How many hospitals are getting paid for the complexity of care they actually provide?
Consider the premature baby who requires weeks of NICU care with specialized monitoring, ventilation support, and dedicated nursing—yet your hospital receives the same reimbursement as a routine newborn admission, which barely covered half the costs. This is exactly the type of payment inequity that APR-DRG (All Patient Refined Diagnosis Related Group) was designed to eliminate. APR-DRG (All Patient Refined Diagnosis Related Group) changes this dynamic—it’s a sophisticated classification system designed to give your hospital appropriate credit for treating complex and high-risk patients.
By incorporating detailed measures of illness severity and risk of mortality, APR-DRG ensures your reimbursement aligns more closely with actual resource use and clinical challenges. Let’s see how APR-DRG makes this happen.
Evolution of patient classification: the rise of APR-DRG
APR-DRG (All Patient Refined Diagnosis Related Group) is a patient classification system that groups hospital inpatients based on diagnosis, severity of illness, and risk of mortality. Developed by 3M Health Information Systems, APR-DRG evolved from earlier DRG systems to provide more detailed patient acuity assessment and address limitations in previous models, particularly for pediatric and high-risk cases.
Widely used by Medicaid programs, commercial insurers, and hospitals across the U.S., APR-DRG supports fair reimbursement, quality measurement, and resource management. The system enables hospitals to categorize cases more precisely, ensuring classification accurately reflects patient complexity and actual resource requirements.
What makes APR-DRG different from other DRGs?
The All Patient Refined Diagnosis Related Group (APR-DRG) system represents a more advanced approach to patient classification in hospital settings. While traditional DRG systems focus primarily on the principal diagnosis with basic severity considerations, APR-DRG takes a comprehensive view of patient complexity. This system recognizes that patients with the same diagnosis can have vastly different care requirements based on their overall health status, comorbidities, and illness severity, ensuring your hospital receives appropriate reimbursement that reflects the true complexity of care provided.
Key differentiators
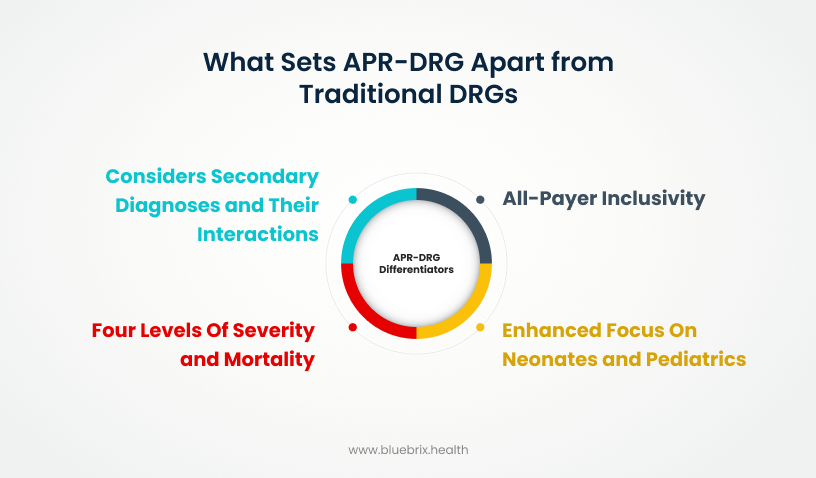
All-payer inclusivity
APR-DRG is designed to classify all patient populations—adults, children, newborns, and obstetric cases—rather than limiting classification to specific age groups or payer categories. This comprehensive approach makes the system applicable across Medicaid, commercial insurance plans, and other payer types, providing your hospital with a unified classification framework that has broader reach and applicability than traditional DRG systems.
Four levels of severity and mortality
Each patient case receives assignment to a base DRG according to their primary diagnosis, then undergoes further classification into one of four distinct levels for both Severity of Illness (SOI) and Risk of Mortality (ROM): minor, moderate, major, or extreme.
Let’s dive into each one in detail:
- Minor: The patient has a relatively stable condition; minimal organ dysfunction and low treatment intensity. For example, a patient admitted for a simple pneumonia without complications.
- Moderate: The patient shows a moderate level of physiological disruption, perhaps requiring increased monitoring or intervention. For example, pneumonia with mild dehydration or controlled diabetes as a secondary condition.
- Major: The patient has serious complications or comorbidities that significantly impact care. For instance, pneumonia complicated by heart failure or respiratory failure needing ICU care.
- Extreme: The highest level, reflecting severe physiological compromise with multiple organ failures or critical conditions. For example, pneumonia with septic shock requiring mechanical ventilation and intensive life support.
Considers secondary diagnoses and their interactions
APR-DRG systematically evaluates the impact of all secondary diagnoses rather than limiting assessment to a predetermined list of complications. The system analyzes how various medical conditions interact with each other to influence patient outcomes and resource requirements, providing your hospital with a more comprehensive understanding of patient complexity that translates to appropriate reimbursement levels.
