Revenue is an absolute necessity for a practice to operate without hindrances. But what does that mean exactly? Historically, the healthcare industry operated on a fee-for-service model of treatment, where providing services or treatments and receiving payment from the patient or reimbursement from the insurance provider was the norm. Factors such as patient outcome, quality of care, or patient satisfaction were not significantly influential on a practice’s revenue. However, the industry has evolved and is now adopting a value-based care model of treatment, which is expected to become the norm in a handful of years. This shift means that to optimize revenue, practices need to fine-tune their workflow, structure, and operations. This includes setting and tracking Key Performance Indicators (KPIs) and other relevant metrics.
For the purposes of this article, we will focus specifically on behavioral health clinics. Behavioral health clinics, whether they are Certified Community Behavioral Health Clinics (CCBHCs), Community Health Mental Centers (CHMCs), outpatient clinics, virtual clinics, clinics for individuals with intellectual and developmental disabilities (IDDs), or substance use disorder (SUD) treatment centers, need to track key performance indicators (KPIs) to ensure they provide high-quality care and operate efficiently.
Here are ten important metrics that every behavioral health clinic should consider, to optimize their revenue:
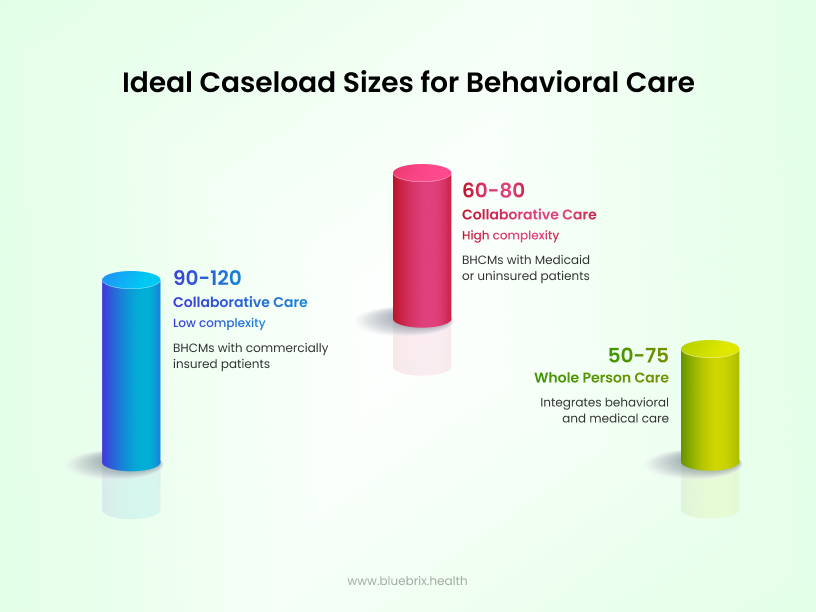
1. Client load or caseload
Effectively managing the number of clients each provider oversees—referred to as “caseload”—is crucial in behavioral health for delivering quality care and ensuring positive outcomes. A manageable caseload allows providers to dedicate adequate time and attention to each client, reducing the risk of burnout and enhancing client satisfaction.
In behavioral health, caseloads are typically measured by the number of clients a provider is responsible for at any given time. However, the complexity of each case significantly influences the ideal caseload size. For instance, intensive case management models, such as Assertive Community Treatment (ACT), often involve smaller caseloads due to the high needs of the clients they serve. ACT teams, comprising 10–12 multidisciplinary professionals, share caseloads to provide continuous, comprehensive care. Factors such as appointment length, client complexity, support systems and service delivery model influence caseload size.
