
Why write an article specifically on behavioral health billing and not just healthcare billing as a whole? Because behavioral health billing is quite simply much more complex than the others; owing to factors such as the coding specifics differing from the ones used in general medical billing; behavioral health services including a variety of treatments (as well as the assessment of health and treatment plans being nuanced and variable); and payer regulations varying wildly based on extenuating factors.
However, as we in the healthcare ecosystem know all too well, proper revenue cycle management is a necessity for a practice to function effectively and efficiently, while serving the healthcare needs of as many potential patients as possible. Presently, this is a tool that is lacking in the behavioral healthcare space, with yearly research suggesting that in the United States, nearly $300 billion dollars is being wasted in potential earnings owing to mental illness.
Challenges in behavioral health billing

Let us explore the specific challenges faced in handling behavioral health billing:
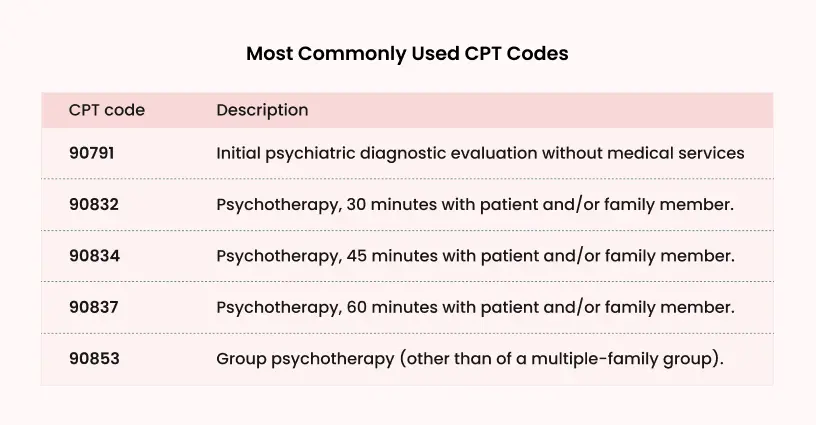
- Coding Requirements: The CPT (Current Procedural Terminology) codes differ for behavioral health and general health. Without proper coding, submissions cannot be made accurately, and reimbursement cannot be received in a timely manner. There are many CPT codes and expecting behavioral healthcare providers (or their administrative staff) to recall them and note them down without error 100% of the time is a lot to ask. For example, psychotherapy with the patient and/or family member of the patient for 30 minutes or 45 minutes doesn’t seem like a major difference, but they are noted down differently (CPT code 90832 and 90834 respectively), and the reimbursement received for each varies by a significant enough margin that over time, it would cause a major difference in the provider and the practices financial resources.
- Pre-authorization hurdles: Pre-authorization is a necessity to acquire before providing care, as it ensures that the provider will be reimbursed, and the patient will not be burdened with unforeseen out-of-pocket expenses. This is a tedious task, which asks the provider to submit to the payer a detailed and descriptive layout of the patient’s diagnosis and treatment plan, along with supporting documents.
- Payer regulations: Meeting pre-authorization requirements, coding standards, complying with laws and regulations, timely submission of claims (and handling denial), payer requirement variations are just a few of the many hurdles that need to be crossed by the provider to ensure they receive reimbursement from the payer.
- Uncertainty of treatment plans: Behavioral health treatment varies depending on the patient and thus, it is nigh impossible to create a billing procedure that can be uniformly implemented and followed. A patient suffering from depression brought on by a temporary grievance, for example: a breakup, requires a very different treatment plan compared to a patient suffering from depression due to childhood trauma.
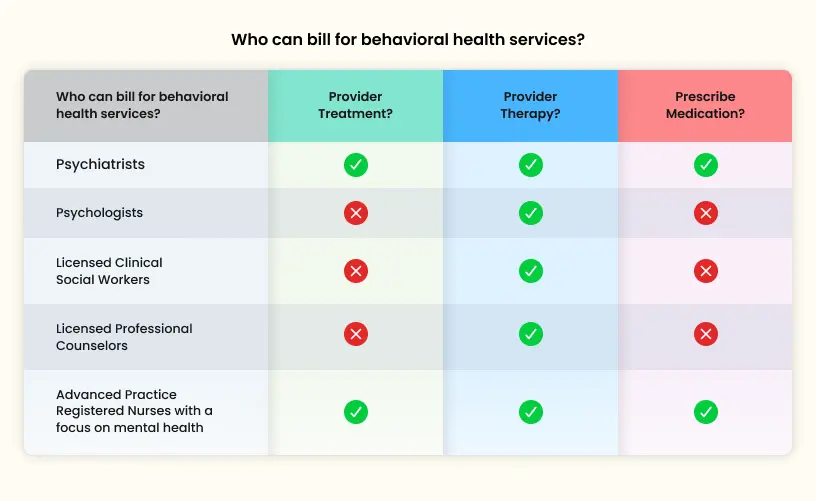
Who can bill for behavioral health services?
