Value-Based Care (VBC) promises to transform healthcare by linking payments to quality outcomes and efficiency rather than volume of services. But despite this promise of better rewards and fairer reimbursement, many healthcare organizations are still struggling to fully capture these financial incentives. What’s standing in their way? Rather, what are the gaps and challenges that need to be addressed to untap the full potential of VBC payments?
Before diving into the challenges, let’s take a step back and understand how the value-based care model actually drives incentive payments.
Understanding value based care financial multipliers
Value-based care shifts how healthcare providers are paid from rewarding volume of services delivered to rewarding quality and efficiency of care. Instead of a simple fee-for-service, VBC uses complex incentive structures designed to improve clinical outcomes, patient satisfaction, and cost savings.
What are financial multipliers in VBC?
Financial multipliers in VBC refer to the way incentives grow exponentially as providersclose more care gapsand achieve higher performance across multiple domains. Rather than earning incremental, flat bonuses for each improvement, providers can multiply their total incentives by addressing a wider set of quality measures and demonstrating continued improvement.
How CMS and payers score performance
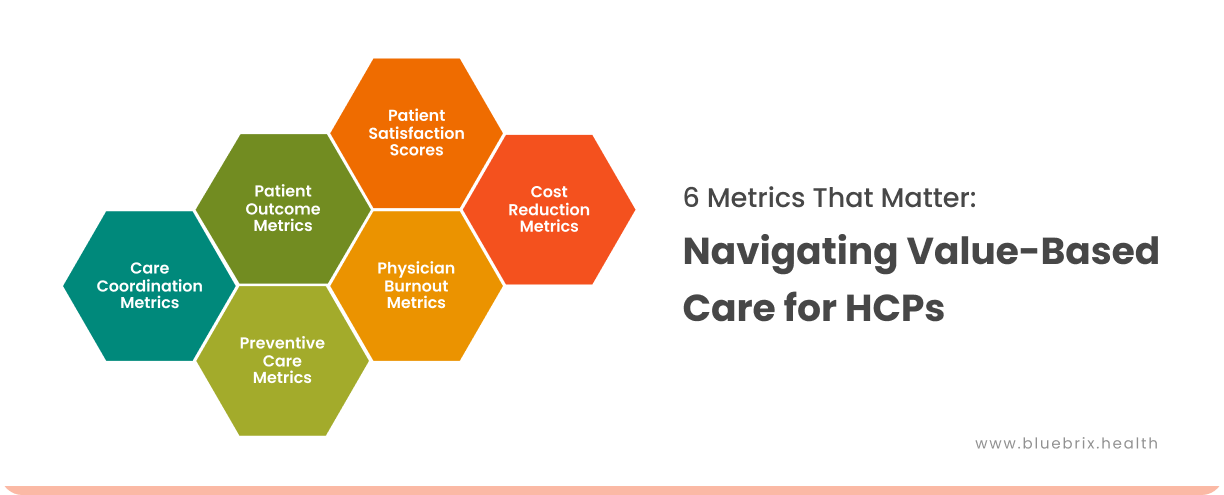
The Centers for Medicare & Medicaid Services (CMS) and other payers evaluate providers based on key domains such as:
- Clinical outcomes: Reduction in hospital readmissions, better management of chronic conditions, preventive screening completion.
- Patient experience: Satisfaction scores, effective communication, care accessibility.
- Cost efficiency: Lowering unnecessary services, reducing emergency visits, managing resource use wisely.
What’s standing in your way of earning full value-based care incentives?
Value-based care holds enormous promise, but for many providers, reaching the full rewards feels just out of reach. Incentives are often tied to complex requirements, shifting rules, and factors beyond a provider’s direct control. From evolving CMS regulations to the realities of patient non-adherence, organizations face a maze of obstacles that undercut their ability to consistently qualify for bonuses. Below, we break down the most common and most costly roadblocks that stand between providers and their VBC incentive goals:
Limited duration and uncertainty of incentives
Many value-based incentives, including the Advanced APM bonus under MACRA, have been temporarily extended or gradually reduced from 5% initially down to 3.5% in 2025 and 1.88% in 2026. This creates uncertainty for providers, making it difficult to justify ongoing investments in care coordination, technology, and staffing essential for sustained VBC success.