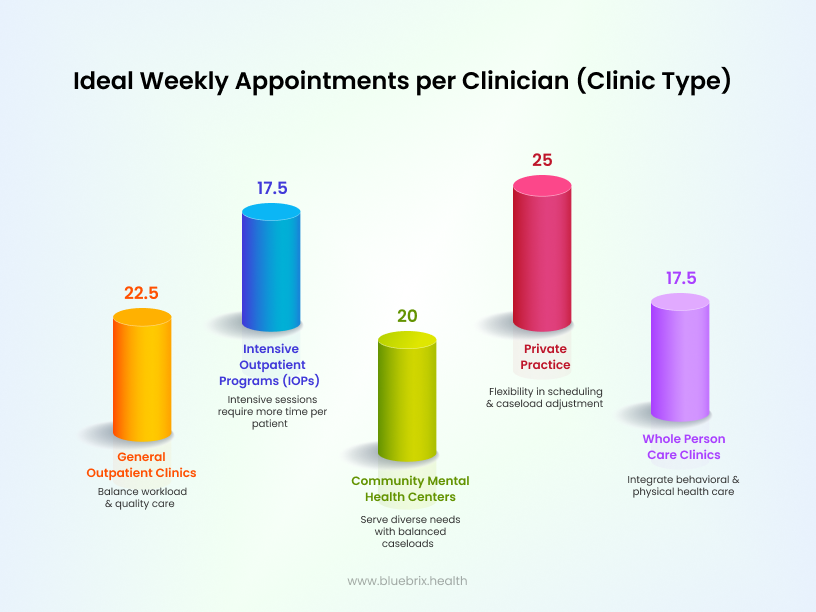
2. Appointments per clinician
Appointment per clinician is a key performance indicator (KPI) used in behavioral health to measure the productivity of clinicians. It tracks the number of appointments each clinician conducts over a specific period, such as daily, weekly, or monthly. This metric helps in understanding workload distribution, identifying potential burnout, and optimizing clinician schedules. It is calculated as follows:
Appointments per clinician = total number of appointments/number of clinicians
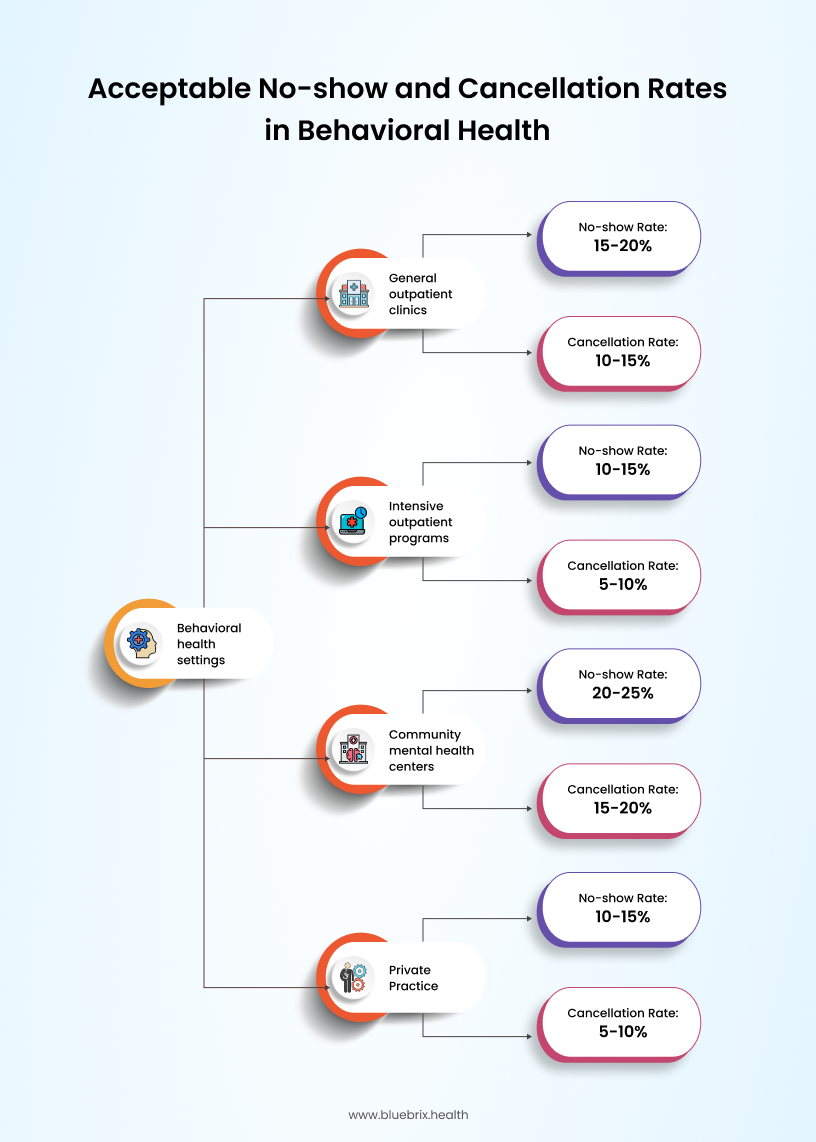
3. No-show and cancellation rates
No-show gauges the percentage of scheduled appointments that were missed and cancellation rate represents the percentage of appointments cancelled by patients. Missed or cancelled appointments are problematic for practices because they lead to no revenue or partial revenue. Gaining insight into this information allows your practice to implement procedures to reduce the percentage of no-shows and cancellations. For example, implementing a text reminder system can be beneficial to