The landscape of Workers' Compensation is far more than a simple medical event; it is a sophisticated process demanding precise coordination across diverse stakeholders, each operating with their own systems, priorities, and often, isolated information. This fragmentation frequently culminates in "digital chaos", with crucial information scattered across disparate platforms, disjointed communication, and unnecessarily prolonged and frustrating path to recovery for the injured worker. The antidote to this pervasive chaos lies in the strategic adoption of a robust care coordination platform. In this blog, we explore how blueBriX’s intelligent care coordination platform helps organizations manage workers’ comp.

Navigating the Workers’ Comp Maze
Workers’ Compensation is a complex journey from injury to return-to-work, involving many stakeholders such as injured workers, employers, healthcare providers, adjusters, and legal teams. A significant challenge within this ecosystem is the lack of coordinated communication, which frequently leads to debilitating delays and inefficiencies throughout the claims process. The root of this disarray often lies in fragmented systems and manual processes, which are regrettably common practice in Workers’ Compensation administration. These outdated methods severely hinder real-time data exchange and impede collaborative decision-making, exacerbating the overall complexity of case management.
This fragmentation isn’t just inconvenient; it drives up costs, delays care, and erodes trust. When communication falters and data remains siloed, the resulting delays and inefficiencies translate directly into longer case resolution times. Poor communication alone can escalate claim costs by up to 20% due to extended disability and increased litigation. This does not simply mean more administrative work; it implies prolonged disability for the injured worker, potentially escalating medical costs due to delayed or suboptimal treatment, and increased indemnity payments. For employers, the repercussions include extended periods of lost productivity and, consequently, higher insurance premiums. As for healthcare providers, increased administrative burdens and delayed reimbursements add to their operational costs significantly. This systemic inefficiency creates an “invisible cost” that transcends direct financial outlays, eroding trust among stakeholders, fostering more disputes, and ultimately compromising the quality of care and the injured worker’s overall well-being and morale. The digital chaos is not merely an operational glitch; it represents a significant financial and human drain on the entire Workers’ Compensation system.
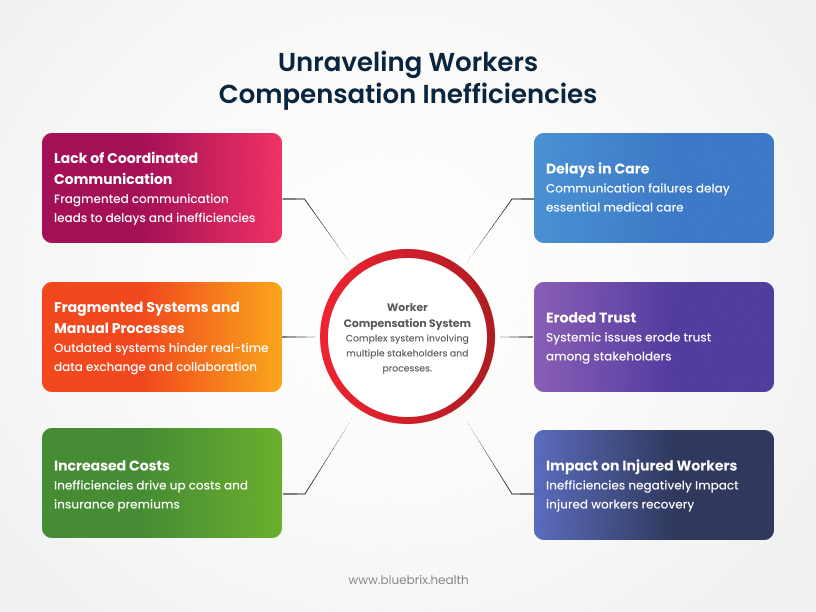
At the heart of the Workers’ Compensation system is the injured worker, whose journey is profoundly impacted by these systemic inefficiencies. When communication channels are broken and information systems are fragmented, the worker’s path becomes fraught with difficulty. This often manifests as delayed access to essential medical care, persistent confusion regarding their claim status, profound frustration with the convoluted process, and, in many cases, poorer health outcomes, including prolonged recovery periods or the development of chronic issues. The systemic inefficiencies, as documented, directly contribute to the human cost of Workers’ Compensation. Addressing these systemic failures is not just about streamlining business processes; it is fundamentally about improving the life and recovery trajectory of the injured individual, elevating the value proposition of a coordinated solution beyond mere efficiency to one of profound societal impact, especially given the constantly evolving regulatory landscape.
