The HCC risk adjustment model has been a cornerstone of Medicare payments since CMS introduced it back in 2004. What started as a way to standardize payment adjustments based on patient health status and complexity quickly became essential for ensuring fair reimbursement that actually reflects the risk of patients’ chronic and acute conditions. But HCC Version 24, which was originally developed based on ICD-9-CM and adapted to map ICD-10-CM codes, began to show limitations as clinical practices and healthcare delivery evolved.
This limitation gave birth to HCC version 28. CMS developed V28 to enhance clinical specificity by fully leveraging the detailed ICD-10-CM coding system, expanding condition categories from 86 to 115. The rollout is happening in three phases from 2024 to 2026, gradually replacing V24. For billing teams, this means adapting coding practices, documentation workflows, and preparation strategies to meet new standards and optimize risk scores throughout this transition.
Let’s first have a sneak peek into HCC V24 limitations!
Why HCC V24 needed an update: challenges in today's healthcare landscape
HCC V24 didn’t go well with the evolving healthcare landscape, such as it struggled with outdated ICD-9-based coding, inconsistent risk scoring, and allowed upcoding that risked audits and payment clawbacks. These issues made accurate billing and revenue forecasting difficult, calling for a more precise and clinically relevant update—now addressed by HCC V28.
Upcoding and overpayment
Under HCC V24, even minor, well-controlled, or history-only conditions could increase a patient’s risk score, paying providers higher than justified. This “upcoding” was baked into the system, exposing billing teams to the risk of audits, payment clawbacks, or fraud investigations. The lack of checks meant that even unintentional errors could trigger costly penalties and draw negative payer attention—raising the stakes for every claim submitted.
Outdated condition mapping
V24’s structure was designed for the old ICD-9 coding system, but everyone now codes in ICD-10. This mismatch meant billing teams often had to bend or stretch today’s codes to fit yesterday’s categories, resulting in confusion, misapplied codes, and frequent delays in payment. As a result, hard work tracking new or clinically important diagnoses could be wasted if those conditions didn’t translate into higher RAF scores or were simply left out of the model altogether.
Oversized and non-specific code lists
With nearly 10,000 diagnosis codes mapping to HCCs—many of which were broad or vague—it was difficult for billing teams to distinguish which codes truly impacted reimbursement. This “everything counts” approach created complexity, increased the likelihood of coding errors, and made it hard to develop clear internal protocols. The noise from non-specific codes often drowned out opportunities for focused, accurate documentation, secretly eroding compliant revenue.
Inconsistent RAF scoring
One of the biggest challenges of V24 was its unpredictable approach to scoring. Some chronic conditions with complications could sharply increase payments, while other serious diagnoses were undervalued or inconsistently weighted. For billing teams, this made forecasting revenue unreliable and muddied communication with clinical staff about which diagnoses merited meticulous attention. Ultimately, this inconsistency threatened both financial planning and operational trust.
HCC V28 steps in: how CMS is rewriting the risk adjustment playbook
HCC V28 brings significant changes to risk adjustment by removing ICD-10 codes that are not significant for predictive purposes and adding more relevant ones, fully adopting the detailed ICD-10-CM system, expanding condition categories from 86 to 115, and much more. Let’s take a closer look at each one.
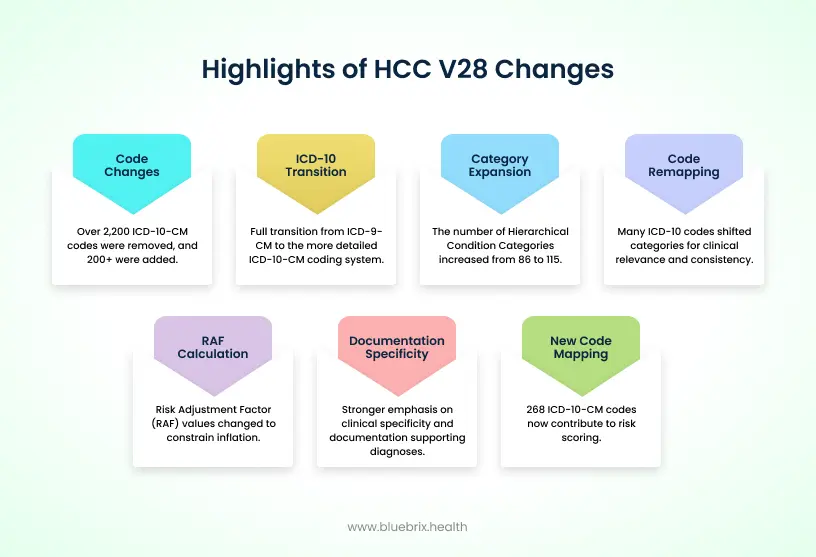
2,200+ ICD-10-CM codes removed, 200+ added
HCC V28 notably reduces the overall number of diagnosis codes that count toward risk adjustment, removing over 2,200 ICD-10 codes that were considered less predictive of future healthcare costs. Many of these were for mild, stable, or resolved conditions like stable angina (e.g., I20.8, I20.9) or substance use disorders in remission (e.g., F10.21, F19.21), which weighed scores under V24 but did not reflect ongoing clinical complexity.
