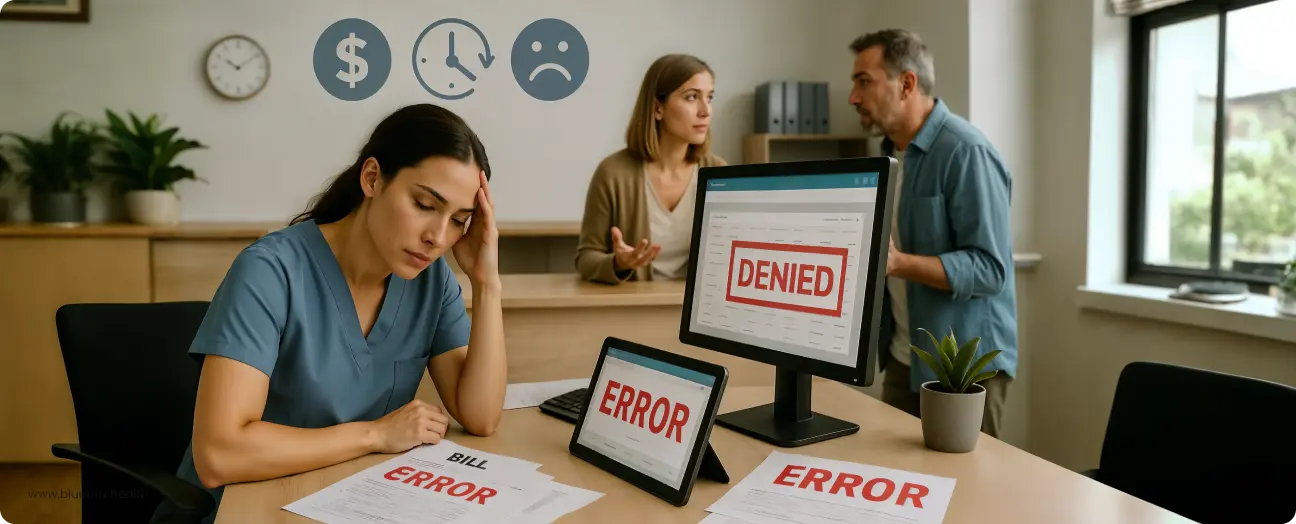
Imagine this scenario: Dr. Emily Roberts, a dedicated orthopedic surgeon, just completed a complex spinal fusion. Her team provided exceptional care, and the patient is recovering well. Yet, a few weeks later, her practice administrator, Mark, appears with a grim look. “Another denial,” he sighs, pointing to a claim for that very surgery. “The payer says the DRG wasn’t supported by the documentation, and we’re looking at a 25% reduction in reimbursement for this case alone.” This isn’t an isolated incident; it’s a recurring headache costing them hundreds of thousands annually.
This story, or one strikingly similar, plays out daily in healthcare organizations across the US. Financial stability hinges on precision, and at the heart of this precision lies Diagnosis-Related Group (DRG) coding. If you’re a healthcare provider or practice administrator, you know that navigating this complex system isn’t just about compliance; it’s about optimizing every aspect of your revenue cycle and ensuring consistent, fair reimbursement for the high-quality care you provide.
