The hidden revenue risk in inpatient psychiatry
Inpatient psychiatric care, while profoundly complex and essential, often faces a unique challenge that directly impacts its financial viability. Many facilities unknowingly leave significant revenue on the table due to common documentation pitfalls. Psychiatric Diagnosis-Related Groups (DRGs) are frequently lower than they should be, primarily due to documentation issues. This leads not only to substantial revenue loss but also exposes facilities to considerable compliance risks. For instance, studies indicate that approximately 25% of claims are rejected initially in the healthcare industry due to billing errors, and mental health practices are no exception.
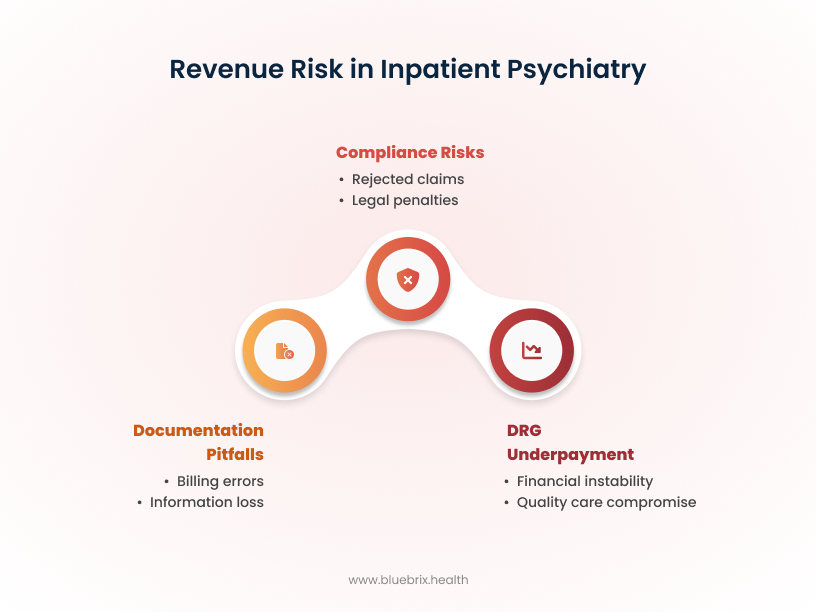
The inherent disconnect between the nuanced, often subjective clinical reality of complex psychiatric care and the objective, codified data required for DRG reimbursement is a significant point of vulnerability for many facilities. When subjective clinical narratives must be translated into objective codes, there is a substantial risk of information loss or misinterpretation if the process is not meticulously managed. This loss directly impacts DRG assignment, leading to underpayment that, in turn, can compromise a facility’s ability to invest in quality care, retain skilled staff, and maintain overall financial stability, particularly given the high resource utilization often observed in psychiatric settings.
The documentation imperative in inpatient psychiatry
Inpatient psychiatric facilities provide essential care, but their financial stability hinges on precise documentation. In the U.S. healthcare system, DRGs dictate reimbursement for hospital stays based on diagnosis, procedures, age, and comorbidities. The challenge in psychiatry lies in translating subjective clinical narratives into the objective, specific data required for accurate coding.
Inaccurate or incomplete documentation directly leads to revenue loss and increased compliance risks. For instance, DRGs explain less than 8% of the differences in Length of Stay (LOS) for psychiatric care, highlighting the classification system’s limitations in this specialty. This gap between clinical nuance and coding requirements makes query management an essential strategy for revenue integrity.
DRGs and dollars: The direct link to your psych reimbursement
DRGs are the foundation of hospital reimbursement, making coding accuracy critical for revenue and compliance. Psychiatric DRGs are often lower than they should be due to documentation deficiencies, leading to underpayment for complex, resource-intensive care. Only 15% of admissions for psychosis (DRG 885) are paid above 150% of Medicare rates, compared to 71% for hip and knee replacements (DRG 470). Mental health hospitalizations also have the lowest average financial margins, at $136 per day, versus $611 per day for other medical hospitalizations.
Lack of specificity in diagnoses is a primary culprit, forcing coders to assign lower-weighted DRGs. Insufficient documentation results in underpayments and frequent denials; Medicare Advantage plans, for example, deny 17% of initial claims, leading to a 7% net reduction in provider revenue. HealthCare.gov insurers denied 19% of in-network claims in 2023. These denials trigger costly appeals, diverting resources. Accurate documentation, conversely, ensures optimal reimbursement and reduces audit risks. Practices that fail to follow up on denied claims can lose an average of $100,000 in uncollected revenue annually.
5 critical documentation gaps that are hurting your inpatient psych DRGs
Inpatient psychiatric facilities frequently encounter specific documentation gaps that, if unaddressed, can significantly undermine their DRG assignments and lead to substantial revenue loss. Understanding these common pitfalls is the first step toward rectifying them.