reduce these rates. Behavioral health treatment appointments are often scheduled weeks or months apart, making it understandable why a patient might forget them. By sending an automated text reminder 72 hours before the appointment, you can ensure that the patient remembers their appointment and will be able to take the necessary steps to attend their scheduled appointment.
No-show rate = (total number of no-show appointments / number of scheduled appointments) ×100
Cancellation rate = (total number of cancelled appointments / number of scheduled appointments) ×100
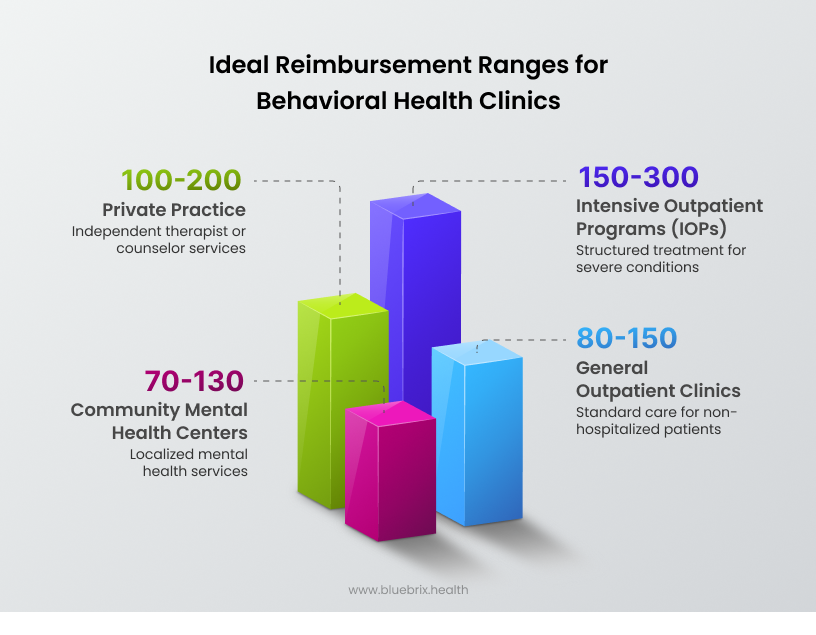
4. Revenue and reimbursement
Revenue in behavioral health refers to the total income generated from providing mental health and substance use disorder services. Reimbursement Rates are the amounts that healthcare providers receive from insurance companies, Medicare, Medicaid, or other payers for the services they deliver. These metrics are crucial because they ensure that your billing process is running effectively and efficiently, allowing you to operate seamlessly without financial difficulties.