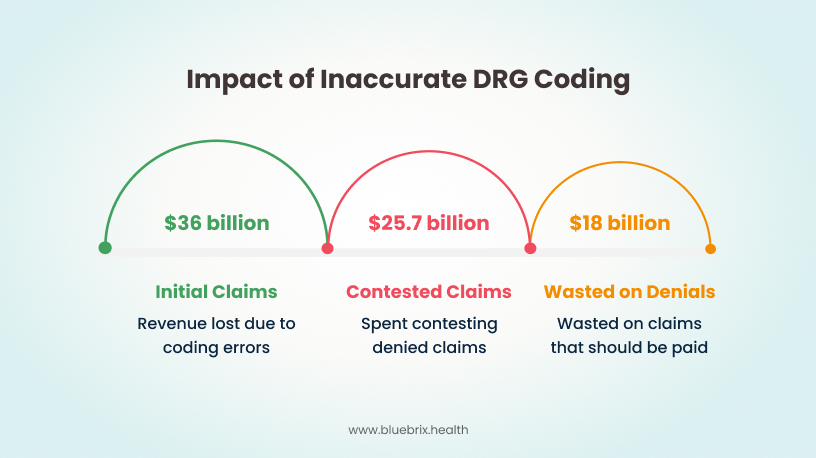
Having navigated the intricacies of medical coding for two decades, blueBriX understands these exact challenges intimately. Since 2005, we’ve collaborated with countless healthcare organizations, empowering them to achieve financial balance and operational excellence with our cutting-edge digital health solutions and RCM services. Our deep expertise isn’t just theoretical; it’s forged in the daily realities of accurate, compliant DRG coding, helping our clients avoid the staggering $18 billion that providers reportedly waste annually on overturning claims denials across the industry.
In this article, we’ll explore the nuances of DRG coding and how to master it.
Understanding the building blocks of DRG: More than just codes
So, what exactly are DRGs, and why are they so crucial?
Introduced by the Centers for Medicare and Medicaid Services (CMS) in the early 1980s, Diagnosis-Related Groups, or DRGs as they are popularly called, were designed as a standardized classification system. They group patients with comparable healthcare resource use. Think of them as a standardized way to group patients based on their medical conditions, ensuring that hospitals can track resource consumption while maintaining a sharp focus on treatment quality.
The power of DRGs lies in their foundational components, which meticulously ensure patients are classified appropriately for fair reimbursement:
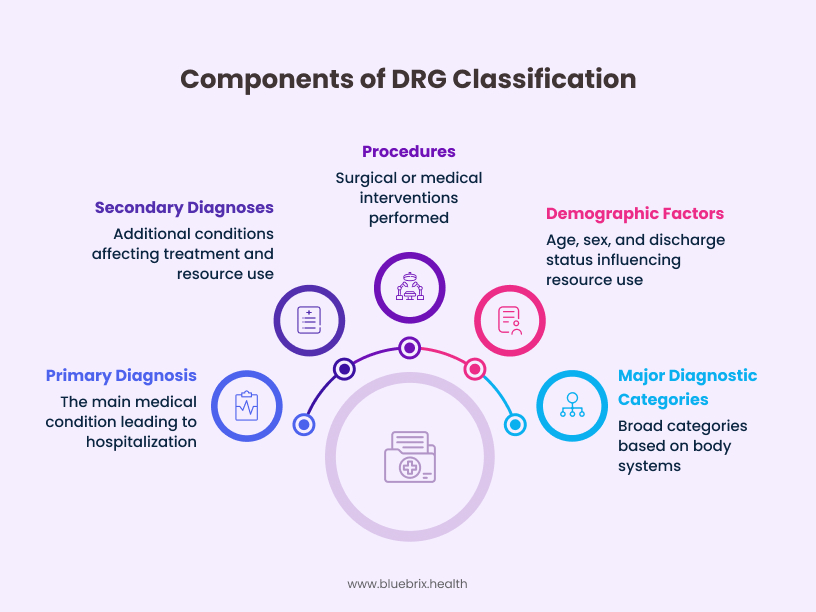
Primary diagnosis: This is the main condition that brought the patient to the hospital and was the central focus of their stay. For example, a patient admitted for acute myocardial infarction (heart attack) would have this as their primary diagnosis.
Secondary diagnoses: These are any additional conditions present at admission or that develop during the stay, significantly impacting treatment and resource use. If that heart attack patient also has chronic kidney disease, that secondary diagnosis will influence the DRG assignment and reimbursement.
Procedures: Any surgical or medical interventions performed during the hospital stay are key factors in DRG assignment. A coronary artery bypass graft (CABG) procedure, for instance, would heavily influence the DRG.