Guidelines for behavioral health billing
Behavioral health billing involves unique complexities, requiring adherence to specific guidelines to ensure accurate and compliant billing. These guidelines help healthcare providers navigate coding, insurance verification, and reimbursement processes for mental and behavioral health services.
The following guidelines, irrespective of the type of organization or location, must be followed by all organizations:
- Ensure that you are using the correct CPT codes when filing claims for the services given.
- Ensure that that patient’s insurance coverage covers the treatment plan before administering the treatment.
- Obtain pre-authorization if required.
- Provide documentation that is uncorrupted, up-to-date and accurate.
- File claims in the time frame required by the payer.
- Stay up to date with federal and state regulations and meet them.
CMS (Centers for Medicare & Medicaid Services) behavioral health billing guidelines
- While CMS covers a wide range of behavioral health services, all of them MUST be medically necessary (and must be proven as such) for CMS to cover their payment.
- Providers, whether they are medical professionals, such as psychiatrists or nurse practitioners, or they provide other forms of mental health support, such as social workers, are eligible to receive reimbursement.
- Accurate coding, documentation and compliance with regulations are all required necessities.
State-wise specifications and regulations
- Medicaid program coverage varies based on state regulations. So, services that might be covered under the regulations of one state, might not be covered under a different one. For example, in New York, licensed social workers and mental health counselors are eligible under Medicaid to receive reimbursement; however, in Florida, the only providers who are eligible for reimbursement under Medicaid are licensed medical professionals, like a psychologist or a psychiatrist.
- Telehealth regulations have experienced wide-spread growth in the years since the Covid-19 pandemic, but as a newly popularized method of treatment, it is still gaining ground and has not been adopted completely across all states.
- Licensing requirements, as well as coding, documentation and mental health parity laws and regulations all have a baseline requirement across the nation, but certain states ask that additional or different requirements be met as well for reimbursement to be given.
Payer guidelines
- Medicaid and Medicare provide reimbursement based on whether the services rendered are medically necessary and covered under their offerings. The necessary tasks that must be completed (coding, documentation, etc.) vary based on state regulations and the provider’s specifications.
- Private insurances provide reimbursements based on a wider range of factors, such as the patient’s specific insurance plan, along with all the requirements that Medicaid and Medicare also require from providers.
- Behavioral Health Billing for Telehealth, as previously mentioned, is a growing field, with telehealth having exploded in popularity and usage in the years since the 2020-2021 pandemic. The billing requirements for this method of mental healthcare provision, like any other behavioral health provision method, are dependent on the specific state/payer requirements to receive reimbursement.
Most used CPT codes
Best practices to ensure proper behavioral health billing
Obtain a competent and malleable EHR (Electronic Health Record) system
Many of the issues in billing rises from human error. The usage of an EHR would eliminate or greatly reduce that risk and ensure the data is accurate. Furthermore, it would save the administrative staff stress and time, which can be allocated towards focusing on patient care.
EHRs can also be a great asset in ensuring that the provider complies with regulatory requirements, as well as coding standards, while implementing validation checks, maintaining data synchronization, and boosting inter-office coordination.
Consider hiring a billing service
Billing/Revenue Cycle Management services are, as the name suggests, experts in their field. They can greatly help behavioral health practices by ensuring that the provider’s practices are up-to-date and meets regulation; they can handles claims submission, as well as denial management; the outsourcing of billing would greatly reduce administrative costs, as well as reducing mental burnout for the administrative staff; the proper filing of claims and handling of denials/delays would lead to faster reimbursements, which would result in increased revenue for the provider, while providing more time and resources that can be utilized in providing care.