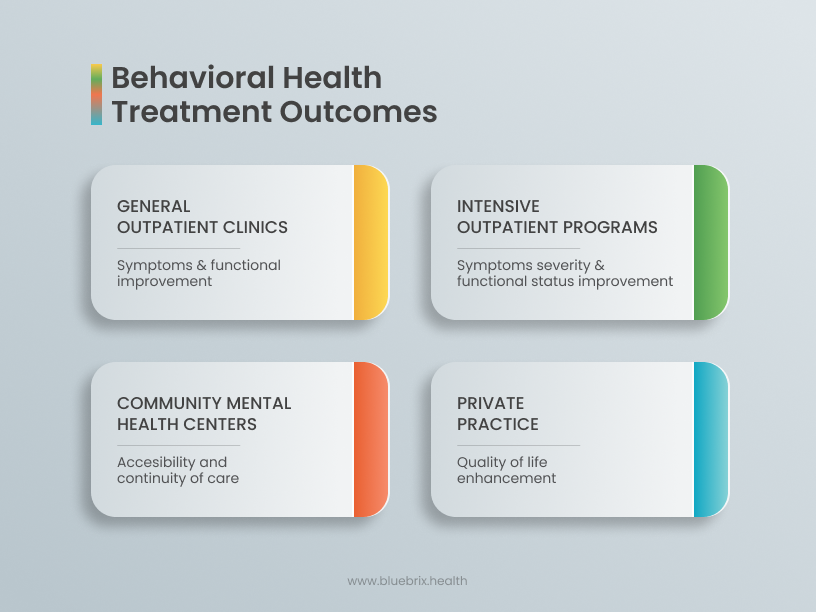
5. Client satisfaction and outcomes
This metric is a KPI that must be tracked by all those who are part of the value-based care model of treatment, as it determines their reimbursement. Tracking this information through methods such as collecting patient feedback through surveys, following up with patients, or keeping track of rehospitalization rates allows practices to consistently improve and meet requirements necessary to be compliant with the value-based care model.
Measuring client satisfaction and outcomes in behavioral health involves using a combination of subjective and objective tools to assess the quality of care and its impact on patients. Here’s a comprehensive overview of how these are measured:
Measuring client satisfaction
- Surveys and questionnaires:
- Tools like the Client Satisfaction Questionnaire (CSQ), Consumer Assessment of Healthcare Providers and Systems (CAHPS), Mental Health Surveys and the Service Satisfaction Scale (SSS) are commonly used to gauge satisfaction with services received.
- The Self-Help Agency Satisfaction Scale (SHASS) measures satisfaction with involvement in treatment decisions and services.
- Feedback sessions:
- Regular feedback sessions with clients help identify areas for improvement and assess overall satisfaction with care.
- Net promoter score (NPS) and patient satisfaction score (CSAT):
- These metrics measure client loyalty and satisfaction by asking how likely they are to recommend services to others.

Measuring outcomes
- Objective outcome measures:
- Symptom severity scales: Tools like the PHQ-9 for depression and GAD-7 for anxiety quantify symptom changes over time.
- Physiological indicators: These include measures of physical health that can be impacted by mental health treatments.
- Subjective outcome measures:
- Patient-reported outcome measures (PROMs): Clients report on their own symptoms and functioning, providing a personal perspective on treatment effectiveness.
- Self-report questionnaires: These capture changes in mood, coping mechanisms, and overall well-being.
- Clinician-rated measures:
- Observation-based assessments: Clinicians evaluate patient progress through observations and clinical interviews.
- Treatment-specific measures: Tools like the Cognitive Fusion Questionnaire (CFQ) for Acceptance and Commitment Therapy (ACT).
- Behavioral Health EHRs:
- Purpose-built EHRs like blueBriX can track client progress in real-time, helping clinicians make data-driven decisions.