Demographic factors: Age, sex, and discharge status can subtly influence the expected resource use and outcomes, contributing to the overall DRG calculation.
Major diagnostic categories (MDCs): To maintain clinical relevance, DRGs are further organized into MDCs, which are broad categories based on the body system or cause of the primary diagnosis (e.g., Diseases and Disorders of the Circulatory System).
Why should DRG accuracy be a top priority for your organization?
Because its impact stretches far beyond a single claim and has the potential to drive a healthcare organization’s financial health and operational excellence. DRG reimbursement plays a crucial role in controlling healthcare costs for payers, offering a predictable framework for services rendered. These pre-determined diagnosis groupings are set for most common and significant inpatient encounters, ensuring consistent reimbursement. What’s truly remarkable is that these complex algorithms even allow for variability based on patient complexity, comorbidities, and can even handle extreme outlier cases.
For providers, ensuring these intricate claims are accurately coded and billed according to the actual services provided is fundamental to maintaining financial balance and preventing unnecessary expenditure on healthcare claims. Accurate DRG assignment directly translates to optimal revenue capture. Beyond the immediate financial transaction, DRGs also offer a strategic advantage: they help healthcare providers and policymakers understand patterns in resource utilization. This critical insight enables better planning, smarter allocation of healthcare resources, and more informed decisions about where to focus efforts for improvement and investment.
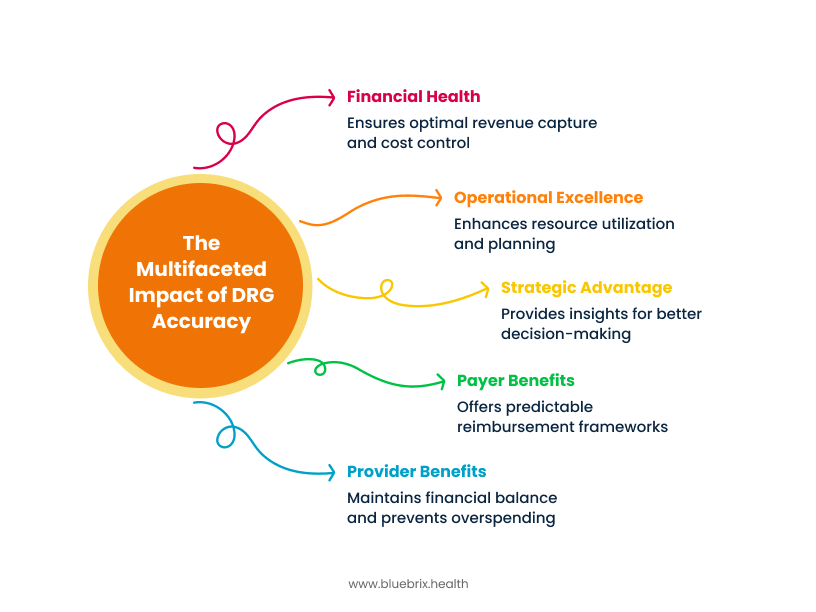
In essence, a thorough review of the DRG brings balance to the relationship between a payer’s desire for accurate payment and a provider’s need to maximize compliant reimbursement.
The high stakes: risks of inaccurate DRG coding
Ignoring DRG accuracy is akin to leaving substantial revenue on the table – or worse, opening the door to significant financial and compliance liabilities. The consequences of inaccurate DRG coding are severe and multi-faceted:
Financial impact
- Underpayments: If a DRG code fails to fully capture the patient’s severity or treatment complexity, your hospital could be significantly underpaid for the services you’ve diligently provided. For instance, a common error, like failing to adequately document and code complications, can lead to a DRG downgrade, costing your hospital thousands of dollars per patient encounter. Remember Mark, the practice administrator? His practice experienced a 38% reimbursement reduction on a femur fracture case because the initial DRG (MS-DRG 481) wasn’t fully supported by documentation, requiring an adjustment to a lower-paying DRG 482. This isn’t just theoretical; it’s a direct hit to your bottom line.
