The healthcare landscape is in constant flux, shifting from traditional fee-for-service models towards value-based care. This paradigm shift emphasizes patient outcomes, quality of care, and cost-efficiency over the volume of services provided. At the heart of this transformation lie Risk-Sharing Arrangements (RSAs), mechanisms designed to align incentives among healthcare stakeholders and drive better results.
In this environment, data has emerged as the lifeblood of effective healthcare. From electronic health records to claims data and public health registries, the sheer volume of information available is too much to handle. However, merely collecting data isn’t enough; the true power lies in its intelligent utilization to inform decisions, improve processes, and, critically, optimize financial and clinical outcomes.
Understanding risk-sharing arrangements
Risk-sharing arrangements are contractual agreements between healthcare entities—typically payers (insurers), providers (hospitals, physician groups), and sometimes pharmaceutical companies—that link financial incentives or penalties to specific performance metrics. The core idea is to share the financial risk and reward associated with patient care, encouraging all parties to work collaboratively towards shared goals like improved health outcomes and reduced costs.
Types of risk-sharing models
RSAs manifest in various forms, often blending financial and clinical outcomes:
- Outcome-based models: These models tie payments to the achievement of specific clinical outcomes, such as reduced readmission rates, improved chronic disease management, or successful adoption of preventive care. For example, a pharmaceutical company might offer a discount on a drug if it doesn’t achieve a certain efficacy rate in a patient population.
- Financial-based models: These focus on cost targets. Examples include:
- Bundled payments: A single payment covers all services for a defined episode of care (e.g., a knee replacement). If costs are lower than the bundled payment, providers share in the savings; if higher, they absorb the excess.
- Accountable care organizations (ACOs): Groups of providers take responsibility for the overall cost and quality of care for a defined patient population. They share in savings if they meet quality targets and keep costs below a benchmark but may incur losses if costs exceed it.
- Shared savings/losses: Similar to ACOs, these models involve setting a target cost for a patient population. If actual costs come in under the target, both payer and provider share the savings. If costs exceed the target, the provider may share in the losses.
Stakeholders involved: payers, providers, and pharma
The success of RSAs hinges on the collaboration of key stakeholders:
- Payers: Insurers and government programs (like Medicare/Medicaid) are keen to reduce healthcare expenditures while ensuring quality. RSAs allow them to shift some financial risk to providers and incentivize efficiency.
- Providers: Hospitals, physician groups, and individual practitioners are increasingly participating in RSAs to demonstrate their value, improve care coordination, and potentially earn additional revenue through shared savings.
- Pharma: Pharmaceutical companies are exploring outcome-based agreements for high-cost drugs, where payments are linked to the drug’s effectiveness in real-world settings.
Why optimization matters in value-based care models
Optimization of RSAs is crucial because:
- Fairness: Ensuring that risk and reward are allocated equitably among stakeholders based on accurate data.
- Sustainability: Designing models that are financially viable for all parties involved, preventing financial distress for providers or excessive costs for payers.
- Effectiveness: Maximizing the potential of RSAs to drive improvements in patient outcomes and cost efficiency.
- Trust: Building confidence among stakeholders through transparent, data-driven methodologies.
Understanding historical data in healthcare
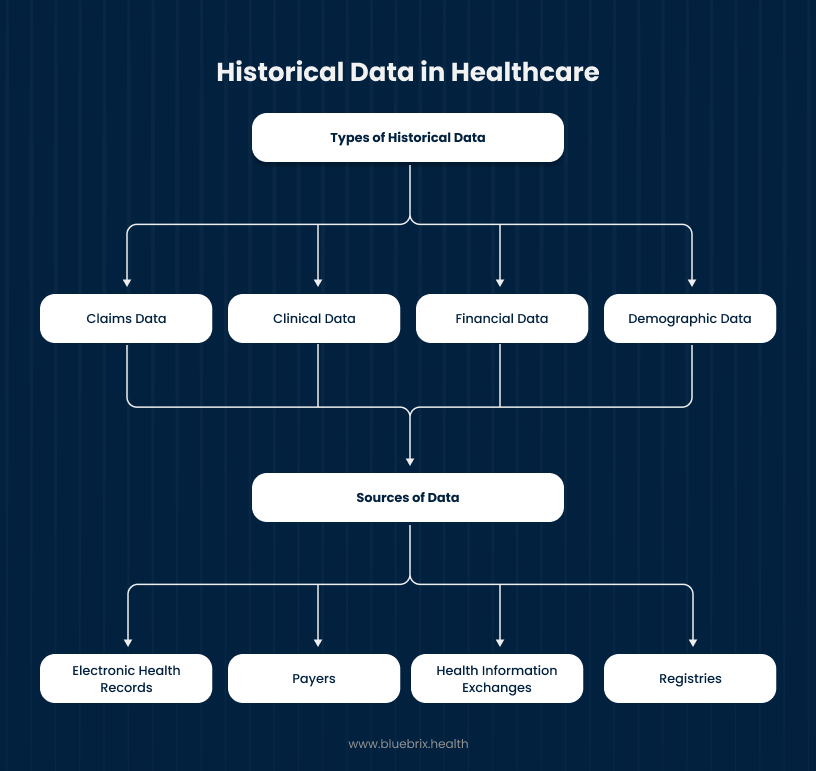
Claims data, clinical data, financial data, demographic data, population health data etc are all types of historical data that are relevant and useful sources of information when it comes to healthcare. These could be sourced from EHRs, payers, Health Information Exchanges (HIEs), registries,etc. Though, the latter two are rarely, if ever, called upon. In healthcare, for best results, data needs to be reliable; i.e. it needs to be complete, factual, and consistent.