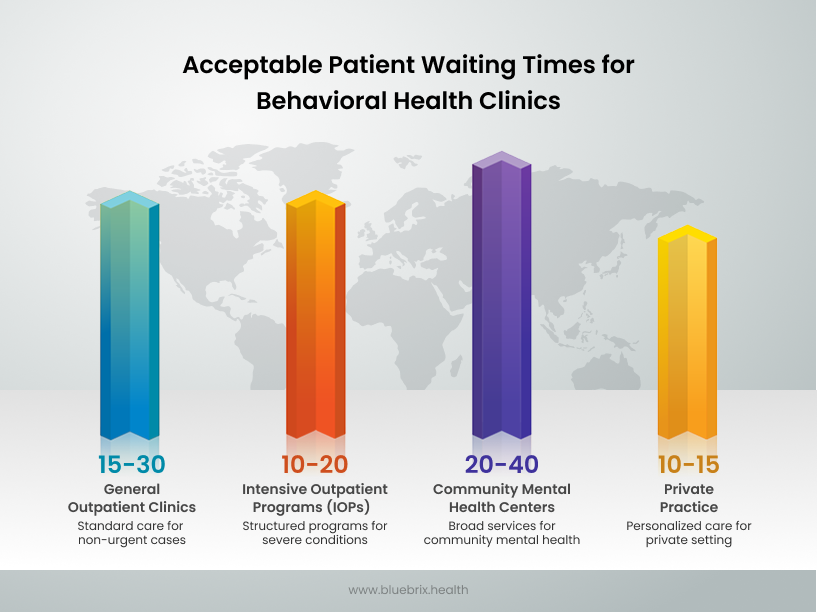
6. Patient wait time
This metric tracks the average patient wait time during an appointment before they are able to get face-to-face or one-on-one time with the provider. For example, if a patient arrives the clinic at 10:00 AM and is seen at 10:30 AM, the wait time is 30 minutes. This metric is helpful because long wait times are undesirable and might cause patients to no-show or cancel their appointment or seek treatment elsewhere. By reducing patient wait time, practices can improve patient satisfaction, reduce the probability of no-shows or cancellations, and improve efficiency and resource utilization.
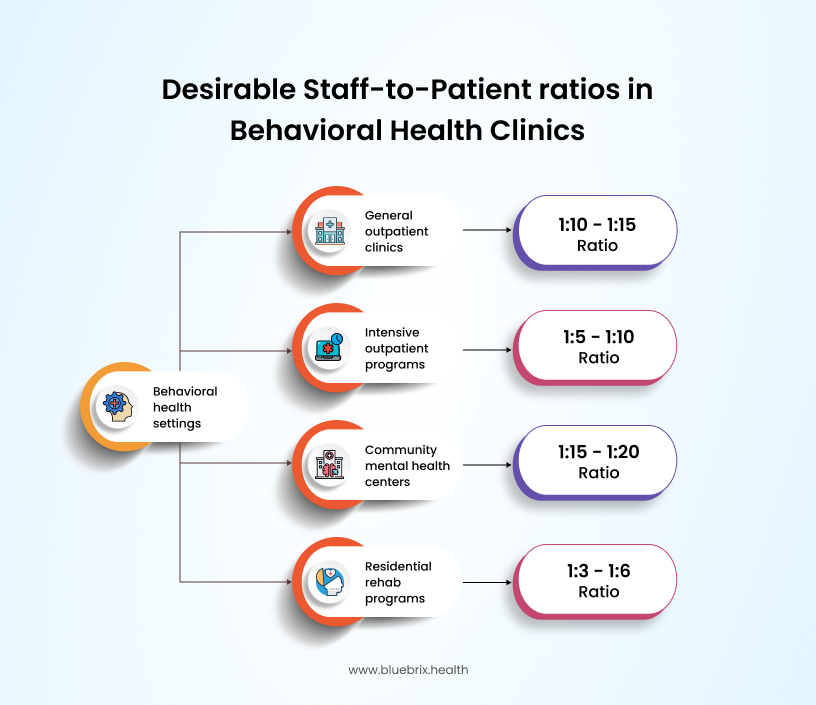
7.Staff-to-patient ratio
This metric informs you of the ratio of staff members to patients. This is important because an unbalanced ratio could lead to staff members feeling overwhelmed and burned out, negatively impacting the quality of care they provide, which would negatively impact patient health and patient satisfaction. Maintaining a balanced ratio of staff to patients greatly reduces this risk and benefits both the patient and all involved in the provision of treatment, as care can be provided in a personalized and more effective manner. It is calculated as number of staff members divided by the number of patients.