- Overpayments: On the flip side, overcoding or unsupported coding can trigger demands for repayments from insurers or Medicare, often coupled with hefty fines or penalties for noncompliance. In 2019 alone, fines from CMS for improper billing and coding reached $2.5 billion, with the Office of Inspector General imposing an additional $3.7 billion in fines. These are not minor slaps on the wrist.
Compliance risks
Incorrect DRG codes are a glaring red flag for regulatory bodies, frequently triggering audits. This scrutiny puts hospitals at significant risk of severe penalties or even exclusion from vital payer programs. A single audit can consume thousands of staff hours and lead to substantial financial clawbacks.
Operational inefficiencies & mounting costs
Beyond the immediate financial hit, inaccurate DRG codes lead to frustrating claim rejections and denials. Industry reports indicate that the average claim denial rate can range from 5% to over 10%, with some organizations experiencing rates as high as 19% for in-network claims in 2023 on HealthCare.gov plans, and even 37% for out-of-network claims. Some providers even report denial rates exceeding 15%. These denials cause significant delays in cash flow and amplify administrative burdens. Providers spent an estimated $25.7 billion in 2023 contesting claims denials, with nearly $18 billion of that potentially wasted on claims that should have been paid initially. Each denied claim adds an average of $57 in administrative costs just to contest. This means countless hours are spent on rework rather than focusing on patient care, impacting your bottom line and staff morale. Research suggests that medical coding errors can lead to staggering revenue losses, costing healthcare organizations up to $36 billion annually, with individual clinics experiencing losses of 10% to 30% of their annual earnings.
DRG validation the imperative for precision and profitability
Given these high stakes, DRG validation isn’t optional; it’s an essential safeguard for your clinic’s financial health and reputation. It’s the critical process that ensures your coded claims accurately reflect the clinical documentation and justify the resources utilized.
Accurate reimbursement
Validation ensures that the documentation truly reflects the actual severity of a patient’s illness and the complexity of their care, preventing substantial revenue loss from incomplete or inaccurate records. This means you get paid appropriately for the care you deliver. For example, a hospital that implements rigorous training programs for coding staff can see a decrease in claim denials by up to 30% within the first year.
Reducing denials
Denied claims are a significant administrative burden, consuming valuable time and resources. While it’s reported that 86% of denials are potentially avoidable, navigating the appeals process for the remaining 14% is still costly. By performing robust DRG validation, you ensure your documentation and codes are clinically valid and strictly aligned with coding guidelines, drastically reducing the risk of costly denials and appeals. Although 70% of contested denials are eventually overturned, this often occurs after multiple, costly rounds of review and significant payment delays, making prevention far more beneficial.
Compliance and audit readiness
Providers are held to rigorous standards of care and documentation. A robust DRG validation process ensures unwavering compliance with coding guidelines, significantly reducing the likelihood of audits and penalties, especially those associated with high-risk DRGs.
Quality measure performance
Many crucial hospital quality measures, including those within CMS value-based purchasing programs, are directly tied to the coded record, not just clinical outcomes. Discrepancies between the coded record and the actual patient’s condition can result in lower quality measure performance, impacting your reputation and future reimbursement.
Navigating Extreme Complexity: The Sepsis Coding Challenge
Among the myriad of coding complexities, sepsis stands out as a formidable challenge. It continues to climb the charts as one of the most frequent principal diagnoses for US hospitalizations and is among the nation’s most expensive conditions to treat. This naturally warrants intense scrutiny from payers, making sepsis-related claims one of the most frequently denied diagnoses.
The challenges in sepsis billing are rooted in several factors:
Evolving definitions: The clinical definition of sepsis has undergone significant changes over time, from early concepts like Sepsis-1 (based on SIRS) to the current Sepsis-3 definition (focusing on life-threatening organ dysfunction). This evolution, along with varying clinical indicators, creates a moving target for documentation and coding, making it difficult to keep up.
