Every day, healthcare organizations across the United States lose thousands of dollars to preventable inefficiencies. Poor care coordination costs the American healthcare system between $27.2 billion and $78.2 billion annually in wasteful spending. For individual organizations, these losses manifest as hospital readmissions, duplicate testing, staff burnout, and missed quality bonuses under value-based care contracts. The question isn’t whether your organization can afford to invest in better care coordination, it’s whether you can afford not to.
Healthcare decision-makers face an urgent reality: fragmented care coordination directly impacts your bottom line and operational performance. With 80% of serious medical errors involving miscommunication during care transitions, and hospital readmissions costing Medicare alone over $17 billion annually, the financial and reputational stakes have never been higher. This comprehensive analysis examines how the following 10 care coordination challenges erode your ROI and operational efficiency and how intelligent care orchestration platforms are helping leading organizations reverse these losses.
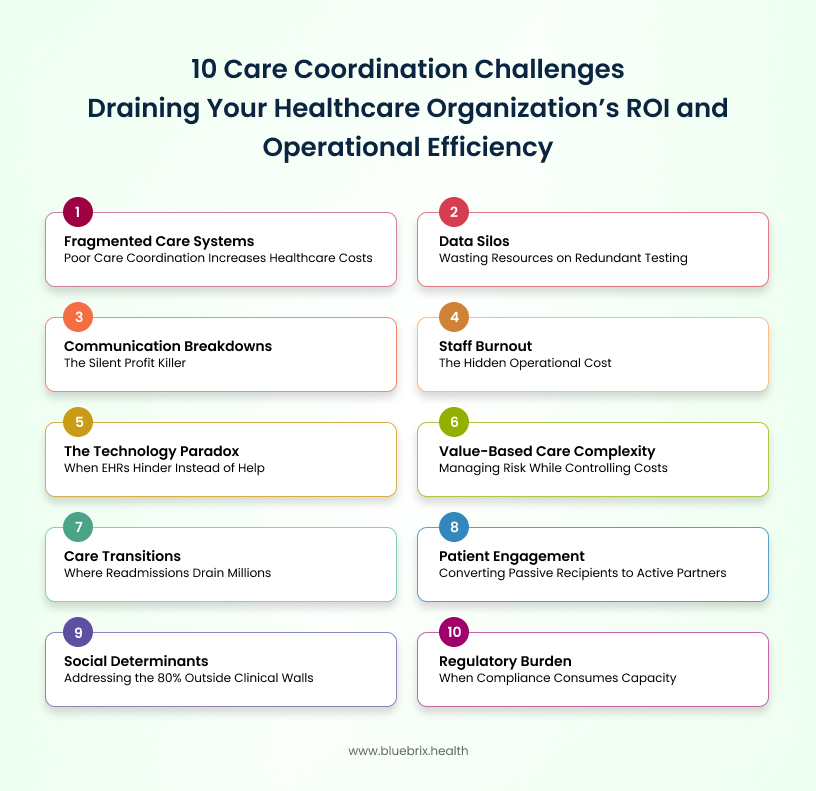
1.The financial impact of fragmented care systems
Research demonstrates that poor care coordination can increase healthcare costs by up to 20% due to redundant tests and unnecessary treatments. For an average-sized hospital managing 50,000 patient encounters annually, this translates to millions in avoidable costs. One study documented duplicate testing charges of $639 per trauma patient transferred between facilities due to lack of information sharing.
When healthcare services operate in isolated silos with disconnected electronic health record systems, the financial consequences cascade throughout your organization. Fragmentation forces patients to navigate disconnected services without clear pathways, resulting in treatment delays, medication errors, and ultimately poorer health outcomes.
Fragmented systems force care coordinators to manually track down patient information across multiple platforms, consuming hours that could be spent on direct patient care. When providers lack access to complete medical histories, they must order repeat tests, schedule redundant appointments, and spend additional time reconciling conflicting information.