Enhanced focus on neonates and pediatrics
APR-DRG includes specialized, detailed classification groups specifically designed for newborns, neonates, and pediatric patients, addressing the limitations of traditional DRG systems that often apply generalized approaches to these unique populations. This focused classification ensures your hospital receives more accurate reimbursement for complex pediatric cases that require specialized care, equipment, and expertise that differ significantly from adult patient needs.
Understanding how APR-DRG measures case mix and acuity
You see it every day—your facility treats a wide variety of patients, from those with minor problems to others with very serious, complex illnesses. Your “case mix” describes this blend, showing the range and complexity of patients your hospital cares for, while “acuity” simply means how sick those patients are.
You know it’s critical for payment systems to recognize these differences because caring for your sicker or more complex patients takes more time, resources, and expertise from your teams. By grouping patients based on both their condition and their level of sickness, the APR-DRG system ensures your hospital gets paid more fairly when you treat those tougher cases that require the extra work your staff puts in every day.
APR-DRG relative weights: what they mean for hospital reimbursement
Every patient who walks through your doors gets a “difficulty score”—that’s essentially what relative weights are. Each APR-DRG gets a weight that reflects how much work and resources that patient needs compared to average.
For example, let’s say you have two patients:
Patient 1: Simple pneumonia case with no complications = weight of 1.0 (average resources)
Patient 2: Pneumonia with diabetes, heart failure, and requiring ICU care = weight of 2.3 (more than double the resources)
Your payment is simple math: Base rate × Relative weight = Your reimbursement.
If your base rate is $5,000:
- Patient 1: $5,000 × 1.0 = $5,000 payment
- Patient 2: $5,000 × 2.3 = $11,500 payment
Patient 2’s higher payment reflects the reality—they needed more nursing hours, longer stay, ICU resources, and specialized care your team provided.
Key components of the APR-DRG payment methodology
Let’s break down the key pieces that make up how your hospital gets paid under APR-DRG. From the base payment tied to patient complexity, to special adjustments for short stays, transfers, or high-cost cases—each component plays a role in making sure your hospital is fairly compensated for the care you deliver.
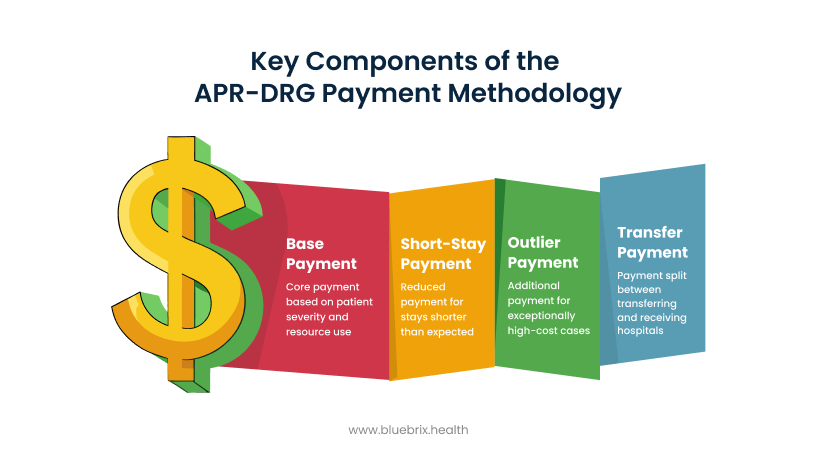
Base payment
This is the core payment the hospital receives for each patient’s stay. It is calculated based on a base rate multiplied by the APR-DRG’s relative weight, which reflects the patient’s severity and expected resource use. Policy adjustments may apply (e.g., for trauma centers or neonatal cases).
Short-stay payment
For inpatient stays shorter than expected (below a defined length of stay for the specific APR-DRG), a per diem or reduced payment may be given instead of the full base payment. This avoids overpaying for very short, less resource-intensive stays.
Outlier payment
If a hospital’s cost for a patient is exceptionally high—much higher than typical for the APR-DRG assigned—an additional “outlier” payment is made to help cover these extraordinary costs, ensuring hospitals won’t face financial losses for very complex cases.
Transfer payment
When a patient is transferred from one hospital to another, payments are split accordingly: the receiving hospital gets the full APR-DRG payment, while the transferring hospital is typically paid based on the length of stay relative to the expected average length for that DRG.
Why APR-DRG payments are critical to hospital financial health and quality care
Let’s talk about why APR-DRG payments are so critical to your hospital’s financial health and quality of care. This isn’t just about reimbursement—it’s about making sure the complexity of the patients you treat is properly recognized and reflected.
Financial fairness
APR-DRG ensures your hospital receives payments that accurately reflect the complexity and severity of your patients. When you treat sicker or more complicated patients, you receive higher reimbursements that cover the extra nursing hours, specialized equipment, and additional staff time these cases require.
This system prevents both undercharging for resource-intensive cases and overcharging for routine care. You’re appropriately compensated for every service and resource you provide, helping your hospital maintain financial stability while continuing to care for the most challenging patients that other facilities might decline to treat.
