The behavioral healthcare landscape is more than just dynamic; it’s a rapidly shifting current, often feeling like a torrent for those dedicated to navigating its depths. For the providers who pour their hearts into healing and the administrators who tirelessly champion efficiency and quality, the weight of administrative burdens, especially billing, can feel overwhelming. It’s a silent stressor, pulling focus away from the profound impact you strive to make every single day.
In 2025, the idea of simply “getting by” with your current systems is no longer viable. It’s about protecting the very core of your mission. When billing falters, it’s not just about lost revenue; it’s about the emotional toll of delayed care, the exhaustion of fighting administrative battles instead of focusing on patient well-being, and the heartbreaking reality of potentially compromising the compassionate care you’re so committed to delivering.
At blueBriX, we truly see you. We understand the sacrifices you make, the late nights, and the profound responsibility you carry. We know your focus needs to be on the human connection, on guiding individuals towards hope and healing. That’s why we’re not just offering technology; we’re offering a lifeline. We’re here to empower your practice with a billing system that liberates you from the administrative quicksand, allowing you to breathe, to thrive, and to pour your invaluable energy back into the lives you touch.
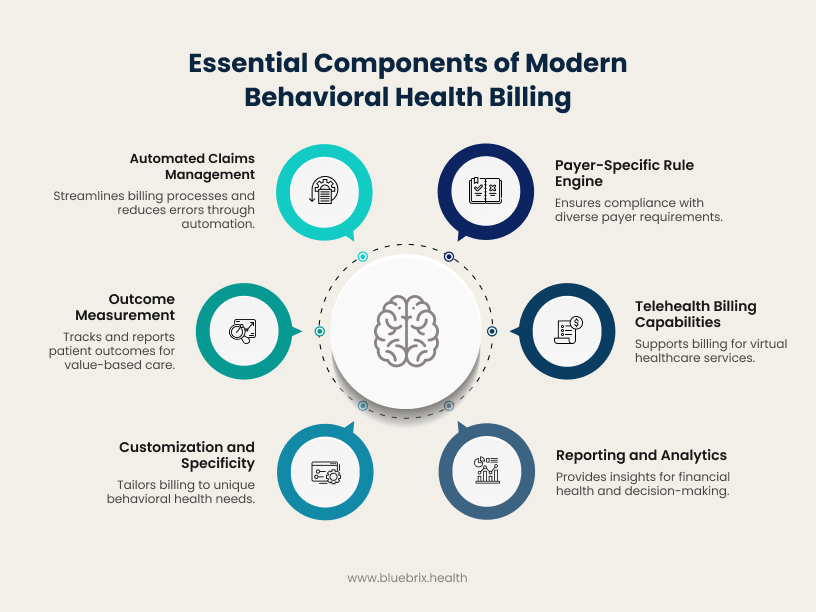
Join us as we explore the six essential features that will transform your billing from a source of anxiety into a steadfast partner, ensuring your practice remains financially robust and emotionally sound, ready to meet the future with unwavering dedication.
Feature 1: automated claims management and real-time tracking
The complexities of behavioral health billing—from varying CPT codes for psychotherapy to specific modifiers for telehealth—often lead to claim rejections, delayed payments, and administrative backlogs. Manual claim submission and a lack of visibility into their status can impact cash flow and divert valuable resources to chasing down denials rather than focusing on patient well-being.
In 2025, a leading behavioral health billing system must offer automated claims management coupled with real-time tracking capabilities. Such intelligent and proactive management will identify issues before they become problems, ensuring a smooth and predictable revenue cycle.
- Proactive error detection: Automated pre-submission scrubbers catch common billing errors and compliance issues specific to behavioral health (e.g., incorrect NPIs, missing authorizations for specific services) before claims are sent.
- Accelerated reimbursements: With automated submission processes and fewer rejections, claims are processed faster, leading to quicker reimbursements.
- Transparent financial oversight: Real-time dashboards provide an instant, clear view of every claim status—from submission to payment. Practices can track claims by payer, identify bottlenecks, and quickly address any issues.
- Reduced manual intervention: Automating the submission process frees staff from tedious, repetitive tasks, allowing them to focus on more impactful work like patient care and complex case management.
Our solutions provide an intelligent automation layer for your claims, ensuring that each submission is optimized for acceptance and offering you continuous, real-time insights into your financial health.
Feature 2: payer-specific rule engine and automated claim scrubbing
Behavioral health billing is notoriously complex due to the huge volume and diversity of payer rules. Each insurance carrier – be it Medicaid, Medicare, or commercial plans – has its own unique requirements for coding, modifiers, documentation, and submission formats. Staying on top of these ever-changing rules manually is a tedious task, otherwise leading to claim rejections, denials, and significant delays in reimbursement.
In 2025, your billing system must feature a robust payer-specific rule engine combined with automated claim scrubbing. This intelligent functionality acts as your first line of defense, proactively identifying potential issues before a claim ever leaves your office.
- Real-time error detection: Instantly flags missing or invalid patient details, unsupported diagnoses, and payer-specific coding issues—common pitfalls in behavioral health billing.
- Continuously updated payer logic: Ensures compliance with state-specific Medicaid rules, modifier requirements for therapy services, and evolving documentation mandates.
- Pre-submission validation: Reduces the burden of denials by catching issues early, which is critical when dealing with complex services like IOP, PHP, or group therapy.
- Maximized revenue: Fewer denials and faster processing cycles translate to improved cash flow and sustainable revenue for behavioral health organizations.
blueBriX understands the dynamic nature of payer rules. Our system incorporates an advanced rule engine that is continually updated, offering comprehensive claim scrubbing capabilities to minimize denials and optimize your revenue cycle, ensuring you get paid accurately and on time.