Clinical ambiguity: Diagnosing sepsis can be subjective. Patients present with diverse ailments, and organ dysfunction may or may not be due to infection. Even common diagnostic tools like the SOFA score, developed in ICU settings, may underestimate organ dysfunction outside of the ICU.
Documentation hurdles: The uncertainties in diagnosis often lead to unclear documentation that negatively impacts coding and can result in denials. Physicians must make a clear connection between abnormal clinical findings, organ dysfunction, and the sepsis diagnosis. Vague terms like “urosepsis,” “sepsis-like,” “meets sepsis criteria,” or “sepsis syndrome” are problematic and must be avoided.
Coding discrepancies: Coding sepsis is as challenging as diagnosing it because CMS guidelines haven’t always fully aligned with the latest clinical definitions. Even with guidance from sources like the AHA Coding Clinic, physician documentation doesn’t always explicitly clarify sepsis with associated acute organ dysfunction. This often necessitates queries to clarify documentation – a resource-intensive process.
Fear of missed diagnosis: There’s speculation that sepsis diagnosis might be overused due to the potentially fatal consequences of not treating a suspected case.
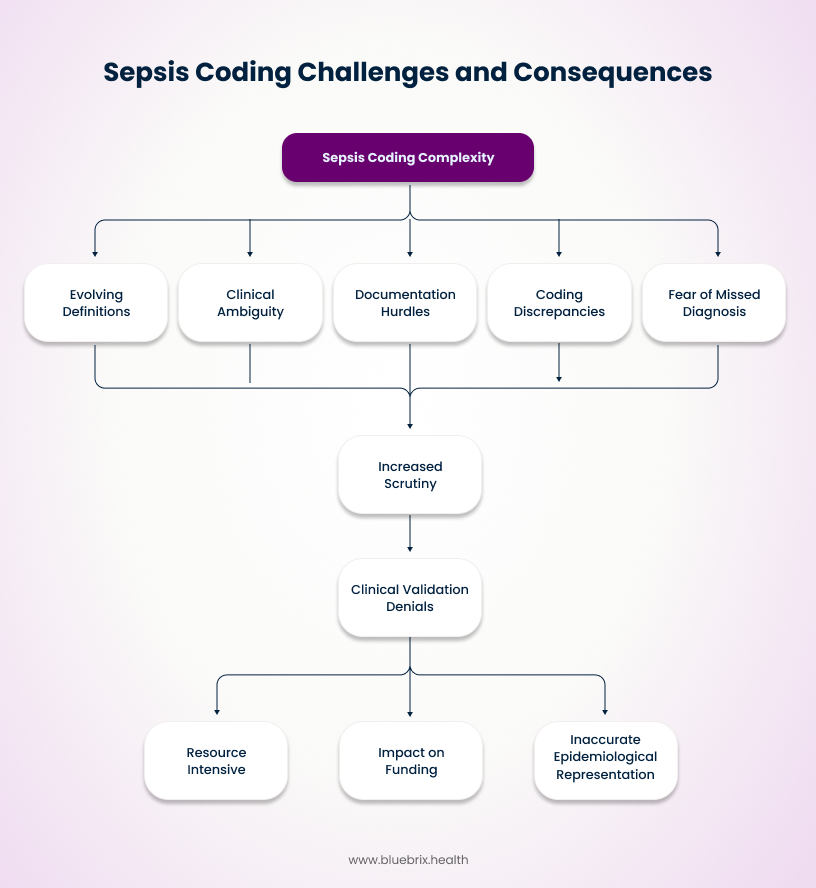
These complexities mean that MS-DRG 871 (Septicemia or severe sepsis with a major complication) is one of the most frequently billed MS-DRGs, leading payers to scrutinize these claims rigorously, often with prepayment and post-payment reviews. The consequence? Increasing clinical validation denials due to misaligned criteria between providers and payers, and insufficient documentation. These denials are expensive and resource-intensive, impacting funding and accurate epidemiological representation.
blueBriX's edge: Mastering DRG coding for unrivaled accuracy and revenue optimization
In a landscape defined by complexity and high stakes, blueBriX stands apart. Our two decades of unwavering commitment to medical coding excellence for US healthcare providers isn’t just a claim; it’s a proven track record. We understand that your success depends on a partner who delivers not just service, but a strategic advantage forged from experience and innovation.