Because without quality data, even the best models of care cannot function correctly, and it will lead to poor and unwanted outcomes. Factual historical data leads to proper analysis, which leads to useful conclusions, which can be leveraged to forecast positive outcomes.
An example of this would be having the population health data for a region where the likelihood of obesity is high. By analyzing the data and determining what factors contribute to this (whether it is diet, environmental factors, genetic predisposition, etc.), providers would be able to provide more personalized and well-informed treatment to their patients, to prevent them from becoming obese.
Types of historical data
- Claims data: This is a rich source of information, detailing every service billed by providers to payers. It includes diagnosis codes (ICD-10), procedure codes (CPT), drug codes (NDC), dates of service, and billed amounts. Claims data offers a comprehensive view of utilization and costs.
- Clinical data: Derived from Electronic Health Records, this data includes patient demographics, medical history, diagnoses, lab results, medications, progress notes, and vital signs. It provides granular insights into patient health status and treatment pathways.
- Financial data: Beyond claims, this includes actual payments made, operational costs of healthcare facilities, revenue cycles, and financial performance metrics. It’s crucial for understanding the true economic impact of care.
- Demographic data: Information about patient age, gender, race, ethnicity, socioeconomic status, and geographic location. This data is vital for risk stratification and understanding population health trends.
Sources of data
Historical data is collected from various sources:
- Electronic health records (EHRs): The primary repository of clinical patient data, capturing a longitudinal view of an individual’s health journey.
- Payers: Insurance companies and government health programs maintain vast databases of claims data, offering insights into utilization and costs across large populations.
- Health information exchanges (HIEs): Platforms that enable the secure sharing of patient health information among different healthcare providers and organizations, fostering a more complete patient record.
- Registries: Specialized databases that collect specific health data for diseases, conditions, or procedures (e.g., cancer registries, joint replacement registries). These offer deep insights into specific patient populations and treatment outcomes.
Data quality and integrity considerations
The utility of historical data hinges on its quality. Poor data quality can lead to flawed analyses and detrimental decisions. Key considerations include:
- Accuracy: Is the data free from errors?
- Completeness: Are there missing values or gaps in the data?
- Consistency: Is the data formatted uniformly across different sources?
- Timeliness: Is the data up to date enough for the intended analysis?
- Relevance: Does the data actually address the questions being asked?
- Validity: Does the data measure what it is intended to measure?
Robust data governance and validation protocols are essential to ensure the integrity of historical data.
The link between historical data and risk
Historical data provides the necessary context and evidence to understand and manage risk effectively within healthcare.
Predictive value of past performance
The past is often a strong indicator of the future. By analyzing historical trends in patient populations, provider performance, and cost utilization, healthcare organizations can develop predictive models that forecast future risks and opportunities. For example, patients with a history of multiple chronic conditions are highly likely to be high-cost patients in the future.
Identifying patterns of cost and utilization
Historical claims and financial data reveal patterns in healthcare spending and service utilization. This allows stakeholders to identify:
- High-cost procedures or conditions: Understanding where the majority of healthcare dollars are spent.
- Frequent utilizers: Identifying patients who repeatedly access emergency services or have high inpatient stays.
- Variations in care: Pinpointing differences in treatment patterns or costs across providers or regions.