Feature 3: telehealth billing capabilities
The post-pandemic era has solidified telehealth as an indispensable component of behavioral healthcare delivery. Virtual appointments offer accessibility and convenience, making them a permanent fixture in modern practice. However, billing for telehealth services introduces its own set of complexities.
Specific CPT codes, modifiers (such as -95 or GT), and nuanced geographical requirements often apply to telehealth services. Incorrect application of these can lead to denials or audits.
- Supports core behavioral health modalities: Bill seamlessly for individual therapy, group therapy, psychiatry sessions, and phone consults—regardless of platform.
- Smart modifier automation: Automatically applies the correct modifiers based on session type, provider location, and payer requirements, ensuring compliance and speed.
- State-specific rule management: Navigates Medicaid and commercial payer telehealth regulations across state lines, ideal for multi-state or hybrid practices.
- Telehealth platform integration: Syncs session data, logs, and attendance directly into billing workflows—saving time and ensuring documentation integrity.
Recognizing the permanence of telehealth, blueBriX has prioritized robust telehealth billing functionalities within our EHR. Our system simplifies the complexities, ensuring that your virtual services are billed accurately, compliantly, and efficiently, allowing you to focus on delivering care.
Feature 4: reporting and analytics for financial health
In 2025, static reports that merely list figures are no longer sufficient. To truly understand and improve your practice’s financial health, you need dynamic, insightful analytics that allow for data-driven decision-making.
- Claim denial rates and trends: Spot denials stemming from time-based coding, lack of prior auth, or inconsistent documentation common in therapy and psychiatry billing.
- Revenue cycle management (RCM) performance: Track the efficiency of your entire billing process, from claim submission to payment.
- Accounts receivable (A/R) aging: Track aging balances tied to recurring sessions, Medicaid reimbursements, or split billing (e.g., for co-occurring disorders).
- Payer mix analysis: Assess the impact of Medicaid, Medicare, and commercial plans on your behavioral health collections—especially across states with varying telehealth coverage.
- Identification of revenue leakage: Pinpoint where money is being lost due to inefficiencies, uncollected balances, or consistent denials.
- Enhanced operational efficiency: Identify bottlenecks in your billing process and optimize workflows for maximum output.
blueBriX provides intuitive and powerful reporting and analytics tools that transforms raw data into actionable insights. Our dashboards and customizable reports give you a real-time pulse on your practice’s financial health, empowering you to make smarter, more profitable decisions.
Feature 5: deep behavioral health specificity & customization
Generic billing systems often fall short when confronted with the nuanced demands of behavioral health. From the unique diagnostic codes for mental health and substance use disorders (e.g., F-codes) to the specific requirements for different modalities like group therapy, family counseling, or telehealth, a one-size-fits-all approach inevitably leads to miscoded claims, compliance gaps, and missed revenue opportunities. In 2025, a premier behavioral health billing system must offer deep, inherent specificity and extensive customization capabilities.
- Tailored coding and modifiers: Support for specific CPT codes (e.g., 908xx series), DSM-5 diagnoses, and relevant modifiers (e.g., GT for telehealth, GN/GO/GP for specific practitioners) is built-in, reducing manual errors and ensuring accurate claims that reflect the clinical reality of behavioral health services.
- Flexible workflow configuration: Practices can customize intake forms, treatment plan templates, scheduling rules for recurring sessions, and billing pathways to align with their specific clinical protocols and operational needs, whether they are an outpatient clinic, an inpatient facility, or a community-based organization.
- Scalability for diverse practice models: The system can be configured to support a wide range of behavioral health settings—from solo practitioners to large multi-specialty groups, integrated care models, or substance abuse treatment centers—each with their distinct billing and documentation requirements.
Solutions at blueBriX are engineered with an intrinsic understanding of the behavioral health landscape, providing a highly customizable platform that not only manages your billing with precision but also seamlessly integrates with and enhances your unique clinical and operational workflows, ensuring compliance and maximizing your financial health.
Feature 6: outcome measurement and value-based care support
Behavioral health practices are facing increasing pressure to demonstrate the effectiveness of their services as we are moving towards the value-based care concept. The lack of integrated tools to systematically collect, track, and report on patient outcomes makes it challenging for practices to prove their value. This often leaves practices at a disadvantage in a market increasingly focused on quantifiable results. Therefore, a leading behavioral health billing system must offer capabilities for outcome measurement and integrated support for value-based care models.
- Integrated outcome tracking: Seamlessly embedded validated outcome measures (e.g., PHQ-9, GAD-7, PTSD-5) directly within clinical workflows. This ensures consistent data collection without disrupting patient care, providing a clear picture of progress over time.
- Value-based care reporting & analytics: Generate the specific reports and aggregated data required for participation in alternative payment models (APMs), such as bundled payments, shared savings, or capitated arrangements. This enables practices to meet contractual obligations and unlock new revenue streams.
- Enhanced payer negotiation: Leverage demonstrable outcome data to negotiate more favorable contracts with insurance carriers. By proving the effectiveness and efficiency of your services, your practice can secure higher reimbursement rates and preferred network status.
- Population health insights: Analyze outcome data across your patient population to identify trends, optimize care protocols, and continuously improve the quality and efficacy of the services you provide.
blueBriX integrates comprehensive outcome measurement and value-based care support, empowering your practice to manage your revenue cycle efficiently as well as to prove your clinical impact, thrive in new payment models, and deliver demonstrably better patient care.
Ready to transform your billing process and secure your practice's financial health?
Request a demo to see how our comprehensive EHR billing system can empower your behavioral health practice in 2025 and beyond.
Request a demo