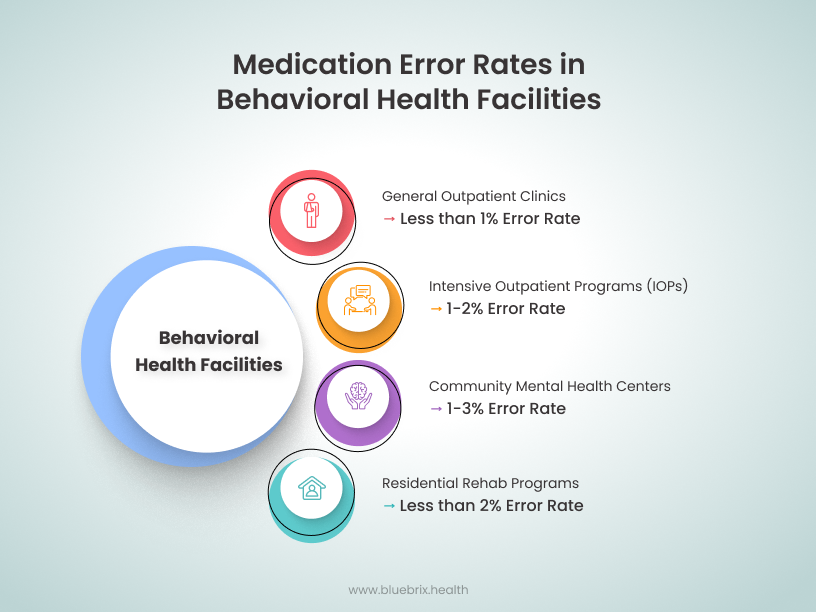
8. Medication errors
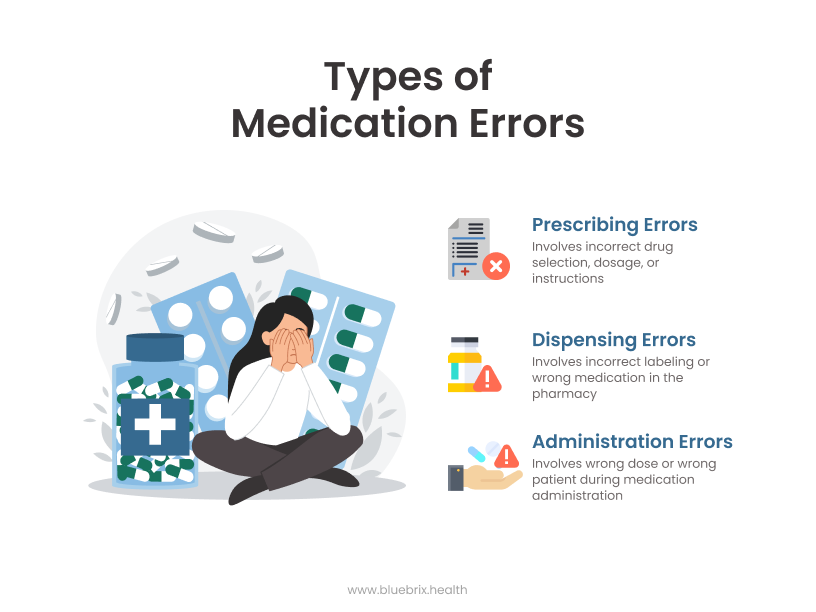
Medication errors in behavioral health refer to mistakes in prescribing, dispensing, or administering medications. These errors can occur at any stage of the medication management process and can have serious consequences for patient safety and treatment outcomes. This metric provides important insight into medication administration and whether it is being done correctly. This metric is critical because it concerns patient safety. Ensuring that you have a medication management system that works correctly and that staff are knowledgeable and receive regular training can help prevent medication errors.