The Multi-Stakeholder Conundrum: Why Workers’ Comp is So Complex
The complexity of Workers’ Comp stems from diverse roles and often conflicting objectives among stakeholders.
- Injured Workers: Seek optimal recovery and timely return-to-work, but face confusing systems and communication gaps, leading to delayed RTW, increased stress, frustration, and suboptimal care.
- Employers: Aim to support employees, manage costs, and ensure compliance, often burdened by paperwork and coordinating multiple parties to understand medical progress. This can result in extended lost productivity, higher premiums, and compliance risks.
- Healthcare Providers: Deliver care, but struggle with administrative tasks, delayed authorizations, and incomplete patient histories, which can lead to delayed patient care, administrative overhead, and delayed payments.
- Adjusters: Manage claims and investigations, spending significant time chasing information and coordinating numerous parties, leading to case delays, increased workload, and reduced caseload capacity.
- Legal Teams: Resolve disputes and ensure compliance, hampered by incomplete records and difficulty verifying information, which can result in increased litigation costs and protracted disputes.
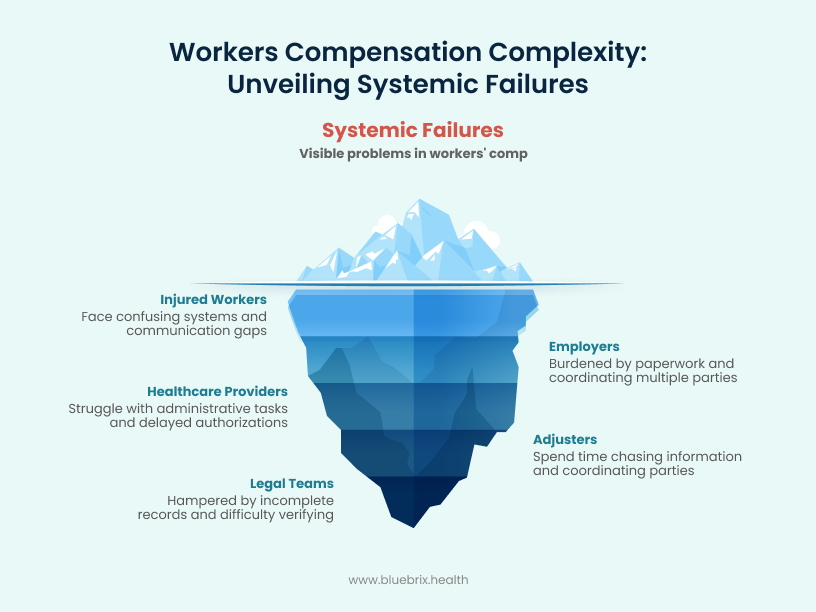
These individual challenges combine to create systemic failures. A delay in one area, like treatment authorization, cascades through the entire system, escalating costs and extending resolution times. Beyond direct financial costs, fragmented communication and data silos also pose significant regulatory and reputational risks. Litigation, while costly in itself, often signals a fundamental failure in compliance and transparency, which can attract heightened scrutiny from regulatory bodies such as state Workers’ Compensation boards, and even the Centers for Medicare & Medicaid Services (CMS) if federal programs are involved.
A history of unresolved disputes and inefficient claim management can severely damage an employer’s reputation, impacting employee morale and talent acquisition. Similarly, a provider’s standing can suffer, affecting referrals, and an adjuster’s efficiency ratings may decline. These consequences extend beyond financial penalties to encompass significant reputational and regulatory exposure, positioning a robust, auditable system as a crucial preventative measure rather than merely an efficiency tool. This is particularly pertinent as federal and state policies continue to evolve, introducing new compliance requirements and penalties.
The Evolving Workers’ Compensation Regulatory Landscape: Federal and State Trends
Workers’ compensation is a constantly evolving area of law and policy in the US, with ongoing changes at both federal and state levels impacting how claims are managed and resolved.
Federal Policies
While workers’ compensation is primarily regulated at the state level, federal programs exist for specific employee groups. Recent federal activity largely focuses on:
- Federal Employees’ Compensation Act (FECA): This is the federal workers’ compensation program. Recent legislative changes impacting FECA include:
- COVID-19 Presumption (American Rescue Plan Act of 2021): This act created a presumption of eligibility for FECA benefits for federal employees who contracted COVID-19 within a specific period (January 27, 2020, to January 27, 2023), provided they had public or coworker contact. This presumption is currently scheduled to terminate on September 30, 2030.