Modern care coordination platforms like blueBriX address fragmentation by creating a unified data architecture that aggregates information from EHRs, labs, claims systems, and behavioral health records into a single source of truth. This eliminates the need for manual data hunting and ensures every care team member accesses the same comprehensive, real-time patient view.
2. Communication breakdowns: the silent profit killer
Communication failures between healthcare providers represent one of the most dangerous and expensive coordination challenges. When providers rely on different communication methods ranging from fax machines to disparate digital systems, critical information falls through the cracks. These breakdowns result in treatment delays that extend hospital stays, duplicative testing that wastes resources, and medication errors that trigger costly adverse events requiring additional intervention.
Consider the workflow disruptions: a care coordinator attempting to reach a specialist’s office may spend 15-20 minutes on hold, send multiple faxes that go unanswered, or resort to physically walking paperwork between departments. Multiply these interruptions across dozens of patients and multiple care team members, and you’ve created a system where administrative friction consumes the majority of productive capacity.
Advanced care coordination platforms eliminate these bottlenecks by embedding HIPAA-compliant, real-time communication tools directly into care workflows. Secure messaging, automated task routing, and instant notifications ensure that the right information reaches the right provider at the right time without phone tag, lost faxes, or delayed responses that compromise patient safety and organizational efficiency.
3. Data silos: wasting resources on redundant testing
Isolated pools of patient information that cannot be shared between providers create one of the most quantifiable drains on healthcare resources. When different organizations use incompatible data formats and standards, exchanging information becomes extremely difficult or impossible.
Data silos force clinical staff to manually re-enter information across systems, consuming valuable time while introducing transcription errors. Providers spend additional time tracking down test results from external facilities, often reordering tests rather than delaying treatment, a decision that prioritizes immediate patient needs but compounds long-term cost and efficiency problems.
The numbers tell a compelling story. Research found that 32% of examined cases involved duplicate testing, with 20% of cases having at least one duplicate test that was not clinically indicated. Higher care coordination scores were inversely associated with Medicare expenditures, with organizations seeing reductions ranging from $83 to $106 per patient per month for each one-point increase in coordination scores. For organizations managing populations of 10,000 or more patients, these monthly savings compound into millions annually.
Interoperability-first platforms built on FHIR, HL7, and open API standards eliminate data silos by enabling seamless, bidirectional information exchange across any healthcare system. When patient data flows automatically and securely between EHRs, labs, specialists, and community providers, organizations eliminate redundant testing while accelerating clinical decision-making.
4. The technology paradox: when EHRs hinder instead of help
An average-sized hospital spends nearly $760,000 annually just to meet meaningful use administrative requirements, with an additional $411,000 invested in system upgrades. When EHR systems lack needed functionality or fail to communicate with each other, organizations face the double financial burden of technology costs plus the ongoing expense of manual workarounds. Meanwhile, fewer than 40% of U.S. providers reported sharing health data effectively with other organizations, undermining the coordination benefits that EHRs should provide.
Consider the real-world impact: nurses and physicians spending 30-40% of their time on documentation rather than patient care, care coordinators toggling between five different systems to compile a complete patient record, and clinical staff developing time-consuming workarounds because the EHR doesn’t support their actual workflows.
Modern care coordination platforms like blueBriX solve the technology paradox through intelligent integration rather than replacement. By layering coordination functionality on top of existing EHRs through open APIs, organizations preserve their technology investments while gaining the workflow automation, real-time communication, and comprehensive patient views that drive measurable efficiency gains.
5. Staff burnout: the hidden operational cost
Care coordinators managing caseloads exceeding 300 patients while juggling competing data management and case management demands represent a ticking time bomb for healthcare organizations. The emotional stress of working with vulnerable populations, combined with inadequate technological support, creates burnout rates exceeding 20% among social workers.
Staff turnover costs organizations between 50-200% of an employee’s annual salary when accounting for recruitment, onboarding, training, and lost productivity during vacancy periods. For specialized care coordinators earning $60,000-$80,000 annually, each turnover event costs $30,000-$160,000. Organizations experiencing high coordinator burnout face continuous turnover cycles that perpetually drain resources while undermining care quality and coordination continuity.