Inadequate risk adjustment and patient complexity considerations
Providers caring for highly complex or high-cost patients may find that risk adjustment methodologies don’t fully capture patient severity, leading to inadequate compensation despite high-quality care.
Complex and evolving program rules
Value-based care programs are built on rules that rarely stay the same for long. Frequent updates to CMS and payer frameworks whether in eligibility criteria, incentive structures, or quality benchmarks, create uncertainty for providers. Even small shifts in how measures are defined or scored can change performance outcomes, forcing organizations to continually adjust care strategies, documentation processes, and reporting systems. This constant flux makes it difficult to achieve stability and reliably qualify for incentives.
Administrative and reporting burdens
High administrative workload related to data collection, coding, reporting, and compliance can overwhelm provider staff, causing delays or mistakes that reduce incentive payouts.
Data problems and technology gaps
Value-based care requires good data on outcomes, patient experience, and costs. But most organizations struggle because their systems don’t talk to each other, making data collection and analysis difficult and time-consuming.
Patient non-adherence and social determinants
Despite providers’ best efforts, patient factors such as non-adherence to care plans or unaddressed social determinants of health negatively impact outcomes and scores that determine incentives.
Getting everyone on the same page
Large health systems need buy-in from doctors, administrators, and insurance companies to make value-based care work—but getting all these groups to align and commit is extremely difficult, even though it’s absolutely essential for success.
Fragmented care delivery and poor coordination
Fragmentation between providers, specialties, and care settings reduces care continuity, leading to poor outcomes and higher costs that penalize providers under VBC. Many organizations lack effective care coordination frameworks to address this fragmentation.
That said, in this blog, we will explore how effective care coordination directly drives VBC incentives—examining the concrete connection between better communication, streamlined workflows, and the quality metrics that value-based programs reward. By ensuring patients receive the right care at the right time, care coordination becomes a measurable lever for achieving 2x-4x incentive improvements.
Care coordination gaps that undermine value-based care incentives
At the heart of value-based care is the promise of delivering the right care, at the right time, in the right setting. That promise depends on seamless coordination across providers, systems, and patients. But when coordination breaks down due to staffing shortages, siloed systems, or disengaged patients, the ripple effect shows up in missed follow-ups, preventable readmissions, and poorer outcomes. These gaps don’t just hurt patients; they directly erode the quality scores and cost benchmarks that determine whether providers earn their full VBC incentives.
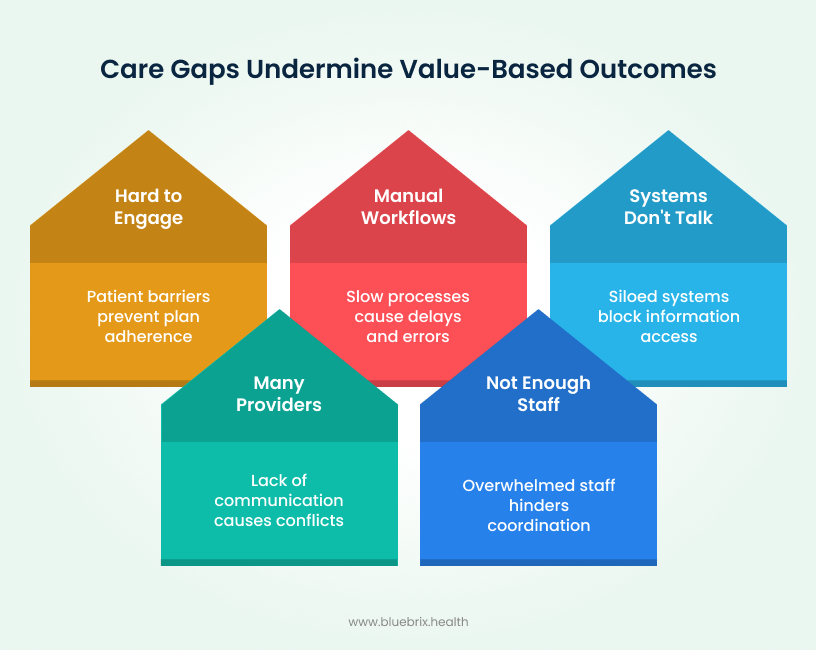
Not enough dedicated staff
You’re stretched thin. Your doctors and nurses are already overwhelmed with patient visits, documentation, and emergencies. When care coordination falls on their shoulders as an extra responsibility, something has to be given and usually it’s the time you need to track down test results or confirm that follow-up appointments actually happen.