Incentives for good patient care
APR-DRG creates a direct connection between accurate clinical documentation and appropriate reimbursement for your hospital. This system incentivizes your clinical teams to thoroughly document and treat all aspects of each patient’s condition, encouraging comprehensive, high-quality care, particularly for patients with multiple comorbidities.
When your staff properly documents patient complexity and severity, your hospital achieves two critical outcomes: improved patient care and appropriate reimbursement that reflects the actual level of services provided. This alignment between documentation accuracy and payment fairness supports both clinical excellence and your hospital’s financial sustainability.
Crucial documentation and operational practices for maximizing APR-DRG payments
Let’s explore the four essential practices to maximize APR-DRG reimbursement: thorough clinical documentation, regular chart audits, concurrent coding specialists, and clear communication between coders and clinicians in detail.
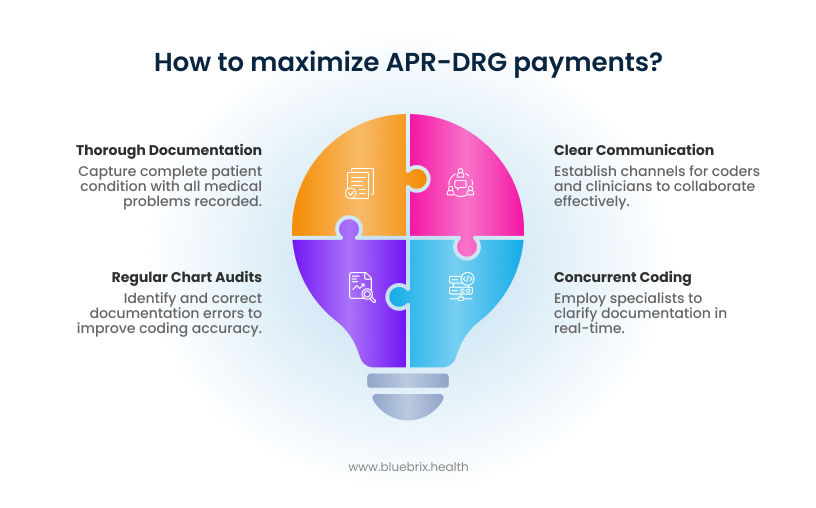
Keep clinical documentation thorough and specific
Your clinical documentation must capture the complete picture of each patient’s condition, with all medical problems—particularly secondary diagnoses and comorbidities that impact care—clearly and comprehensively recorded.
For instance, when a patient presents with pneumonia but also has diabetes, both conditions must be properly documented to reflect the full complexity and severity of their illness, ensuring your hospital receives appropriate reimbursement that accurately reflects the resources and expertise required for comprehensive patient management.
Perform regular chart audits
Regular chart audits are essential for identifying missed clinical details or complications that may not have been properly documented during the initial patient encounter. These systematic reviews help improve coding accuracy and prevent revenue loss that occurs when case severity is underestimated due to incomplete documentation, ensuring your hospital captures the full complexity of patient care provided.
Use concurrent coding or documentation specialists
Employing coders or clinical documentation specialists who work alongside your clinical teams during active patient care allows for real-time clarification of documentation questions and coding requirements. This concurrent approach reduces coding errors and ensures your documentation accurately reflects the patient’s evolving condition and treatment complexity, leading to more precise APR-DRG assignment and appropriate reimbursement.
Encourage clear communication between coders and clinicians
Establish clear communication channels that enable coders to easily consult with physicians and nurses when documentation requires clarification or additional detail. This collaborative approach prevents misunderstandings, ensures all relevant conditions and complications are properly recorded, and facilitates accurate APR-DRG assignment that reflects the true complexity of patient care your hospital provides
Partnering with blueBriX: stay ahead of the curve in APR-DRG payments
In the complex world of APR-DRG payments, partnering with blueBriX gives your hospital a clear advantage. Here’s how we help you stay ahead:

Expert coding team with specialists
Our highly skilled coding professionals and clinical documentation specialists possess comprehensive expertise in APR-DRG systems, ensuring your hospital’s documentation and coding processes are precise and optimized to capture the full complexity of patient care for appropriate reimbursement levels.
Technology-driven solutions
We utilize advanced technology platforms to enhance coding accuracy, automate complex documentation processes, and deliver real-time analytics that enable your hospital to maintain operational efficiency while staying informed about coding performance and reimbursement optimization opportunities.
Strong payer relationships built over two decades
Through nearly two decades of healthcare industry experience, blueBriX has cultivated trusted, long-standing relationships with major payers that facilitate expedited claim approvals and streamlined payment processes. These established connections reduce reimbursement delays and improve your hospital’s cash flow, while our deep understanding of payer requirements minimizes claim denials and creates a more efficient financial operation for your organization.
Advanced documentation support
blueBriX leverages cutting-edge documentation tools and technology to ensure every patient’s clinical details are captured accurately and comprehensively. Our solutions help simplify and standardize documentation workflows, reduce errors, and enhance real-time coding accuracy. By combining advanced tools with expert clinical knowledge, we help your hospital maximize the accuracy of APR-DRG assignments and secure fair reimbursement faster.