Meanwhile, V28 adds about 200 new codes, including more specific conditions that better identify severe or chronic illness, such as certain congenital anomalies (e.g., Q21.1 Atrial septal defect) and severe persistent asthma (e.g., J45.50 Severe persistent asthma, uncomplicated). This streamlining improves accuracy by focusing payment on truly active and costly conditions.
Moving from ICD-9-CM to the ICD-10-CM structure
HCC Version 24 was originally developed using the ICD-9-CM coding system, which was limited in detail and less suited for today’s complex healthcare environment. V28 fully transitions to ICD-10-CM, a much richer and more detailed coding system. This shift allows HCC categories to better represent the wide variety of medical conditions seen today, including subtle differences in disease type, severity, and location. The ICD-10 system’s enhanced structure supports more precise risk adjustment, enabling payments that more accurately reflect patient complexity.
Expanding payment condition categories (86 to 115)
The number of Hierarchical Condition Categories increases from 86 in V24 to 115 in V28, allowing more detailed grouping of diagnoses. For example, diabetes previously split into broad categories like “with complication” or “without complication” is now divided into finer groups capturing nuances such as “glycemic control unspecified” and specific types of complications.
Similarly, psychiatric conditions like psychosis have been expanded to differentiate between schizophrenia, other psychotic disorders, and severity levels. This granularity supports precision in risk scoring and aligns coding closer to the actual resource needs patients have.
Remapping of ICD-10 codes between HCC categories
Many ICD-10 codes shifted categories to improve clinical relevance and scoring consistency. For example, diabetes codes were classified into three categories – uncomplicated, with acute complication and chronic complication might now be grouped together with same coefficient (risk score) to avoid overinflation of scores. Conditions such as peripheral artery disease and toe amputation related to diabetes may be rolled into one diabetes HCC category instead of separate ones. This remapping reduces redundancies and makes the risk score more reflective of true patient burden.
RAF score calculation changes
The risk adjustment factor (RAF) values assigned to some conditions have changed to constrain inflation and better reflect cost patterns—for example, some diabetes categories now share the same score regardless of complication type. The V28 model’s recalculations generally lead to lower combined RAF scores per patient, reflecting a trimmed down and more clinically accurate risk profile. Billing teams can expect to see case-mix scores that better mirror severity rather than “counting” all associated diagnoses separately.
Increased specificity in documentation
V28 places stronger emphasis on the clinical specificity and documentation supporting diagnoses. Coders and billers must capture the exact type, severity, and status of a condition. For example, simply documenting “vascular disease” is no longer sufficient; terms like “vascular disease with ulcer” or “vascular disease with gangrene” are needed to justify higher risk scores.
Similarly, mild or inactive conditions—like mental health disorders in remission—no longer impact scores unless clear clinical activity or treatment is documented. This demands closer collaboration between billing, coding, and clinical teams to ensure documentation supports precise coding and accurate reimbursement under V28.
New codes mapping to HCC in V28
In V28, 268 ICD-10-CM diagnosis codes that did not map to any HCC category in V24 now contribute to risk scoring. This is partly due to the system’s evolution to fully leverage the ICD-10 structure. Many of these new codes come from Chapter 16 (“Certain conditions originating in the perinatal period”) and Chapter 17 (“Congenital malformations, deformations, and chromosomal abnormalities”).
Although these conditions are uncommon in Medicare populations, they can significantly impact risk adjustment for commercial insurance groups where such diagnoses are more frequent. This update broadens the model’s clinical scope and enables more accurate risk stratification in non-Medicare settings.
Preparing billing team for the V28 shift: what you need to do now
Here are some essential steps billing teams must take now to prepare for the HCC V28 transition—from understanding discontinued codes and raising documentation standards to mastering the blended RAF model, auditing claims, staying updated with CMS changes, and leveraging advanced technology for a smooth, compliant shift.