Burnout manifests operationally as increased absenteeism, reduced productivity, higher error rates, and disengaged staff who complete minimum requirements rather than delivering exceptional care. Survey data reveals that 78% of wraparound care coordinators identify stress and burnout as significant causes of turnover in their organizations. Organizations trapped in burnout cycles find themselves continuously training new staff rather than building expert teams.
Intelligent care coordination platforms directly address burnout by automating administrative burdens that consume coordinator time without adding patient care value. By handling appointment reminders, referral tracking, documentation templates, and routine follow-ups automatically, platforms free coordinators to focus on complex patient needs requiring human judgment and compassion—the work that drew them to healthcare in the first place.
6. Care transitions: where readmissions drain millions
Poorly executed transitions when patients move between care settings represent some of the most expensive coordination failures. Hospital readmissions numbered 2.3 million (19%) among Medicare enrollees within 30 days of discharge, generating over $17 billion in healthcare costs.
Under Medicare’s Hospital Readmissions Reduction Program, hospitals face financial penalties for excess readmissions—penalties that can reach 3% of Medicare payments. For a hospital receiving $50 million in annual Medicare reimbursements, maximum penalties could total $1.5 million annually. Beyond penalties, each preventable readmission costs organizations the full expense of care without corresponding reimbursement under bundled payment models.
Failed transitions create operational chaos: emergency departments managing avoidable admissions, care teams scrambling to piece together discharge information, and coordinators conducting crisis management rather than proactive care planning. Research shows that among patients referred for post-discharge coordination, those who didn’t receive assigned interventions had 1.27 to 1.83 times higher odds of readmission.
Comprehensive care coordination platforms transform transitions through automated workflows that ensure nothing falls through the cracks. Features including discharge checklist automation, post-discharge monitoring triggers, primary care follow-up scheduling, medication reconciliation tools, and patient education delivery create reliable transition processes that reduce readmissions while requiring minimal manual coordination effort.
7. Value-based care complexity: managing risk while controlling costs
Value-based contracts require organizations to deliver quality outcomes at controlled costs, a balance nearly impossible without coordinated care approaches. Healthcare organizations participating in value-based care arrangements put significant revenue at risk based on quality performance. Medicare Shared Savings Program participants, for example, can earn shared savings bonuses or face shared losses based on their quality and cost performance. Organizations lacking the care coordination infrastructure to close care gaps, manage high-risk patients proactively, and track quality metrics find themselves leaving bonus money on the table or worse, facing financial penalties.
Value-based care requires tracking dozens of quality measures, identifying at-risk patients before they become high-cost cases, coordinating across multiple providers to close care gaps, and documenting all interventions to support quality reporting. Organizations attempting to manage these requirements through manual processes or disconnected systems struggle to scale value-based care programs beyond pilot stages.
Purpose-built care coordination platforms enable value-based care success through risk stratification engines that identify high-need patients, automated care gap identification and closure workflows, customizable care plans aligned with quality measures, and comprehensive reporting that supports quality submissions while tracking shared savings performance. These capabilities transform value-based care from an operational burden into a strategic advantage.
8. Social determinants: addressing the 80% outside clinical walls
Healthcare organizations increasingly recognize that social determinants such as housing stability, food security, transportation access, and social support drive 80% of health outcomes. Yet most struggle to systematically screen for, document, and address these factors due to time constraints, limited community resources, and lack of integrated workflows.
Patients with unaddressed social determinants experience worse health outcomes requiring more expensive interventions. A patient lacking reliable transportation misses appointments, fails to fill prescriptions, and ultimately presents to the emergency department with preventable complications. The emergency visit costs the organization thousands in unreimbursed care under value-based contracts, demonstrating how failing to address a $20 transportation barrier creates a $5,000 problem.
Without systematic approaches, addressing social determinants becomes random and inefficient. Care coordinators spend hours researching community resources, making calls to verify eligibility, and attempting to connect patients with services—often duplicating efforts that colleagues performed weeks earlier for different patients with similar needs.