Medication error rate = (number of medication errors / total number of medications administered) × 100
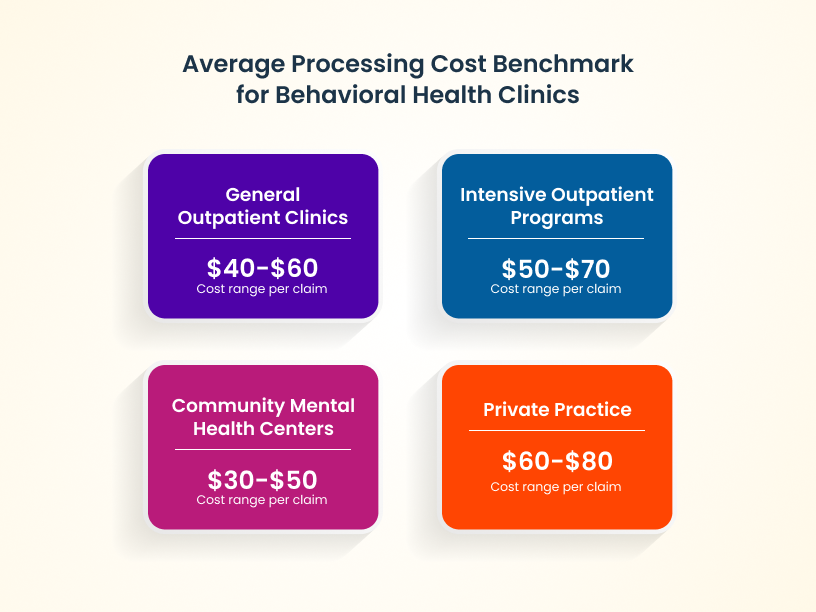
9. Average insurance claim processing time and cost
This metric provides an understanding of the costs and time involved in filing claims and receiving reimbursements. Insurance Claim Processing Time refers to the duration it takes for an insurance claim to be processed from the time it is submitted until the payment is received. Insurance Claim Processing Cost refers to the expenses incurred in processing these claims, including administrative and operational costs. This is an important metric to track because the claims process can be impacted by many variables, such as proper coding, correctly entered information, and achieving pre-authorization. Understanding which variables can be improved upon and made more efficient and streamlined can significantly improve processing times while reducing the risk of denial or partial reimbursement.