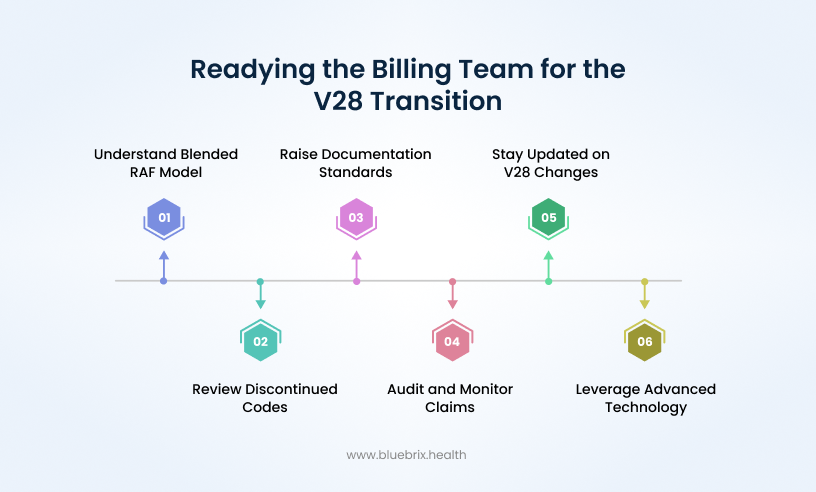
Right picture of blended RAF model
From 2024 to 2026, CMS will calculate risk scores using a blend of V24 and V28 models that gradually shift weight towards V28.
2024 – 67% V24 + 33% V28
2025 – 33% V24 + 67% V28
2026 – 100% V28
An example for 2025 RAF for a MA patient:
Patient RAF score is 1.2 (V24)
Patient RAF score is 1.0 (V28)
Blended score of the patient: 1.2*0.33 + 1.0*0.67 = 1.09
To effectively manage the blended RAF model transition from V24 to V28, monitor key metrics such as monthly RAF score trends to track overall risk score changes, compare individual patient RAF scores under both models to identify impactful diagnosis shifts, measure the capture rate of active diagnoses emphasized by V28, analyze reimbursement variations across risk tiers to understand financial impact, and track documentation quality along with denial trends related to updated coding requirements to pinpoint areas for improvement and proactive revenue management.
Review and understand discontinued codes
The diagnosis codes we discussed earlier that no longer map to HCC categories in V28 are a key area billing teams need to focus on. Because thousands of these codes—like those for stable angina or mental health remission states—were removed, it’s important billing staff know exactly which codes no longer impact risk scores. This understanding keeps everyone from wasting time chasing documentation or coding conditions that won’t affect payments anymore. Instead, billing can concentrate on active and high-impact diagnoses that truly drive reimbursement and compliance.
Raise documentation standards (MEAT)
Version 28 puts a heavier spotlight on MEAT criteria—Monitor, Evaluate, Assess, and Treat—to confirm that diagnoses are truly active and clinically significant. Billing teams should work closely with clinicians to ensure documentation clearly captures these elements, not just checkbox mention but real evidence in patient records. Vague or “history of” diagnoses won’t fly anymore if the condition isn’t driving active treatment or monitoring.
Here is the practical MEAT checklist for the billing team:
Monitor: Document signs, symptoms, disease progression or regression, and mention any surveillance activities (e.g., “Checking HgbA1c,” “disease stable on medication”).
Evaluate: Reference and discuss test results, medication effectiveness, and response to treatment (e.g., “reviewed blood pressure trends,” “medications effective”).
Assess/Address: Provide your clinical impression of the status of the condition, discuss findings, review records, or offer counseling relevant to the diagnosis.
Treat: Describe any specific treatment, including medication changes, referrals, therapies, or patient education related to the condition (e.g., “continue with current therapy,” “referred to endocrinologist”).
Good documentation isn’t just compliance—it’s a tool to improve risk adjustment accuracy and patient care quality. For instance, capturing test results, medication adjustments, evaluation notes, and treatment plans in real time helps meet MEAT and supports codes under V28’s stricter rules. Reports show organizations that emphasize thorough MEAT documentation see better RAF scores and fewer denials because the clinical picture aligns with coding.
Audit and monitor claims
Increased audit activity around V28 is expected as payers refine adjudication under the new model. You should prioritize routine claim audits to catch under- or over-coding, incomplete documentation, or codes that no longer map. Monitoring denial and payment trends early can pinpoint where additional training or process changes are needed. Proactive auditing helps avoid costly recoupments and smooth revenue cycles.
Stay updated on HCC V28 changes
CMS updates or clarifications on V28 coding and documentation will continue to roll out in the years ahead, especially during the phased transition through 2026. You must stay engaged with these updates—through webinars, newsletters, and internal trainings—to align workflows and maintain compliance. This isn’t a one-time learning event; it’s a continuous adaptation.
Leverage advanced technology
Navigating V28’s complexity requires more than manual effort—advanced coding and risk adjustment analytics tools are essential. These tools automatically flag missing MEAT elements and incomplete documentation, help verify encounter form compliance, and highlight coding gaps early. Integrated AI can scan clinical notes for overlooked diagnoses and align coding with evolving V28 standards, improving accuracy without extra clinician burden.
Real-time dashboards provide actionable insights into RAF trends and audit risks, enabling billing teams to proactively optimize documentation and maximize reimbursement while reducing denials and compliance risks.