Advanced care coordination platforms streamline social determinant integration through screening tools embedded in enrollment workflows, community resource directories with real-time availability, closed-loop referral tracking to community organizations, and automated follow-up to ensure patients successfully access services. These capabilities enable organizations to address social determinants efficiently at scale rather than through heroic individual efforts.
9. Patient engagement: converting passive recipients to active partners
Patient non-adherence to treatment plans, missed appointments, and premature therapy discontinuation create significant coordination challenges. These engagement failures stem from multiple barriers including limited health literacy, financial constraints, transportation challenges, and lack of trust in healthcare systems.
Non-adherence costs the U.S. healthcare system an estimated $290 billion annually in avoidable medical spending. For individual organizations, patient non-engagement manifests as no-shows that waste scheduled appointment slots, complications from medication non-adherence requiring expensive acute interventions, and missed quality measure opportunities that reduce value-based care bonuses.
Care coordinators waste significant time attempting to reach disengaged patients through repeated phone calls, rescheduling missed appointments, and managing preventable complications. As one coordinator noted, “One major challenge is getting patients to ‘engage’ in care management. Some of these patients are resistant to talking with a nurse care manager and decline to participate”.
Purpose-built care coordination platforms can enhance engagement through patient portals providing 24/7 access to care plans and health information, automated appointment reminders via patients’ preferred communication channels, educational content delivered at appropriate health literacy levels, progress tracking that gamifies care plan adherence, and telehealth integration that eliminates transportation barriers to care access. These tools convert engagement from a coordination challenge into a strategic advantage.
10. Regulatory burden: when compliance consumes capacity
Healthcare organizations face 629 discrete regulatory requirements across nine domains, consuming nearly $39 billion annually in administrative compliance activities. This regulatory complexity creates significant operational drag that diverts resources from patient care and coordination activities.
An average-sized community hospital dedicates nearly $7.6 million annually to regulatory compliance activities equivalent to $1,200 every time a patient is admitted. These costs represent direct drains on organizational financial performance without corresponding revenue generation. Organizations struggling with manual compliance processes face even higher costs plus exposure to penalties from compliance failures.
Regulatory compliance consumes 59 full-time equivalents at an average hospital, over one-quarter of which are doctors and nurses pulled away from patient care. When compliance documentation requires manual effort, organizations face the impossible choice between staff time spent on compliance versus coordination activities that directly improve patient outcomes.
Care coordination platforms reduce regulatory burden through documentation templates that ensure compliance requirements are met during normal workflows, automated data collection for quality reporting and meaningful use attestation, audit-ready records eliminating time-consuming compliance reviews, and automated alerts flagging potential compliance issues before they become violations. These capabilities enable organizations to maintain rigorous compliance without sacrificing coordination capacity.
The orchestration advantage: transforming challenges into competitive advantages
Leading healthcare organizations are discovering that intelligent care coordination orchestration platforms like blueBriX don’t just solve individual challenges—they transform how care gets delivered. By unifying fragmented data into comprehensive patient views, automating administrative tasks that consume coordinator capacity, leveraging AI to identify risks and predict needs before they become crises, and empowering patients as active partners in their care journeys, these platforms create compounding returns on investment.