Assessing provider performance and patient outcomes
Historical data allows for objective assessment of provider performance. By analyzing clinical outcomes, readmission rates, infection rates, and adherence to best practices over time, payers and providers can:
- Benchmark performance: Compare an individual provider or group against peers.
- Identify areas for improvement: Pinpoint specific clinical or operational areas where performance falls short.
- Track progress over time: Monitor the impact of interventions or quality improvement initiatives.
- Evaluate patient outcomes: Understand the effectiveness of different treatment approaches for various patient cohorts.
Key benefits of leveraging historical data
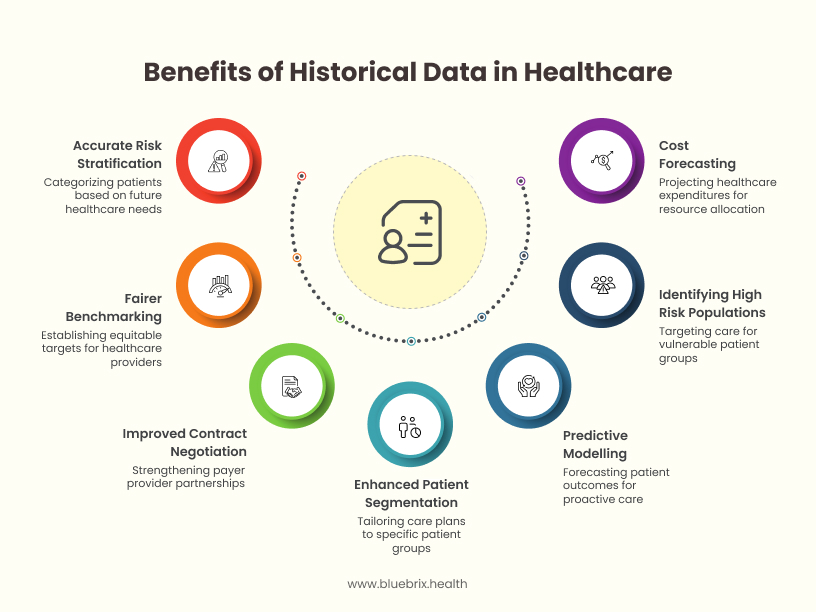
There are many benefits to leveraging historical data, concerning of what has already been mentioned. One of the main ones is more accurate risk stratification, which would help better identify which patients are most at risk and classify them, accordingly, thereby enhancing patient segmentation, so that they can get the proper care plan and resource allocation they need.
More Accurate Risk Stratification
Risk stratification involves categorizing patients based on their likelihood of future healthcare utilization and costs. Historical data, especially claims and clinical information, allows for highly accurate risk stratification by considering factors like:
- Chronic disease burden
- Past utilization patterns (e.g., emergency room visits, hospitalizations)
- Medication adherence
- Socioeconomic determinants of health
This precision ensures that RSAs are tailored to the actual risk profile of patient populations, leading to fairer benchmarks and reimbursement.
Fairer Benchmarking and Reimbursement Models
Without historical data, benchmarks for RSAs can be arbitrary or based on limited information, potentially leading to unfair targets for providers. Historical data enables:
- Data-driven baseline setting: Establishing realistic cost and outcome targets based on past performance of similar patient populations or providers.
- Adjustment for case mix: Accounting for the varying severity and complexity of patients treated by different providers, ensuring “apples-to-apples” comparisons.
- Equitable risk allocation: Ensuring that providers who manage sicker or more complex patient populations are not unfairly penalized.
Improved Contract Negotiation Between Payers and Providers
Historical data empowers both payers and providers with stronger negotiating positions:
- For Payers: Data on past costs and outcomes allows them to propose realistic financial targets and demonstrate the potential for shared savings.
- For Providers: Access to their own historical performance data enables them to showcase their efficiency, quality, and ability to manage costs, justifying favorable terms in risk-sharing contracts. This fosters trust and transparency, leading to more collaborative partnerships.
Enhanced Patient Segmentation and Care Planning
Historical data facilitates the segmentation of patient populations into distinct groups based on similar health characteristics, risk profiles, or care needs. This allows for:
- Targeted interventions: Designing specific care management programs for high-risk cohorts.
- Personalized care plans: Tailoring treatment strategies to individual patient needs, leading to better outcomes.
- Proactive care: Identifying patients at risk of adverse events or high costs before they occur.
Predictive Modelling for Patient Outcomes
By analyzing past patient journeys, historical data can be used to build predictive models that forecast future patient outcomes, such as:
- Likelihood of readmission: Identifying patients at high risk of returning to the hospital within a certain timeframe.