- Presumptive Conditions for Federal Firefighters (James M. Inhofe National Defense Authorization Act for Fiscal Year 2023): This act established a list of cancers and other medical conditions presumed to be employment-related for federal firefighters, allowing the Secretary of Labor to add conditions through rulemaking.
- Civil Monetary Penalties Inflation Adjustment: The U.S. Department of Labor regularly adjusts civil monetary penalties for inflation, which can impact various programs, including those administered by the Office of Workers’ Compensation Programs (OWCP). These adjustments typically occur annually.
- Electronic Filing Requirements: The Department of Labor has been moving towards requiring electronic filing in proceedings before the Benefits Review Board (BRB), aiming to streamline processes.
- Updated Criteria for Specific Programs: The OWCP has published final rules to update criteria for programs like the Energy Employees Occupational Illness Compensation Program Act, particularly regarding beryllium sensitivity.
State Policies
Workers’ compensation laws and regulations vary significantly by state. However, common themes and recent developments across states include:
- Emphasis on Data Integrity and Interoperability(influenced by CMS guidelines) : There’s a growing focus on the importance of robust audit trails for compliance, dispute resolution, and fraud prevention within broader healthcare systems, which extends to Workers’ Compensation. This suggests a push for greater data transparency and accountability.
- Medical Treatment Guidelines and Fee Schedules: Many states are continually reviewing and updating their medical treatment guidelines and medical fee schedules to manage costs and ensure appropriate care. For example, Colorado has adopted rules for medical fee schedules and utilization standards effective in 2025.
- Dispute Resolution Processes: States are often looking for ways to improve efficiency and fairness in dispute resolution. Colorado, for instance, has adopted rules effective January 1, 2024, regarding dispute resolution.
- Specific Industry or Injury Focus: Some states are addressing specific worker populations or types of injuries.
- New York (Effective January 1, 2025): Notably, New York’s workers’ compensation law now covers “mental injury” premised on extraordinary work-related stress for all workers, a significant expansion from previous provisions that primarily covered a subset of first responders.
- New York (Effective 2025): Also, new legislation in New York focuses on reducing musculoskeletal injuries and disorders among workers in manual materials handling jobs, requiring employers to implement injury reduction programs, worksite evaluations, and provide training.
- Electronic Submissions: Several states are mandating or encouraging electronic submissions for claims and related documentation, as seen with New York’s CMS-1500 electronic submission requirement in July 2025.
- Market Dynamics and Cost Control: States continuously monitor the workers’ compensation insurance market, considering factors like wage inflation, medical inflation, and claim frequency to adjust rates and ensure system solvency. There’s an ongoing effort to balance fair benefits for injured workers with manageable costs for employers.
- Fraud Prevention: The utility of audit trails and other measures for fraud prevention remains a significant concern and focus for state workers’ compensation boards.
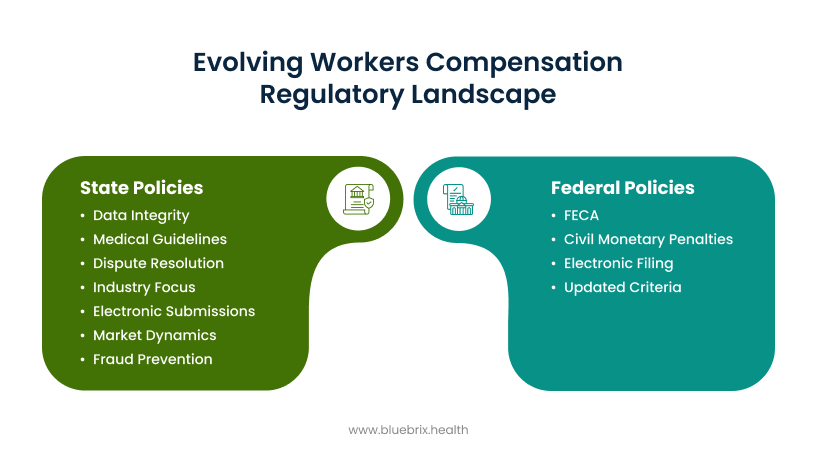
It’s crucial to remember that each state has its own unique workers’ compensation statutes and regulations.