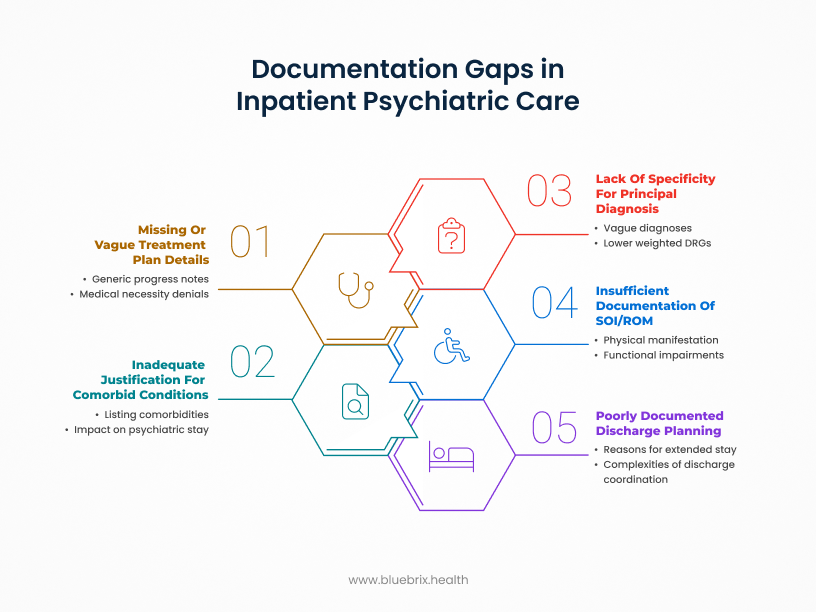
1. Lack of specificity for principal diagnosis
The principal diagnosis—the primary reason for the patient’s admission—must be documented with the highest possible level of specificity. Vague or generalized diagnoses prevent coders from assigning the most accurate and appropriate DRG. For instance, simply documenting “Depression” instead of “Major Depressive Disorder, recurrent episode, severe with psychotic features” or “Bipolar Disorder” instead of “Bipolar I Disorder, current episode manic, severe with rapid cycling,” fails to capture the true clinical complexity and resource intensity. Less specific diagnoses invariably map to lower-weighted DRGs, resulting in significant underpayment for the intricate care provided. The lack of specificity in psychiatric diagnoses is a direct cause of lower DRG assignments, with studies indicating that DRGs explain less than 8% of the differences in Length of Stay (LOS) for psychiatric care due to the complexity of diagnosis and less defined criteria.
2. Inadequate justification for comorbid conditions/secondary diagnoses
Documentation of psychosocial factors and comorbidities is critical in psychiatric care. For example, if a patient admitted for schizophrenia also has uncontrolled diabetes and severe anxiety, merely listing these conditions without documenting their active management, their influence on the patient’s psychiatric care, or their effect on length of stay or resource use, will prevent them from impacting the DRG. Failure to adequately link these comorbidities to the inpatient stay means missing out on crucial Complication/Comorbidity (CC) or Major Complication/Comorbidity (MCC) codes, which can significantly increase the DRG weight and corresponding reimbursement.
For instance, while stays for a principal mental health or substance use disorder (MSUD) cost an average of $7,100, stays where a physical condition is the principal diagnosis but a coexisting MSUD is present cost significantly more, averaging $14,300. This highlights the financial impact of accurately documenting comorbidities.
3. Missing or vague treatment plan details and progress notes
The treatment plan and daily progress notes are fundamental to justifying the medical necessity of the inpatient stay, detailing the specific interventions provided, and documenting the patient’s response to treatment. Vague entries or missing details undermine the entire rationale for the level of care. An example of this gap includes notes stating simply “Patient doing well” without elaborating on specific therapeutic interventions (e.g., individual therapy sessions, group therapy participation, medication management with dosage adjustments and rationale, crisis intervention strategies), the patient’s engagement, or the clinical justification for continued hospitalization. Documentation must explicitly support medical necessity and the services provided throughout the entire admission.
A lack of detailed progress notes can lead to denials for medical necessity, particularly for longer stays. Payers may contend that the inpatient level of care was no longer warranted, leading to costly recoupments and directly impacting the ability to justify the assigned DRG.
4. Insufficient documentation of severity of illness (SOI) and risk of Mortality (ROM)
Documentation must accurately reflect the patient’s overall severity of illness and risk of mortality, even if these factors are not directly related to the principal psychiatric diagnosis. This includes capturing physiological abnormalities, functional impairments, and the intensity of monitoring required. Consider a patient with severe depression exhibiting significant self-neglect, dehydration, and electrolyte imbalance. If these physical manifestations of their mental illness are not clearly documented as impacting their overall health status and necessitating specific medical interventions, their true SOI and ROM will be understated.