Utilize tools such as AI
While artificial intelligence and its implementation is still a controversial topic in many fields, healthcare (and its adjacent industries) is a field in which AI can undoubtedly be used for good. AI can be used effectively to aggregate a great swath of information (such as claim procession time, claim denial reasons, etc) and provide reports that would give a better understanding of how best to optimize the practice for efficiency.
Denial management
Denial management is an unavoidable reality when dealing with behavioral health billing. There are many reasons that a claim can be denied; the main causes for denial are usually:
- The treatment is not considered a necessity for the patient and therefore not covered by the payer.
- Improper or incorrect coding
- Failure to achieve pre-authorization
- Improper or incomplete documentation
Here are some strategies that could be implemented to avoid denials in the future:
- Aggregate the previous denied claims to better understand the reasons behind why they were denied and find recurring issues that can be corrected
- If you choose to do in-house billing, ensure that the billing staff is properly trained (as well as regularly updated on any regulations and practices)
- Ensure that pre-authorization and eligibility are verified before any treatment is administered
- We’ve repeated this many times over the course of this article, but it cannot be reiterated enough the importance of accurate coding and documentation
Benefits Of outsourcing behavioral health billing
- Negating or greatly reducing coding and documentation issues affecting reimbursement
- Ease of mind that pre-authorization and insurance verification are handled properly and without burdening the administrative staff
- Centralized billing allows for larger practices with multiple locations to ensure that payment is allocated to the locations they are supposed to be sent to
- Data collection becomes seamless and automated, once again removing the possibility of human error causing delays
- Administrative tasks, such as scheduling/re-scheduling or setting up recurring appointments, can be automated easily and conveniently
Overcoming behavioral health billing challenges with blueEHR and blueBriX: Key solutions and expertise
Behavioral health billing poses many challenges. But by leveraging both the blueEHR system‘s advanced features and blueBriX’s technical expertise, healthcare providers can greatly improve their revenue cycle management. Outsourcing RCM to blueBriX, ensures the healthcare provider benefits from both cutting-edge technology and deep industry experience. Here’s how blueBriX tackles key billing issues:
- Practice analysis & custom workflow: We analyze the provider’s practice workflow and offer a custom solution to align with their requirements. We also provide suggestions for workflow optimization to bring better RCM results.
- Complex billing codes: Behavioral health billing often involves intricate coding, leading to claim denials. The blueEHR billing module simplifies the management of these codes, ensuring accurate and compliant billing. With blueBriX’s expertise, providers can reduce coding errors further, enhancing claim approvals.
- Insurance verification and authorization: Navigating insurance coverage and prior authorization is time-consuming. blueEHR automates verification and authorization processes, while blueBriX’s experienced team ensures these workflows are optimized, reducing delays and manual effort.
- Centralized billing for multiple locations: Managing billing across various locations can lead to errors. blueEHR’s centralized billing system streamlines payment management, and blueBriX enhances this by ensuring smooth, efficient billing across locations with minimal confusion.
- Data collection for billing: Collecting all necessary billing data is often cumbersome. blueEHR automates data collection during client interactions, and blueBriX ensures that this data is efficiently processed for seamless billing.
- Insurance and patient self-pay management: Balancing insurance claims and self-pay options can be difficult. Our technology makes it easy to manage both payment options, and our team ensures that this process remains efficient, enhancing provider cash flow.
- Recurring appointments and billing: Managing recurring appointments and ensuring accurate billing can be labor-intensive. blueEHR automates scheduling and billing for these appointments, and blueBriX adds a layer of reliability, ensuring that every session is accurately billed.
By partnering with blueBriX for outsourced RCM services, providers not only benefit from blueEHR’s robust features but also gain the advantage of a team with deep technical expertise and industry knowledge. This combination reduces administrative burdens and ensures a highly efficient RCM process, leading to better financial outcomes for healthcare providers.
Final Take
Behavioral health and its importance to overall health has never been taken more seriously by the general population than it is now. However, we are still woefully uneducated, apathetic and lacking in the provision of it for those in need of it. Proper behavioral health billing might not at first seem like it impacts the accessibility of getting behavioral health care, but as this article proves, billing does make a deep impact.
Bibliography
Hidden recession? Mental illness costs the U.S. a staggering $282 billion annually, shows new study