The Blueprint for Harmony: Orchestrating Workflows with a Care Coordination Platform
The average claim resolution can take months, even years, highlighting the urgent need for better coordination. A robust care coordination platform is the strategic answer, transforming reactive, fragmented processes into proactive, integrated workflows for better outcomes and reduced burdens for all.
A sophisticated care coordination platform transforms Workers’ Comp by proactively managing tasks, securely sharing information, and automating workflows. It establishes a single, authoritative source of truth for all authorized stakeholders.
Key Orchestration Features
- Collaborative Task Management: Assign, track, and manage specific tasks for each stakeholder within a unified system, ensuring accountability and progress.
- Real-Time, Secure Communication: Facilitates HIPAA-compliant messaging, document sharing, and notifications, replacing cumbersome traditional methods and reducing delays.
- Centralized Information Hub: Stores all pertinent documents, including medical records, claim forms, detailed treatment plans, and critical authorizations, are stored in a single, easily accessible, and version-controlled location. This eliminates the pervasive problem of information silos and guarantees that every stakeholder is working from the most current and accurate case information. This directly counters the fragmentation and information scattering that characterize digital chaos, and supports compliance with evolving electronic submission mandates.
- Automated Workflows and Reminders: The platform can automate routine administrative tasks and trigger timely notifications based on predefined milestones. Examples include alerts for an approaching return-to-work date or an expiring treatment authorization. This automation guides users through complex processes, substantially reducing manual effort and minimizing the potential for human error. This feature specifically addresses the administrative burdens faced by healthcare providers and adjusters, allowing them to redirect their focus towards more critical, value-adding activities, while also ensuring adherence to state-specific timelines and reporting requirements.
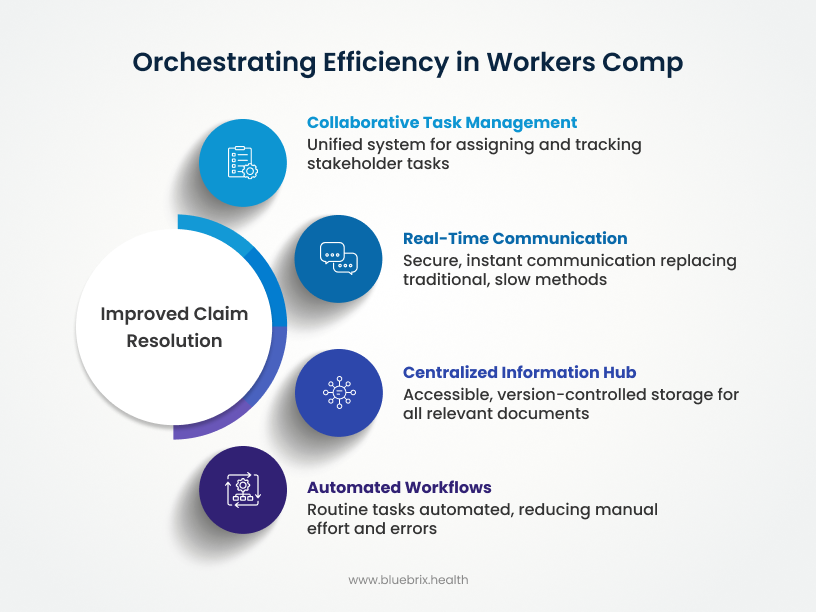
These features shift operations from reactive problem-solving to proactive prevention. Automated reminders, centralized data, and shared tasks prevent issues from escalating, reducing disputes and overall claim costs. This transparency fosters trust, empowers informed decisions, and fundamentally reshapes Workers’ Comp management.
Building Trust and Transparency: The Indispensable Role of Audit Trails
In a highly regulated environment like Workers’ Comp, robust audit trails are crucial. They provide an immutable record of all activities, communications, and decisions, ensuring compliance and effective dispute resolution.
Audit trails can transform the system into one founded on transparency and accountability, significantly lowering overall risk and ensuring long-term operational stability. Furthermore, robust audit trails future-proof organizations against evolving healthcare data standards, aligning Workers’ Compensation processes with broader compliance efforts, which is a significant advantage, particularly for healthcare providers.
How Robust Audit Trails Protect All Parties and Ensure Regulatory Adherence
- For Employers & Adjusters: Audit trails provide verifiable proof of compliance, serve as evidence in disputes, and aid in fraud detection.
- For Healthcare Providers: They offer clear documentation of care decisions, traceable communication, and protection against malpractice claims.