Care spread across many providers
Your patients see multiple specialists, for example a cardiologist, primary care doctor, therapist, maybe others. When these providers operate in separate systems without integrated communication, critical information doesn’t flow between them. A medication prescribed by one specialist might conflict with another, but the interaction goes unnoticed because the providers lack real-time visibility into each other’s decisions.
Systems that don’t talk to each other
Different clinics and hospitals use different computer systems that can’t share information easily. One clinic has all the patient records in System A, but the hospital uses System B. Your staff wastes hours manually searching through separate systems just to piece together a patient’s complete health picture. The information exists—it’s just trapped in silos where nobody can access it in real time.
Manual and slow workflows
Many care coordination tasks still happen in the old ways like phone calls, faxes, emails, handwritten notes, etc. Sending a referral to a specialist might take days. Following up on whether a patient attended their appointment requires multiple phone calls. These manual processes are slow, prone to errors, and delays in care follow naturally.
Hard to engage patients fully
Even with the best care plan, patients don’t always understand what they’re supposed to do. Some face real barriers like not having transportation to appointments, struggling financially to afford medications, or dealing with housing instability. If nobody addresses these practical problems, care coordination fails because the patient can’t actually follow through on their care plan.
When care coordination falters, the result is not just operational inefficiency, but a direct hit to patient outcomes and the financial incentives tied to value-based care. The good news is that these challenges aren’t insurmountable. By rethinking workflows, leveraging technology, and engaging both staff and patients more effectively, organizations can turn coordination from a liability into their strongest driver of VBC success. In the next section, we’ll explore practical strategies to close these gaps and maximize incentives.
Care coordination strategies to maximize value-based care incentives
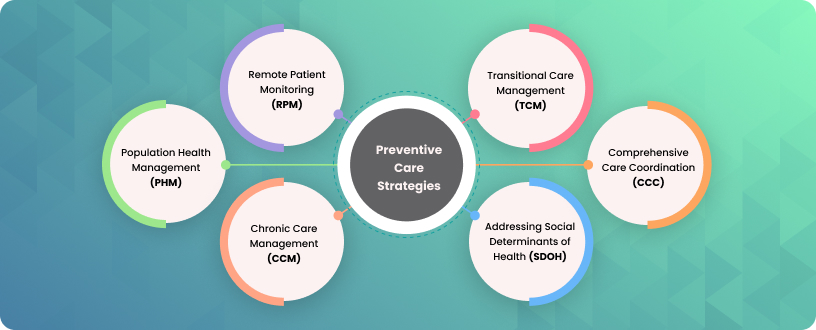
Now that you know care coordination is one of the cornerstones of VBC success, the real challenge comes during execution—and that’s where most healthcare organizations fail. The strategies below will help you actually pull it off—closing care gaps, getting your team on the same page, and capturing those VBC incentives you’ve been leaving on the table.

Integrating data systems for a unified patient view
Make sure your EHR systems are interoperable platforms that break down data silos, combining clinical, claims, behavioral, and social determinants data into a single accessible dashboard for care teams.