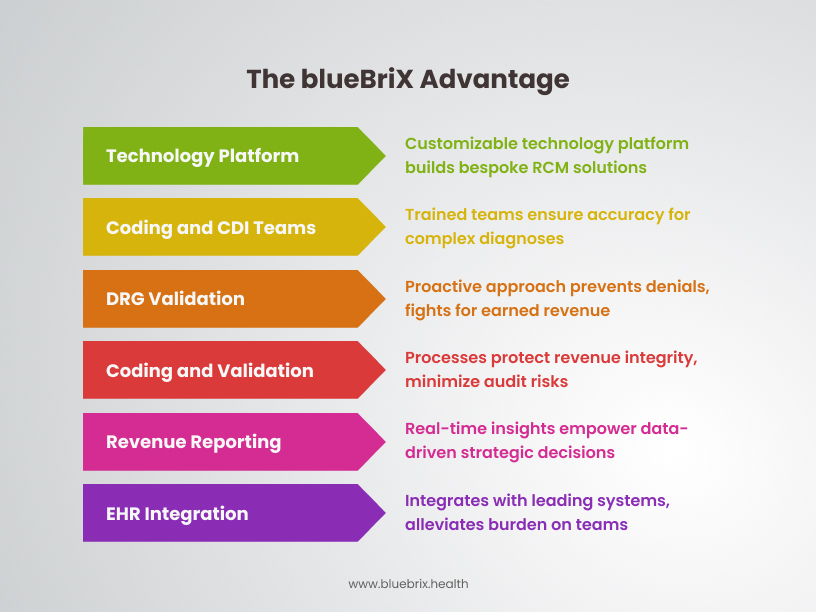
At the core of blueBriX’s enduring success is our own in-house, highly customizable, and configurable technology platform. This unique stronghold on technology sets us apart. It allows us to build bespoke Revenue Cycle Management (RCM) solutions perfectly aligned with each prospect’s distinct operational and financial requirements. This adaptability and technological prowess are key reasons why our clients choose us and remain partners for decades, knowing their unique needs will always be met.
Our specialized coding and Clinical Documentation Improvement (CDI) teams are meticulously trained on the latest definitions, clinical criteria, and payer-specific guidelines. This ensures unparalleled accuracy, especially for high-risk and complex diagnoses like sepsis, where documentation clarity is paramount. We don’t just code; we master the nuances to reflect the true severity of patient conditions, giving you peace of mind.
While the industry struggles with average denial rates often exceeding 10% and facing substantial revenue losses, blueBriX employs a strategic, proactive approach to DRG validation and denial management. We work to prevent denials at the source, and when they do occur, our expert appeal process fights for every dollar you’ve earned, drastically reducing rework and improving your accounts receivable. This saves you the average $57 administrative cost for every claim you don’t have to fight.
Our goal is to ensure you receive the maximum compliant reimbursement for services rendered, safeguarding against both underpayments and the significant risks associated with overpayments. Our rigorous coding and validation processes protect your revenue integrity and minimize the likelihood of costly audits, which are often triggered by inconsistent or inaccurate coding.
We provide clear, real-time revenue reporting and insights that empower your leadership to make data-driven strategic decisions, effectively closing reporting gaps that hinder growth. Understand your coding trends, identify areas for clinical documentation improvement, and optimize your resource allocation with precision previously unavailable.
blueBriX integrates effortlessly with leading EHR/practice management systems like Athenahealth, eClinicalWorks (eCW), NextGen, Kareo, AdvancedMD, and DrChrono. Our flexible outsourcing solution alleviates the burden on your internal billing and coding teams, addressing common challenges like staff burnout and attrition by freeing up your valuable resources to focus on patient care.