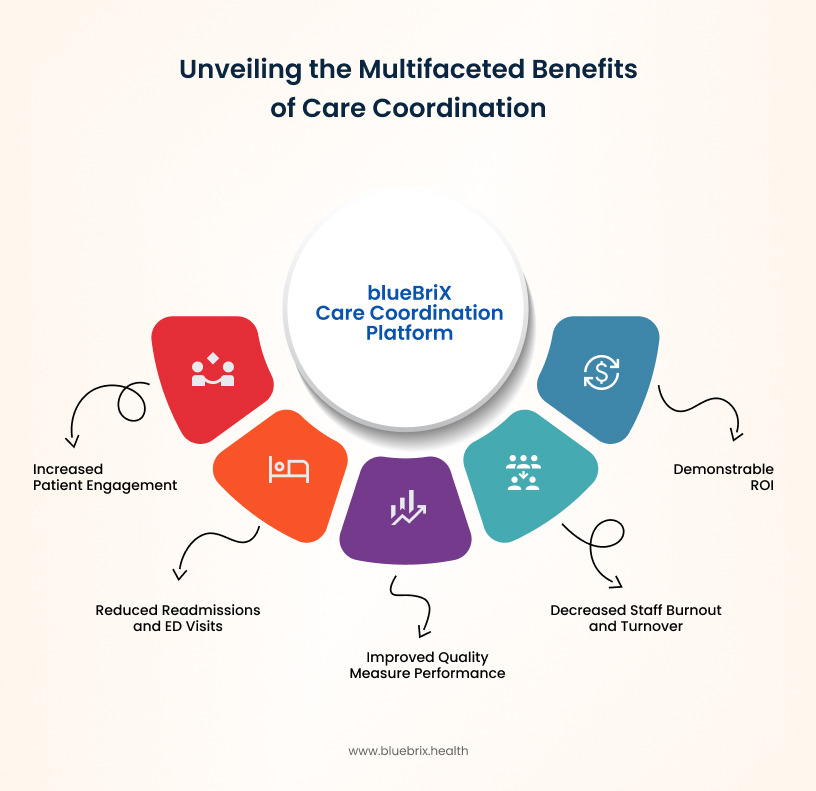
Organizations implementing comprehensive care coordination platforms report measurable outcomes including 30-40% increases in patients engaged per care team member, significant reductions in hospital readmissions and emergency department utilization, improved quality measure performance supporting value-based care success, decreased staff burnout and turnover among coordination teams, and demonstrable ROI within the first year of implementation.
The mathematical reality is straightforward: care coordination failures cost healthcare organizations millions annually through preventable readmissions, duplicate testing, staff turnover, missed quality bonuses, and operational inefficiencies. Each of the ten challenges examined represents multiple opportunities for financial loss and operational drag. Comprehensive coordination platforms systematically address all ten challenges simultaneously, creating cost savings and efficiency gains that far exceed platform investment costs.
The urgency of now: why waiting increases your risk
Healthcare organizations face mounting pressure from multiple directions: value-based care contracts that put increasing percentages of revenue at risk, staffing shortages that make operational efficiency essential, patient and payer expectations for coordinated, seamless care experiences, and competitor organizations implementing advanced coordination capabilities that threaten market position.
The organizations thriving in this environment share a common characteristic: they’ve implemented intelligent care coordination orchestration platforms that transform challenges into competitive advantages. These platforms deliver measurable ROI through reduced readmissions and emergency visits, eliminated duplicate testing and procedures, improved staff productivity and retention, enhanced quality measure performance and value-based care bonuses, and streamlined regulatory compliance.
Perhaps most importantly, comprehensive coordination platforms create scalable infrastructure that supports growth. Organizations attempting to scale value-based care programs or expand patient populations through manual coordination processes quickly hit capacity constraints. Platform-enabled coordination scales efficiently, allowing organizations to manage larger populations with existing staff while maintaining or improving care quality.
Making the investment decision: questions to consider
Healthcare decision-makers evaluating care coordination platforms should examine several critical factors.
- Does the platform integrate seamlessly with your existing EHR and other clinical systems without requiring replacement?
- Can it scale to support your current patient population plus anticipated growth?
- Does it automate the specific workflows consuming the most coordinator time in your organization?
- Can it support your value-based care contracts through risk stratification, care gap closure, and quality reporting capabilities?
- What ROI has the vendor demonstrated with similar organizations?
- How quickly can the platform be implemented without disrupting current operations?
Organizations that have successfully implemented coordination platforms consistently report that the most critical success factor is selecting solutions designed specifically for healthcare coordination challenges rather than adapting generic project management or CRM platforms. Purpose-built healthcare coordination platforms understand the unique requirements of HIPAA compliance, clinical workflows, value-based care reporting, and care team collaboration that generic business tools cannot adequately address.