Automating routine workflows and communication
Instead of relying on manual workflows like phone calls, emails, and spreadsheets, opt for care smart solutions that automate key tasks. Appointment scheduling, referral routing, patient outreach reminders—these happen with just a few clicks. With automation you can eliminate manual errors, speed up processes, and free your staff to focus on patient care and higher-value work instead of administrative tasks.
Implementing evidence-based care pathways
Evidence-based care pathways standardize how your team delivers care. Clear protocols based on proven guidelines tell your care team exactly what actions to take and when. This eliminates inconsistency, reduces errors, and ensures all providers work together smoothly. Standardized pathways deliver better outcomes and make care coordination efficient, exactly what value-based care requires.
Leveraging HCC coding and risk stratification
Leveraging HCC coding and risk stratification helps care teams identify patients with complex or high-risk conditions who need extra care coordination. By focusing resources on these patients, providers can proactively manage their health—reducing hospitalizations and costly complications—which directly improves patient outcomes and supports efficient care delivery.
Financially, accurate HCC coding ensures providers receive fair reimbursement that reflects the complexity of care given. Higher risk scores generated through HCC coding lead to increased payments, incentivizing organizations to invest in thorough documentation and focused care coordination programs. This alignment of clinical effort and financial reward is key to sustaining value-based care success.
Enhancing transitions of care
Coordinated handoffs during patient transitions such as hospital discharge, specialist referrals, and transfer from facility to home prevent readmissions and maintain care continuity, directly impacting VBC success. Take a diabetic patient discharged with a new insulin regimen. With coordinated transitions, discharge instructions reach all providers instantly, medications are reconciled, and automated follow-up reminders ensure adherence. The patient understands her treatment plan, stays compliant, and maintains stable health. She avoids the ER, prevents costly readmission, and strengthens your VBC performance all because coordinated handoffs connected the dots.
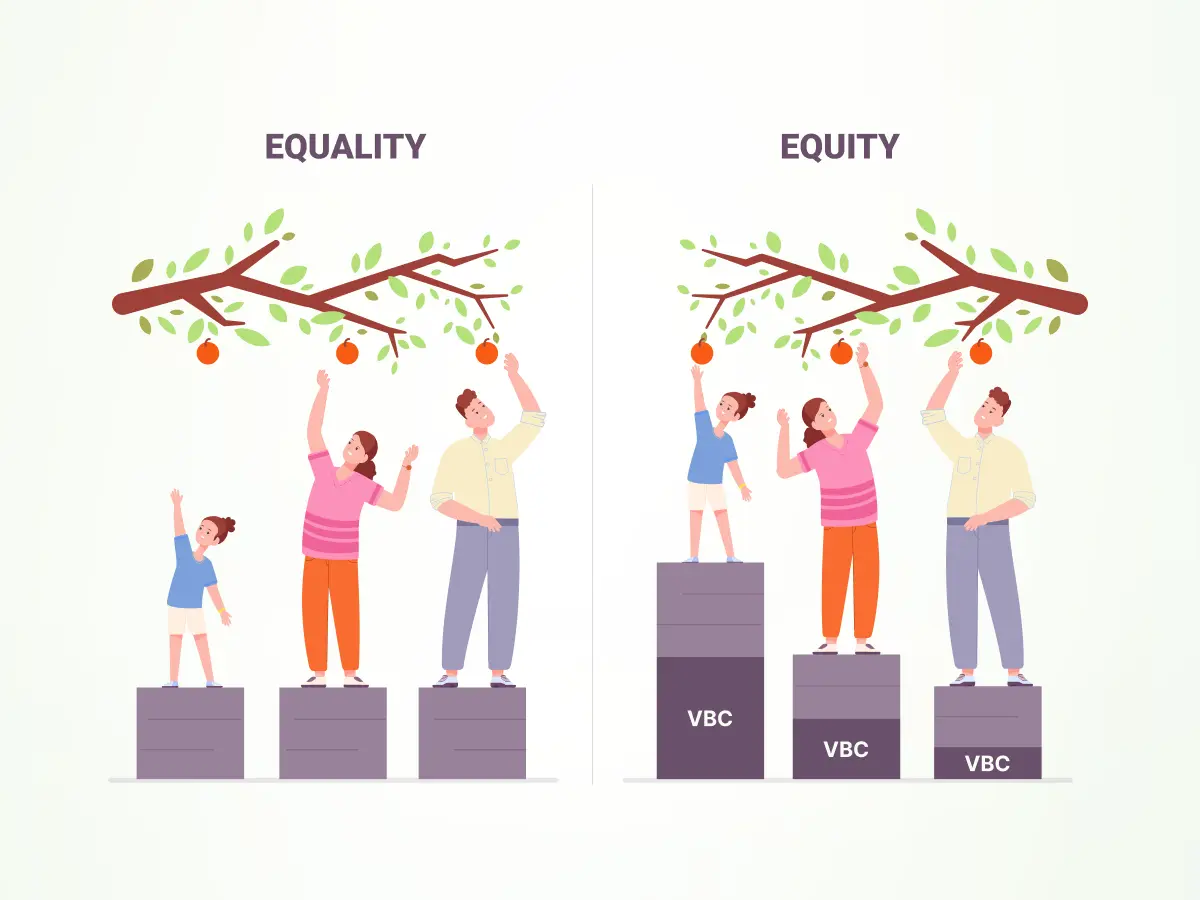
Addressing social determinants of health(SDOH)
Social factors like limited transportation, financial hardship, and housing instability affect every stage of a patient’s care journey. By addressing these barriers through proactive identification and linking patients to community resources, you can improve care plan adherence, reduce hospital readmissions, and lower overall costs. These improvements directly influence key performance metrics in value-based care (VBC) programs.