- For Legal Teams: Access to verifiable facts streamlines discovery, reducing time and resources spent on litigation.
- For Injured Workers: Audit trails provide transparency into case progress and protection of their rights.
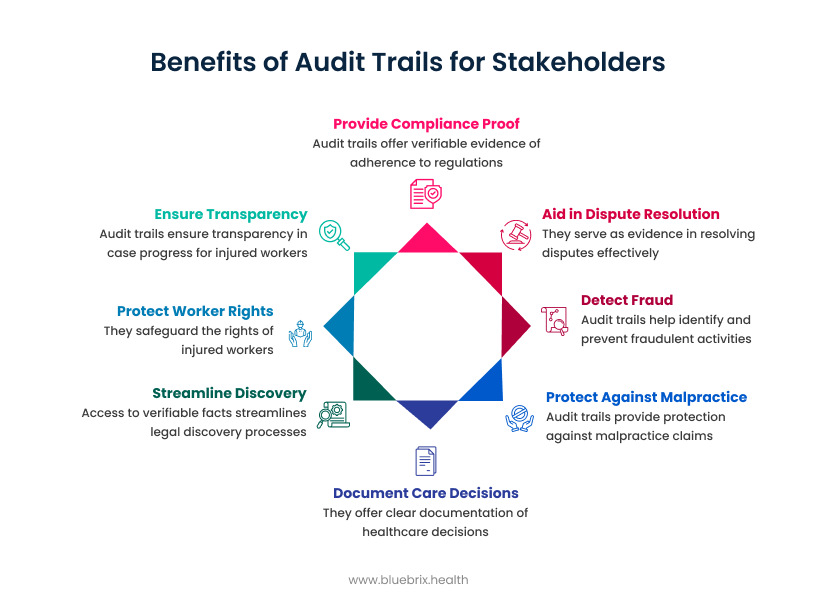
Recent CMS guidelines increasingly emphasize data integrity and interoperability. This makes robust audit trails an essential component for compliance within broader healthcare systems, a requirement that extends its influence to Workers’ Compensation processes, especially for claims involving federal programs or specific data sharing mandates. This regulatory imperative underscores that audit trails are not merely a best practice but a necessary element for modern Workers’ Compensation management.
The prevalence of disputes further highlights this need; in 2022, approximately 15% of Workers’ Comp claims involved some form of dispute, clearly demonstrating the critical need for clear, verifiable records. These audit trails are crucial for navigating the complex and evolving regulatory landscape, including new presumptions for specific conditions or industries, and ensuring all parties meet their obligations.
The blueBriX Advantage: A Unique Perspective on Solving Digital Chaos
blueBriX offers a distinct advantage through its flexibility and integration-agnostic approach. Unlike rigid solutions, blueBriX seamlessly connects with existing EHRs, claims management systems, and payroll software, avoiding costly overhauls. This “integration-agnostic” nature bridges existing silos, creating a powerful network effect that unifies disparate systems.
The blueBriX platform is engineered for integration-agnostic deployment, enabling seamless connections with existing Electronic Health Records (EHRs), claims management systems, and payroll software. This directly addresses the common pain point of organizations being forced to abandon or replace their significant investments in existing systems, making blueBriX a far more attractive and less disruptive solution. Furthermore, the platform’s inherent flexibility allows for extensive customization of workflows, ensuring that it can be precisely tailored to fit specific organizational needs and comply with unique regulatory requirements. This means blueBriX is not a one-size-fits-all solution but a highly adaptable tool, crucial for navigating the diverse and often idiosyncratic Workers’ Compensation landscape, including adapting to new state-specific mandates like mental injury coverage or electronic submission requirements.