- Disease progression: Predicting the trajectory of chronic conditions.
- Response to treatment: Estimating how different patients might respond to specific therapies.
This allows for proactive interventions and more effective resource allocation.
Identifying High-Risk Populations
Through sophisticated analysis of historical claims, clinical, and demographic data, organizations can pinpoint specific patient groups that are likely to incur high costs or experience adverse health events. These could include:
- Patients with multiple comorbidities
- Frail elderly individuals
- Patients with poor medication adherence
- Individuals facing significant social determinants of health barriers
Identifying these populations allows for targeted care management and preventive strategies.
Cost Forecasting and Budget Impact Analysis
Historical. financial, and claims data are invaluable for:
- Forecasting future healthcare expenditures: Projecting costs for specific patient populations or disease states.
- Budget impact analysis: Assessing the financial implications of new programs, treatments, or policy changes.
- Resource allocation: Optimizing the distribution of resources based on anticipated needs.
Data analytics tools and techniques
Leveraging historical data effectively requires sophisticated analytical tools and techniques.
Predictive modelling and machine learning
These advanced techniques enable the identification of complex patterns and relationships within large datasets. Algorithms can be trained on historical data to:
- Forecast future events: (e.g., readmissions, disease progression, cost trends).
- Identify risk factors: Pinpoint variables that strongly influence outcomes.
- Personalize interventions: Suggest the most effective care pathways for individual patients.
Common techniques include regression analysis, decision trees, random forests, and neural networks.
Risk adjustment algorithms
These algorithms normalize data to account for differences in patient populations’ health status and complexity. They ensure that comparisons between providers or patient groups are fair, regardless of the inherent health risks of their patient panels. For example, a provider treating a sicker population would have their costs or outcomes “risk-adjusted” to be comparable to a provider treating a healthier population.
Cohort analysis and attribution models
- Cohort analysis: Involves studying specific groups of patients (cohorts) with shared characteristics over time. This helps in understanding the long-term impact of interventions, disease progression, or specific treatments.
- Attribution models: Determine which providers are responsible for the care of a specific patient or patient population within a risk-sharing arrangement. This is crucial for correctly assigning accountability for costs and outcomes.
Challenges in utilizing historical data
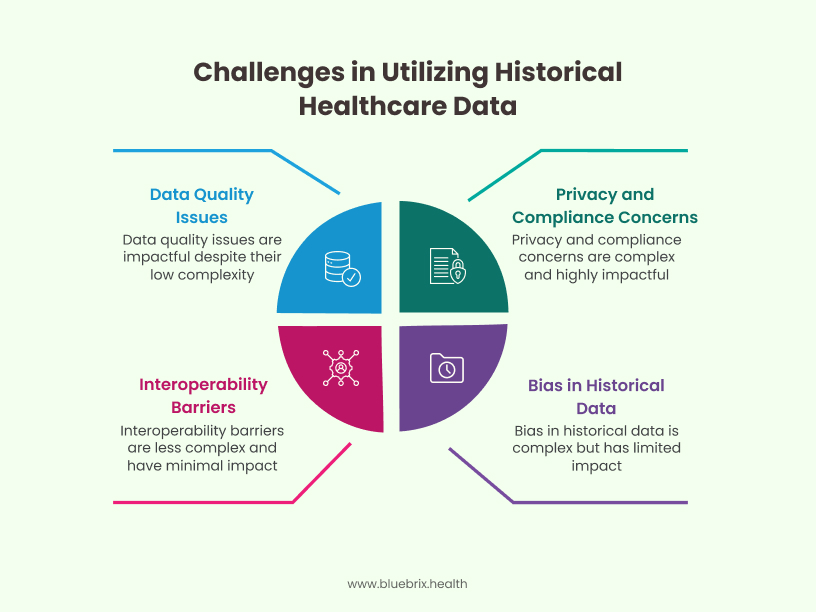
As briefly mentioned in the introduction, while historical data is undoubtedly a valuable and beneficial tool for improving how healthcare is provided, there are challenges. Data is only worthwhile if it is complete and of high quality. For example, knowing that a higher-than-average number of people faced an illness in a specific area is data. But unless we have other relevant factors, such as what the environmental factors were, or what shared identifying factors these people had, the data cannot be utilized effectively.
Data quality and completeness issues
As mentioned earlier, dirty, incomplete, or inaccurate data can severely compromise the reliability of analyses. Missing values, inconsistent formatting, and data entry errors are common problems that can lead to skewed results and faulty conclusions.