Value-based payment models increasingly reward providers who manage social risks effectively among vulnerable populations. CMS ACO REACH and MSSP ACOs have begun rewarding the use of SDOH Z-codes and social risk screening in 2024–2025, aligning incentives with managing social risks effectively. These kinds of incentives for improving outcomes in high-risk communities motivate organizations to invest in social care interventions.
Empowering patient engagement and self-management
Patient engagement is pivotal in value-based care, aiming to actively involve patients throughout their care journey. The objective is to empower patients by providing access to their medical records, educational resources, and self-service tools like appointment scheduling. This personalized and timely communication encourages patients to follow their care plans, make informed decisions, and stay connected with their healthcare team.
By fostering this active participation, providers see better adherence to treatments, fewer missed appointments, and improved health outcomes. This not only benefits patients but also helps healthcare organizations meet quality measures.
Monitoring performance and supporting quality improvement
Monitoring value-based care performance means using three key tools: HEDIS measures how well you deliver preventive and chronic care, MIPS evaluates your performance on quality, cost, and improvement activities while directly linking results to reimbursement, and STAR ratings give Medicare Advantage plans a five-star performance score that influences patient choice and funding bonuses.
Real-time dashboards let you track these metrics continuously, identify gaps quickly, and adjust strategies before problems compound. High scores deliver concrete payoffs: higher reimbursements, performance bonuses, increased patient trust, and stronger positioning in value-based care models. The difference between monitoring and not monitoring isn’t just about compliance—it’s about capturing the financial and competitive advantages that value-based care rewards.
These strategies aren’t theoretical—they’re the operational backbone that determines whether your organization thrives or struggles under value-based contracts. But what do these strategies actually deliver? The answer lies in measurable financial and clinical outcomes—the real returns on coordinated care. Let’s break down exactly what you stand to gain.
The financial and clinical impact of coordinated care in value-based care models
When care coordination works, the benefits show up in two places that matter most: your revenue and your patient outcomes. These aren’t vague improvements or long-term projections—they’re direct, measurable gains that prove your coordination strategies are paying off. Here’s exactly what effective care coordination delivers:
Better patient outcomes
When you proactively close care gaps and ensure consistent treatment follow-through, your patients experience fewer complications, faster recoveries, and better management of chronic conditions. They’re healthier because your coordinated approach catches problems early.