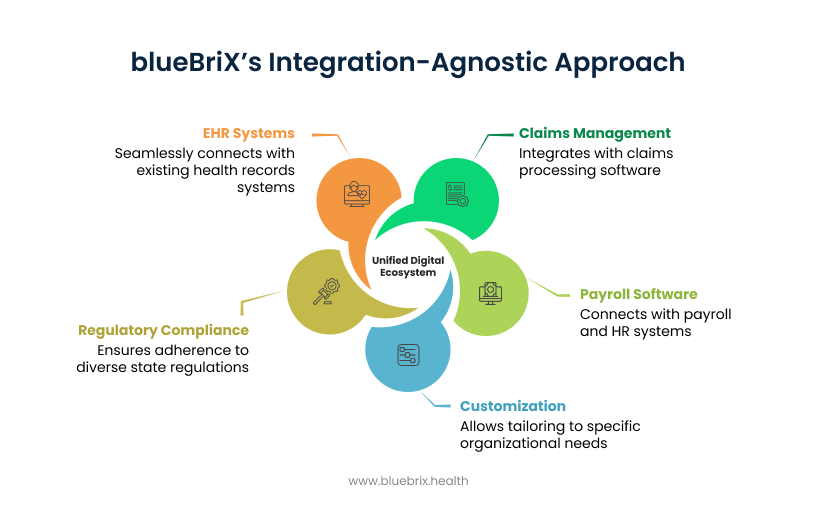
The integration-agnostic nature of blueBriX also means that organizations are not required to discard their current IT investments. This flexibility allows blueBriX to rapidly connect disparate systems, thereby creating a powerful “network effect” where the value of the platform grows exponentially with each new integration. Instead of merely adding another silo to an already fragmented environment, blueBriX serves as the essential bridge between existing silos. This capability is particularly critical in the Workers’ Compensation ecosystem, where various providers, employers, and adjusters often utilize a myriad of different systems. This integration-agnostic approach directly combats digital chaos by unifying existing digital assets rather than contributing to further complexity. It translates into faster adoption rates, lower implementation costs, and a significantly higher probability of achieving true, enterprise-wide care coordination, positioning blueBriX as a genuinely disruptive solution in a market often hindered by proprietary and closed systems. This adaptability is vital for organizations operating across multiple states, ensuring they can seamlessly comply with varying regulations and new legislative changes.
Real-World Examples Demonstrating blueBriX’s Possibilities Across Different Scenarios
To illustrate the tangible impact of blueBriX, consider these potential use-cases:

Use-Case 1: Expediting Initial Injury Reporting & Provider Referral
- Scenario: An employee sustains a workplace injury. An employer can utilize blueBriX’s automated intake forms to submit the First Report of Injury. The platform can instantly notify the designated occupational health provider, who can immediately access all relevant employer information and efficiently schedule the injured worker’s first appointment. All these interactions occur within a secure, auditable thread, ensuring transparency and compliance.
- Potential Impact: Organizations could reduce their initial injury reporting time by an impressive 40% by leveraging blueBriX’s automated intake forms and instant notification capabilities.

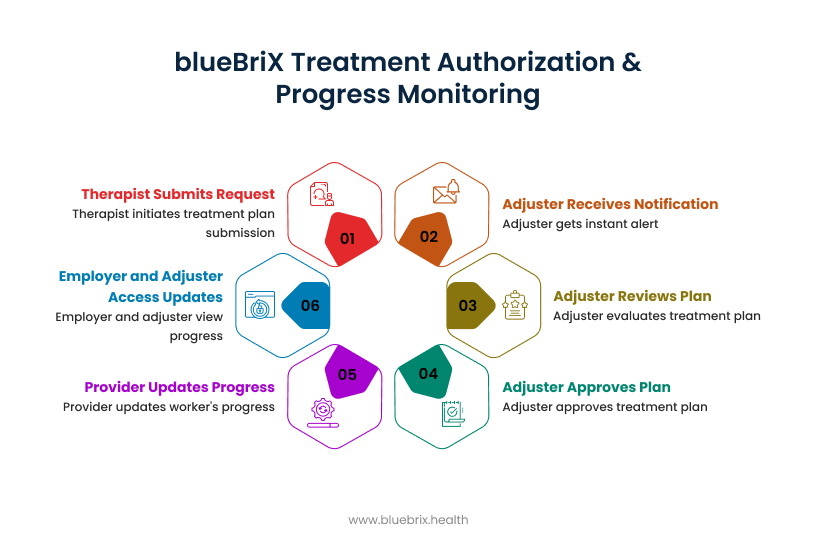
Use-Case 2: Streamlining Treatment Authorization & Progress Monitoring
- Scenario: A physical therapist determines that a new treatment plan is necessary for an injured worker. They can submit the request directly through blueBriX. The adjuster would receive an instant notification, review the proposed plan, and provide approval directly within the platform. Subsequently, the provider could update the worker’s progress notes, which would be immediately accessible to both the employer and the adjuster, eliminating any information lag.
- Potential Impact: blueBriX’s platform could facilitate up to 25% reduction in treatment authorization times, significantly accelerating the delivery of necessary care.