Clinical Documentation Improvement (CDI) plays a vital role in ensuring documentation accurately reflects patient severity. Understating SOI and ROM prevents the assignment of higher-weighted DRGs that appropriately account for the patient’s true clinical complexity and resource consumption, a crucial determinant in DRG assignment. Psychiatric patients often experience long stays and high resource utilization, yet documentation frequently fails to reflect this comprehensive picture.
5. Poorly documented discharge planning and aftercare
While often perceived as an administrative task, discharge planning documentation is crucial for justifying the entire length of stay. It demonstrates the ongoing need for inpatient care until a safe and appropriate discharge disposition could be arranged, and it meticulously outlines the patient’s ongoing care plan. For instance, if a patient is clinically stable for discharge but requires complex coordination for housing, outpatient therapy, and medication management due to their severe mental illness and lack of social support, and these complexities and the efforts to arrange them are not meticulously documented, the final days of the inpatient stay might be questioned for medical necessity.
Inadequate discharge planning documentation can lead to denials for the latter portion of an inpatient stay, especially if the patient is clinically stable but awaiting placement or community resources. This can effectively reduce the reimbursed length of stay, significantly impacting the overall DRG payment.
The power of proactive query management: bridging the gaps for financial health
Addressing the pervasive documentation gaps in inpatient psychiatry requires a strategic, proactive approach. This is where the power of query management, a core component of Clinical Documentation Improvement (CDI), becomes evident. Query management is a collaborative process where trained CDI specialists or medical coders meticulously review patient documentation. When they encounter ambiguities, incompleteness, or contradictions, they issue specific queries to clinicians, seeking clarification.
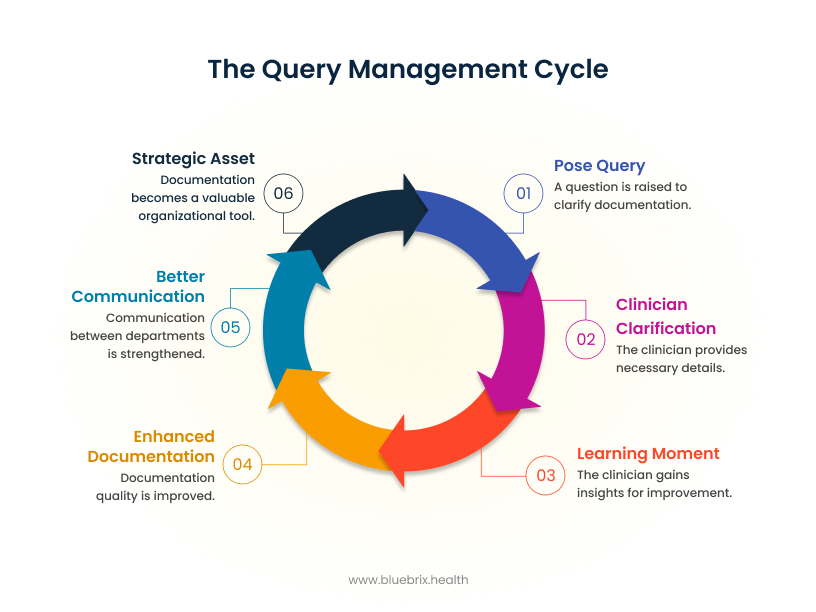
This proactive engagement directly addresses the identified documentation gaps:
- Specificity: Queries prompt clinicians to provide more specific and detailed diagnoses, moving beyond generic terms to capture the full clinical picture.
- Comorbidities: They ensure that all relevant comorbidities, both psychiatric and medical, are documented with their clinical significance and impact on the patient’s care.
- Treatment details: Queries encourage comprehensive justification for treatment plans and the medical necessity of the inpatient stay, ensuring that the intensity of services provided is clearly articulated.
- SOI/ROM: They prompt for documentation that accurately reflects the patient’s true severity of illness and risk of mortality, ensuring that all factors contributing to complexity are captured.
- Discharge planning: Queries can help ensure the rationale for the entire length of stay, including the complexities of discharge coordination and aftercare planning, is clearly documented.