Average processing time = total processing time for all claims / number of claims processed
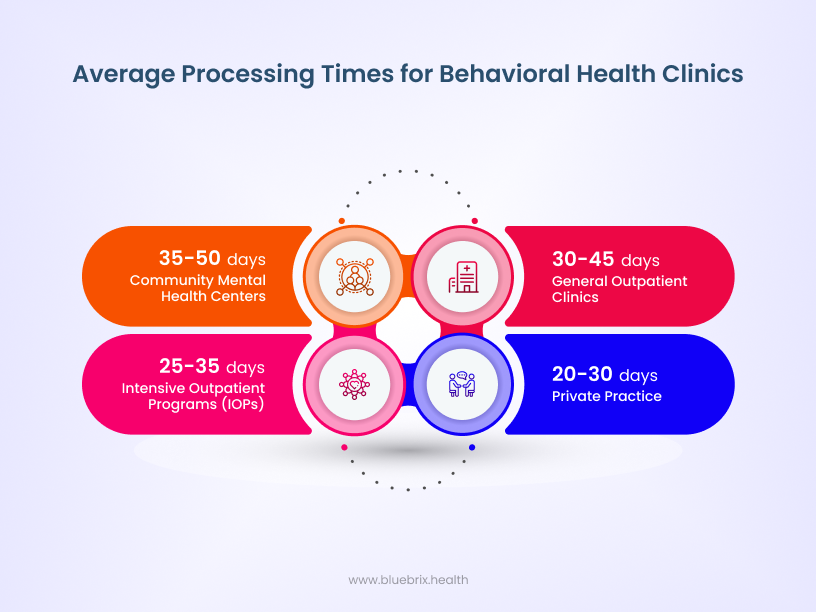
Average processing cost = total cost of processing claims / number of claims processed
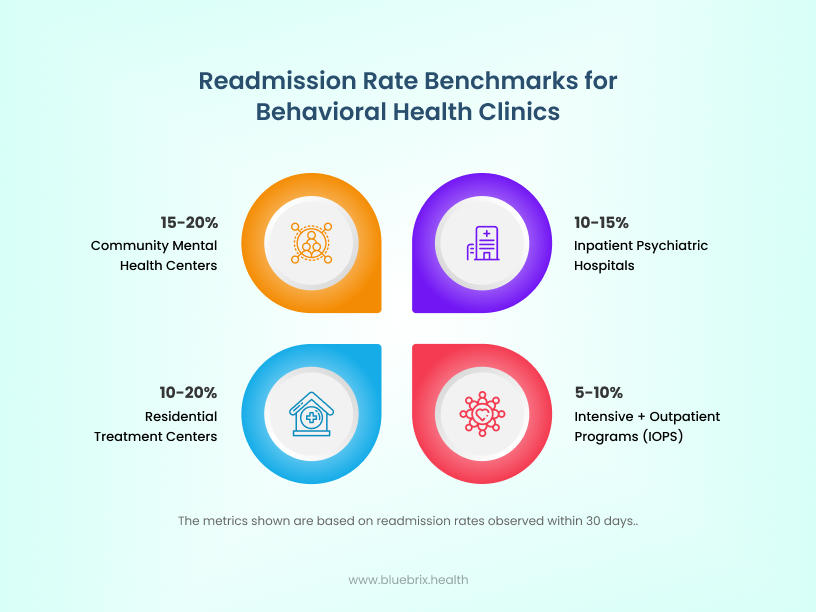
10. Readmission rate
This metric tracks the percentage of patients who are readmitted to a behavioral healthcare facility within a specific period after being discharged. It is often used to assess the quality of care and the effectiveness of discharge planning. Lower readmission rates indicate effective treatment and follow-up care. This is particularly relevant for CCBHCs and SUD clinics, where ongoing care and relapse prevention are critical. While readmission rates are less commonly used for IOPs and outpatient clinics, these settings may track return visits or recurrence rates to monitor the need for additional care or adjustments in treatment plans.
Readmission Rate = (Number of readmitted patients within a specific period / Total number of discharged patients) x 100
Optimizing revenue and operations in a behavioral health clinic requires a multi-pronged approach. Tracking the right metrics is crucial for the success of any behavioral health clinic. As the healthcare ecosystem continues to evolve, staying adaptable and proactive will be crucial for continued success. By monitoring key performance indicators, leveraging technology, investing in staff training, fostering collaboration, and prioritizing patient-centered care, behavioral health clinics can achieve sustainable growth, deliver high-quality service and receive satisfactory revenue accrual. However, managing these metrics effectively requires robust tools and systems. That’s where blueBriX comes in. With our end-to-end purpose-built behavioral health EHR solutions, you can streamline your operations, enhance patient care, and gain valuable insights into your clinic’s performance.