Interoperability and integration barriers
Healthcare data often resides in siloed systems (e.g., different EHRs across providers, separate claims systems for payers). The lack of seamless interoperability makes it challenging to integrate data from diverse sources into a unified, comprehensive view of a patient’s health journey or a population’s healthcare utilization.
Privacy and compliance concerns
Healthcare data is highly sensitive. Strict regulatory frameworks like HIPAA (Health Insurance Portability and Accountability Act) govern the collection, storage, and use of protected health information (PHI). Ensuring compliance requires robust data security measures, de-identification protocols, and careful adherence to consent requirements, which can be complex to manage.
Bias and incompleteness in historical data
Historical data can reflect existing biases in healthcare delivery, leading to skewed insights. For example, if certain demographic groups have historically faced barriers to accessing care, their data might be incomplete, leading to an underestimation of their true healthcare needs. Furthermore, data may not capture all relevant social determinants of health or lifestyle factors that significantly impact health outcomes.
Strategies for effective use of historical data
However, these challenges can be mitigated by employing a few different strategies. For instance, building a unified data infrastructure, which would integrate data from a multitude of sources into a single platform. Building partnerships and collaborating with technology providers and data scientists who have expertise in data evaluation and analysis. Establishing data governance and validation protocols for maintaining the integrity and quality of data is also beneficial.
Building a unified data infrastructure
Establishing a centralized, integrated data warehouse or data lake that can ingest, standardize, and store data from various sources (EHRs, claims, wearables, etc.) is fundamental. This “single source of truth” facilitates comprehensive analysis and breaks down data silos.
Collaborating with technology partners and data scientists
Healthcare organizations may lack in-house expertise in advanced data analytics, predictive modeling, and machine learning. Partnering with specialized technology firms and hiring experienced data scientists can bridge this gap, bringing in the necessary technical skills to extract meaningful insights from complex datasets.
Establishing data governance and validation protocols
Robust data governance frameworks are essential. This includes:
- Defining data ownership and accountability.
- Implementing strict data quality checks and validation processes.
- Developing standardized data dictionaries and taxonomies.
- Regularly auditing data for accuracy and completeness.
These protocols ensure that the data used for decision-making is reliable and trustworthy.
Policy and regulatory considerations
Compliance is a must in healthcare. Failure to do so has disastrous consequences across the board for all stakeholders. So, it is crucial to stay up to date and in line with HIPAA, GDPR, and any other framework that is applicable. Government support and even incentives might be receivable based upon meeting relevant criteria.
It is important to keep in mind that the data is meant to be used for humanitarian purposes and misuse would be considered unethical and would have repercussions.
Ethical implications of data use
The use of historical data, particularly for predictive modeling and patient segmentation, raises significant ethical considerations:
- Bias and discrimination: Ensuring that algorithms built on historical data do not perpetuate or amplify existing healthcare disparities.
- Patient autonomy and consent: Balancing the benefits of data analysis with individual privacy rights and obtaining appropriate consent.
- Transparency: Being clear about how data is being used and the implications for patient care.
- Accountability: Establishing clear lines of responsibility for outcomes derived from data-driven decisions.
Future outlook
The future looks promising when it comes to using historical data to optimize RSAs. AI is already proving to be a valuable asset, capable of offering real-time insights and personalized recommendations. Its influence and assistance can only improve as technology evolves.
The role of AI in evolving risk-sharing models
Artificial intelligence, particularly machine learning, will continue to play a pivotal role. AI can:
- Automate data analysis: Rapidly process vast amounts of historical data.
- Identify subtle patterns: Uncover insights that human analysts might miss.
- Optimize contract terms: Suggest optimal risk-sharing parameters based on predictive analytics.
- Facilitate real-time adjustments: Enable dynamic adjustments to RSAs based on unfolding events.
Personalized contracts based on real-time + historical data
The future will likely see RSAs becoming even more granular and personalized. By integrating real-time data streams (e.g., from remote monitoring devices, wearable tech) with comprehensive historical data, contracts could be dynamically adjusted to individual patient needs and evolving health status. This would allow for highly precise risk assessment and targeted interventions.
Data-driven policy innovations and standardization
As the efficacy of data-driven RSAs becomes more evident, we can expect to see policy innovations that encourage and standardize their adoption. This could involve:
- Common data standards and interoperability frameworks: Facilitating seamless data exchange across the ecosystem.
- Incentives for data sharing and collaboration: Encouraging organizations to contribute to broader data pools for collective benefit.
- Regulatory sandboxes: Allowing for the testing of new data-driven models in a controlled environment.