code assignment for simpler cases, freeing up human coders to focus on complex scenarios and quality assurance.
- Predictive Analytics for Error Reduction: AI can analyze historical claims data to identify patterns indicative of potential coding errors or compliance issues, allowing for proactive corrections before claim submission.
- Augmented Coders, Not Replaced: While AI will handle more routine tasks, the consensus is that it will augment, rather than replace, human coders. Expert coders will be essential for handling complex cases, interpreting nuanced documentation, conducting audits, and overseeing AI-driven processes.
Enhanced Integration with Electronic Health Records (EHRs):
- Seamless Workflows: Future coding tools will be deeply integrated with EHR systems, providing real-time coding suggestions and insights directly within the clinician’s workflow. This aims to improve accuracy at the point of documentation.
- AI-Driven Clinical Documentation Improvement (CDI): AI can analyze clinical notes in real-time, prompting clinicians to provide more specific and billable documentation, reducing ambiguity and improving coding accuracy upstream.
The Continued Shift Towards Value-Based Care (VBC):
- Coding for Quality and Outcomes: In Value Based Caremodels, accurate coding will be even more critical for capturing the quality of care delivered and patient outcomes. Coders will need to understand how to accurately reflect the complexity of care and the achievement of quality metrics.
- Risk Adjustment Accuracy: Comprehensive and precise diagnosis coding (ICD-10-CM) will be paramount for accurate risk adjustment, ensuring fair reimbursement for managing patients with chronic and complex conditions.
- Coding for Care Coordination and Patient Engagement: As Value Based Care emphasizes holistic care, coding may evolve to better capture and reimburse for care coordination activities, patient education, and other engagement efforts.
Telehealth Expansion and Coding:
- Specialized Telehealth Codes: With the permanent establishment of telehealth as a key healthcare delivery model, the need for accurate coding of virtual visits, remote monitoring, and other telehealth services will continue to grow, requiring coders to stay updated on specific CPT and HCPCS codes and payer guidelines.
Increased Focus on Compliance and Data Security:
- AI-Powered Compliance Checks: AI tools will play a greater role in automating compliance checks, ensuring that coding practices adhere to payer-specific and government regulations, thus reducing audit risks.
- Cybersecurity in Coding: With the increasing digitization of coding processes and the use of AI, robust cybersecurity measures will be crucial to protect sensitive patient data.
Key Considerations
- Embrace Technological Advancements: Strategically invest in AI-powered coding tools and ensure seamless integration with existing EHR systems.
- Prioritize Training and Education: Equip your coding teams with the skills needed to navigate the evolving landscape, including AI literacy and Value Based Care coding principles.
- Focus on Data Integrity: Implement robust CDI programs to ensure accurate and complete clinical documentation, which is foundational for effective AI and accurate coding.
- Prepare for Value-Based Care: Ensure your coding practices accurately capture the quality and complexity of care to succeed in value-based payment models.
- Address Data Security and Compliance: Implement strong security measures to protect patient data in increasingly digital coding workflows.
The future of medical coding in US healthcare is dynamic and holds immense potential for improved efficiency, accuracy, and ultimately, a more robust and value-driven healthcare system. By understanding these trends and proactively adapting your strategies, you can position your organization for success in the years to come.
Resources for Medical Coders
Here are some key Resources for Medical Coders that US healthcare providers can use to support their professional development and ensure accurate coding practices:
Professional Organizations:
- AAPC (American Academy of Professional Coders): Offers certifications (CPC, CPB, CPMA, etc.), continuing education, a member magazine, online forums, local chapter meetings, and national conferences. A valuable resource for networking and staying updated.
- AHIMA (American Health Information Management Association): Provides certifications (CCS, CCA, RHIA, RHIT), practice guidance, online communities, education programs, and advocacy for health information professionals, including coders.
Official Coding Publications and Websites:
- CMS (Centers for Medicare & Medicaid Services): The official source for Medicare and Medicaid coding guidelines, updates, manuals (e.g., Medicare Claims Processing Manual), and transmittals. Crucial for understanding federal payer rules.
- AMA (American Medical Association): The publisher of the CPT codebook and related resources, including coding guidelines, webinars, and the CPT Assistant newsletter. Essential for outpatient and physician coding.
- NCHS (National Center for Health Statistics): Part of the CDC, NCHS is responsible for the ICD-10-CM Official Guidelines for Coding and Reporting and provides access to the ICD-10-CM code files and updates.
- U.S. Government Printing Office (GPO): Where official versions of federal regulations, including HIPAA, can be accessed.