Lower avoidable costs
Preventable hospital admissions, emergency department visits, and redundant testing decline significantly. You eliminate waste, free up resources, and reduce overall healthcare spending, directly improving your financial position.
Stronger team collaboration
You can communicate more effectively with every provider involved in your patient’s care and access real-time information instantly. No more waiting for faxes or chasing down specialists for updates. Coordinated decisions happen faster because all providers see the same complete clinical picture. Delays disappear. Medical errors decrease because there’s no miscommunication or missing information; everyone knows exactly what’s been done and what needs to happen next.
Increased patient trust and engagement
Patients feel supported and confident in their care when they see your team working together seamlessly. Better engagement leads to improved treatment adherence and long-term health success—strengthening patient loyalty.
Better resource management
You can focus more on your clinical and financial resources where they’re needed most. Care management efforts become strategic instead of reactive, and your team operates more efficiently with less wasted effort.
Sustainable financial performance
By demonstrating measurable improvements and reducing costly events, you can secure incentive payments, shared savings, and long-term viability in value-based programs. Your organization builds financial stability through better care coordination.
Reduced revenue cycle burden
Effective care coordination lowers claim denials by ensuring accurate, complete documentation and timely submissions. Faster claim approvals minimize administrative delays and eliminate time wasted on re-submissions, improving cash flow and financial stability.
blueBriX: advanced tech solutions for your seamless care coordination
Having spent 15 plus years in healthcare, we understand that tech plays a vital role in orchestrating care across platforms. That’s exactly what we did with blueBriX—designed it to connect systems, automate workflows, and adapt to every care setting.

Seamless integration and interoperability
blueBriX empowers healthcare organizations with robust integration capabilities, ensuring seamless interoperability across diverse systems. Our platform connects effortlessly with EHRs, claims systems, behavioral health tools, telehealth platforms, and community resource databases. This integration breaks down data silos by capturing clinical, claims, behavioral, and social determinants data from multiple systems, making it accessible in real time to all care team members.
Comprehensive referral management
blueBriX streamlines referral processes by consolidating inbound and outbound referrals onto a single platform. Providers and staff can track, prioritize, and communicate about referrals in real time, dramatically reducing delays and referral leakage. Automated insurance verification and intelligent provider matching ensure referrals go to the right specialists quickly to keep patients on track.
Dynamic and configurable care plan engine
Every provider involved in a patient’s care can update and access shared, evidence-based care plans within blueBriX. This collaborative engine ensures all care team members stay aligned with treatment goals, medication changes, and follow-ups, reducing inconsistencies and improving outcomes.
Integrated risk stratification powered by AI
blueBriX captures data from multiple clinical, claims, behavioral, and social platforms to create a holistic patient profile. Advanced AI algorithms analyze this data to identify high-risk patients early and prioritize them for targeted interventions—helping prevent complications and costly hospitalizations.
Workflow automation & resource management
The platform automates routine tasks such as appointment scheduling, reminder communications, referral routing, and care task assignments. This eliminates manual processes, minimizes errors, and frees care coordinators to focus on higher-value patient care activities, maximizing operational efficiency.
Addressing social determinants of health
blueBriX integrates social risk factor screening and connects patients to tailored community resources, such as transportation assistance and housing support. By proactively managing these barriers, the platform improves adherence to care plans and supports equitable care delivery.
Patient engagement tools for personalized care
Patients gain access to their health records, receive customized educational content, and use self-scheduling tools. These features promote self-management, reinforce adherence, and foster an active partnership between patients and providers.
Telehealth integration
For patients unable to attend in-person visits, blueBriX offers integrated telehealth capabilities that ensure seamless care continuity. Built with compliance in mind, blueBriX’s telehealth solution securely supports HIPAA and other regulatory standards, facilitating virtual visits without compromising patient privacy or data security. This integration helps healthcare organizations extend care beyond traditional settings while maintaining regulatory adherence and improving patient engagement.