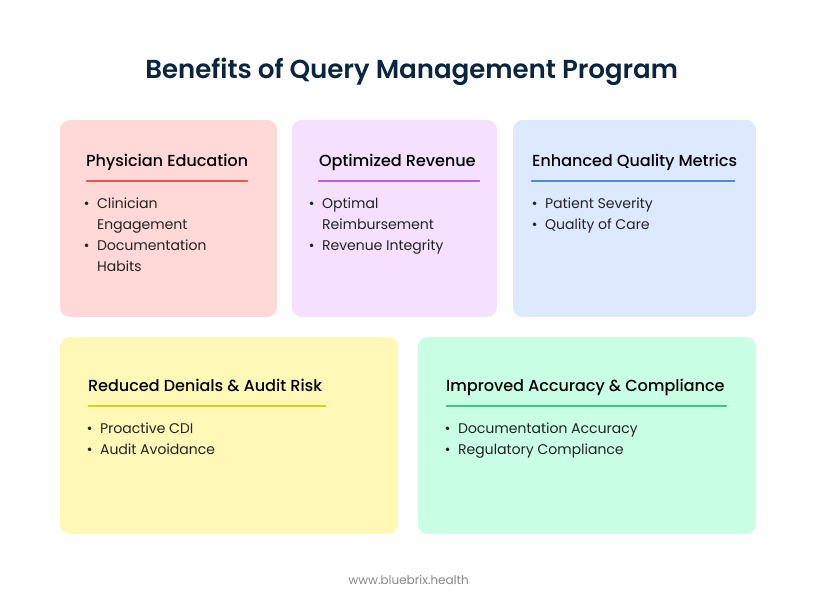
The benefits of implementing a robust query management program are multifaceted and significant:
- Improved accuracy & compliance: CDI and query management demonstrably improve documentation accuracy, ensuring that the patient record accurately reflects the severity of their condition. This leads directly to accurate DRG assignments and strengthens overall compliance with regulatory requirements. Hospitals with strong CDI programs can see up to a 25% reduction in claim denials.
- Optimized revenue: By capturing the true complexity and intensity of care, query management helps facilities achieve optimal reimbursement and effectively optimize their revenue cycle. CDI is crucial for maintaining revenue integrity, with some hospitals reporting revenue increases of as much as $1.5 million after implementing solid CDI programs. Overall, practices that address common billing mistakes can see an average revenue increase of 15-20% annually.
- Reduced denials & audit risk: Proactive CDI significantly reduces the incidence of denials and helps facilities avoid costly audits by ensuring documentation withstands scrutiny.
- Enhanced quality metrics: Accurate documentation, facilitated by CDI, improves reported quality metrics by precisely reflecting patient severity and the quality of care provided.
- Physician education: The querying process serves as a continuous, ongoing educational opportunity for clinicians. It fosters physician engagement and gradually improves future documentation habits, making it a continuous process of learning and refinement.
Query management is not merely a reactive tool for correcting documentation errors; it functions as a proactive, continuous feedback loop that significantly enhances clinical education, improves communication channels between clinicians and coders, and ultimately elevates the overall quality and integrity of a facility’s health data.
Partnering for precision: how blueBriX elevates your revenue cycle with expert medical coding
Navigating the intricate landscape of inpatient psychiatric documentation and DRG optimization can be a daunting task for even the most dedicated internal teams. This is where partnering with a specialized expert like blueBriX becomes a strategic advantage. blueBriX is a leader in healthcare Revenue Cycle Management (RCM), with a core strength rooted in expert medical coding services.
blueBriX’s specialized expertise directly helps psychiatric facilities optimize their DRGs. Their approach is comprehensive and tailored to the unique challenges of mental health documentation:
- Specialized knowledge: The blueBriX team possesses a deep and nuanced understanding of the complexities inherent in psychiatric documentation and coding. This specialized knowledge enables them to expertly navigate complex coding rules and guidelines that often prove challenging for internal teams lacking dedicated psychiatric coding expertise. In 2021, CMS reported that 54% of billing errors in mental health were due to improper CPT and ICD-10 codes, underscoring the need for specialized knowledge.
- CDI & query management implementation: blueBriX goes beyond merely identifying documentation gaps. They actively help facilities enhance their documentation practices through comprehensive Clinical Documentation Improvement (CDI) services. This includes designing and implementing effective query management programs, providing targeted training for clinical staff, developing streamlined processes, and offering ongoing support to ensure sustained improvement. Hospitals with strong CDI programs have seen up to a 20% increase in appropriate reimbursements.
- Proactive solutions: blueBriX empowers facilities to shift from a reactive stance of managing denials to a proactive strategy of documentation improvement. This forward-thinking approach ensures revenue integrity and compliance from the outset, minimizing future financial risks.
- Ongoing support & education: Recognizing that documentation excellence is a continuous journey, blueBriX provides ongoing support and education for both clinical and coding staff. This fosters a culture of documentation excellence, leading to sustained improvements in accuracy and specificity. Almost 90% of larger hospitals experienced significant gains after implementing an invigorated approach toward clinical documentation.

By partnering with blueBriX, psychiatric facilities can bridge documentation gaps, ensure accurate DRG assignment, maximize reimbursement, and significantly reduce audit and denial risks. blueBriX acts as a strategic partner, translating clinical nuances into precise codes and building systems for consistent, high-quality documentation.