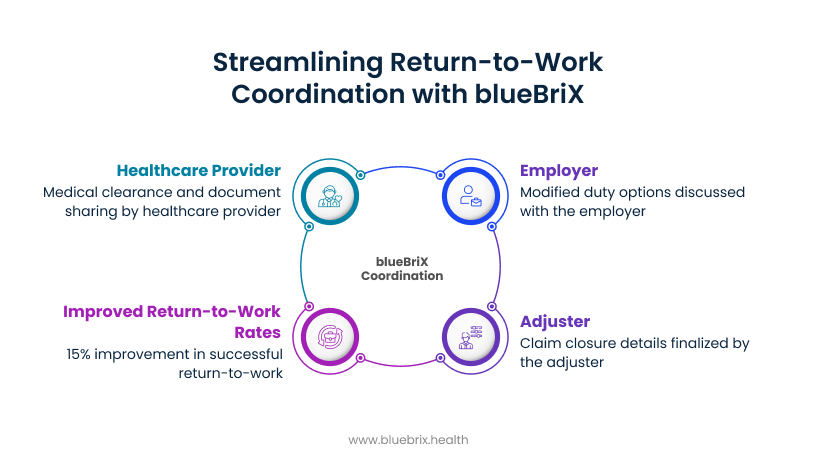
Use-Case 3: Facilitating Return-to-Work Coordination:
- Scenario: As the injured worker approaches their return-to-work date, blueBriX can seamlessly coordinate communication among the healthcare provider (for medical clearance), the employer (for discussing modified duty options), and the adjuster (for finalizing claim closure details). All parties can share essential documents and provide real-time updates within the platform, ensuring a smooth and timely transition back to the workplace.
- Potential Impact: Employers implementing blueBriX could see up to 15% improvement in successful return-to-work rates, directly attributable to the enhanced coordination facilitated by the platform.
Measuring Success: The Tangible Benefits of Streamlined Workflows
Streamlined workflows deliver concrete, measurable outcomes across all stakeholders.
- For Injured Workers: Improved satisfaction and recovery outcomes are achieved through faster access to care and clearer, consistent communication.
- For Employers: They can expect a 10-15% reduction in overall Workers’ Comp claim costs, primarily through faster return-to-work rates and reduced litigation. This also translates to lower insurance premiums and increased workforce productivity.
- For Healthcare Providers: A remarkable 30% decrease in the administrative time spent on Workers’ Compensation cases, freeing up valuable clinical time and often resulting in faster payments.
- For Adjusters: With automated tasks and centralized data, adjusters can manage up to 20% more claims with the same resources, leading to increased caseload capacity and faster claim resolution.
- For Legal Teams: They experience a significant 20% reduction in the time spent on discovery for disputed claims, a direct result of comprehensive audit trails, leading to decreased legal spend.

These quantifiable benefits yield a holistic ROI, improving employee morale, optimizing clinical outcomes, and freeing up resources for strategic initiatives. blueBriX transforms a historically contentious process into a smoother, more collaborative journey.
The Future of Workers’ Comp: Embracing Intelligent Coordination
The fragmented approach to Workers’ Compensation is unsustainable. The future demands intelligent, integrated coordination. Digital transformation is a strategic imperative for efficiency, compliance, and superior outcomes. This is especially true as federal and state policies continue to introduce new requirements and complexities. Organizations that fail to adopt advanced care coordination platforms risk higher costs, longer claim resolution times, increased disputes, and competitive disadvantage.
blueBriX offers a clear path to competitive advantage in this critical sector.
Conclusion: Transform Your Workers’ Comp Workflow Today
The Workers’ Comp journey, often mired in digital chaos, can be transformed into a streamlined, transparent, and efficient process through intelligent care coordination.
blueBriX offers a unique, flexible, and integration-agnostic solution. It empowers healthcare providers, employers, adjusters, and legal teams to orchestrate tasks seamlessly, fostering real-time collaboration and ensuring transparency through comprehensive audit trails. By adopting blueBriX, organizations can significantly reduce claim costs, accelerate return-to-work rates, alleviate administrative burdens, and ultimately, ensure optimal outcomes for every injured worker, all while navigating the dynamic landscape of federal and state workers’ compensation regulations.
Ready to transform your Workers’ Comp workflows from a labyrinth of digital chaos into a streamlined, transparent, and highly efficient journey?