Healthcare organizations across the United States are facing an unprecedented economic challenge. With annual healthcare spending exceeding $4.3 trillion and 20-40% of that classified as waste, the industry desperately needs solutions that don’t just improve care—they fundamentally transform how healthcare economics work. Enter Fast Healthcare Interoperability Resources (FHIR), a game-changing standard that’s not just about connecting systems, but about unlocking massive economic value across the entire care continuum.
The numbers tell a compelling story: healthcare organizations implementing FHIR-based interoperability solutions are seeing $3.20 in return for every $1 invested, with some seeing returns within just 14 months. But this is just the beginning of a much larger economic transformation that could reshape healthcare delivery as we know it.
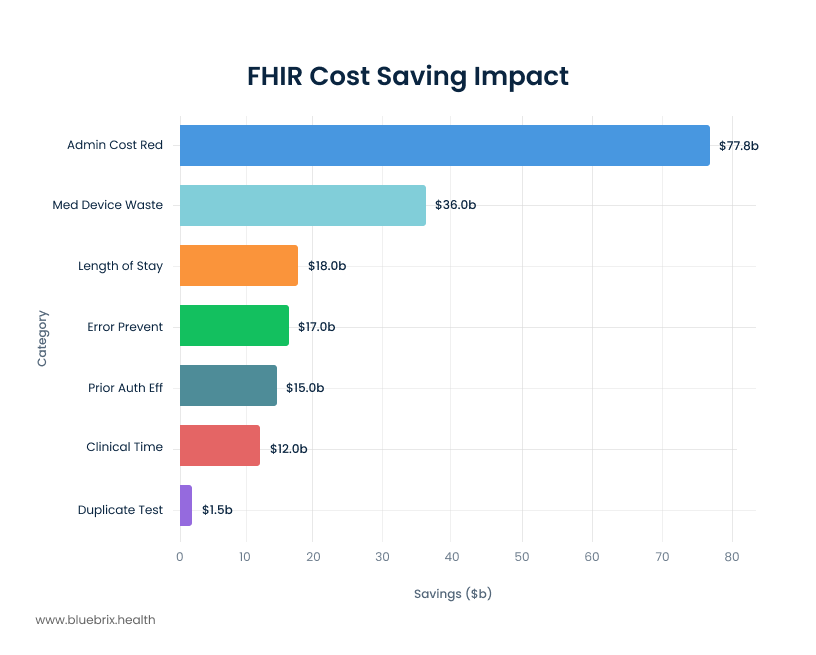
Annual Healthcare Cost Savings Potential Through FHIR Interoperability Implementation
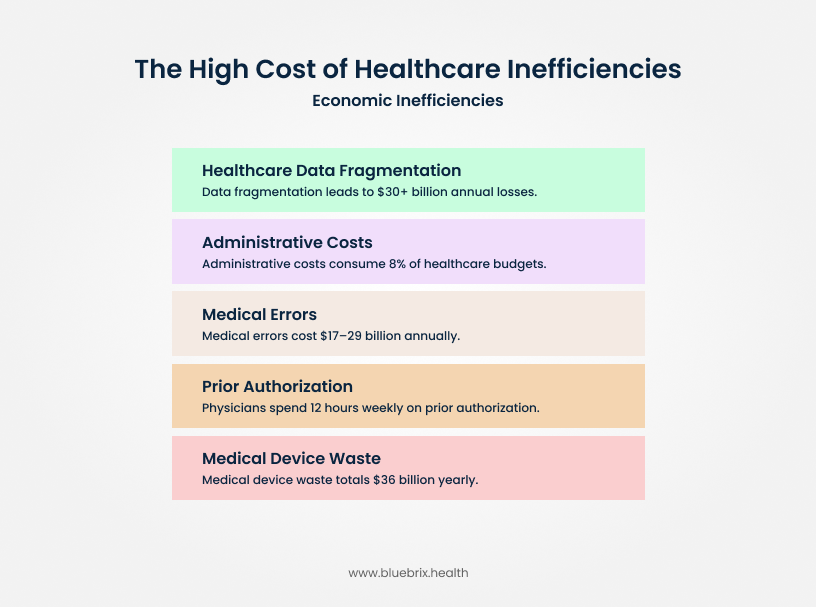
The $935 Billion Problem: Understanding Healthcare’s Economic Crisis
Before diving into FHIR’s economic impact, we need to understand the scope of healthcare’s cost crisis. The United States spends more per capita on healthcare than any other developed nation, yet ranks poorly in health outcomes. According to a landmark 2019 study in the Journal of the American Medical Association (JAMA), this inefficiency results in an estimated $760 billion to $935 billion in annual waste. The root cause? A fragmented system where fewer than one in three hospitals can electronically find, send, receive, and integrate patient information from other providers.
This fragmentation creates a cascade of economic inefficiencies:
- $30+ billion annually lost due to healthcare data fragmentation
- Administrative costs consuming 8% of healthcare budgets due to manual processes
- Medical errors costing $17-29 billion yearly, many preventable with better information sharing
- Physicians spending 12 hours weekly on prior authorization processes alone
- $36 billion in medical device waste in inpatient settings due to lack of interoperability
The healthcare interoperability solutions market has exploded in response, growing from $4.53 billion in 2024 to a projected $14.47 billion by 2029—a staggering 13.89% CAGR that reflects the urgent demand for solutions.
FHIR’s Unique Position to Drive Economic Value
FHIR represents more than just a technical standard—it’s an economic catalyst that transforms healthcare’s cost structure. Unlike previous interoperability attempts that were complex and expensive to implement, FHIR leverages modern web technologies to create a cost-effective, scalable foundation for data exchange.
The inherent design of FHIR positions it uniquely to drive substantial economic value across the healthcare spectrum. By providing a standardized means for representing and sharing information, FHIR ensures consistency regardless of how local EHRs may store their data. This consistency is paramount for reducing discrepancies and errors, which directly translate into tangible cost savings.
The ability to access data in real-time fundamentally transforms healthcare operations. It enables faster, more informed clinical decision-making, allowing providers to act swiftly and accurately. Moreover, this real-time capability streamlines administrative tasks, reducing the manual effort and associated costs. FHIR’s adoption of common web standards (RESTful APIs, JSON) and its modular “resource” approach makes it inherently easier for developers, including those outside traditional healthcare IT, to build and integrate applications. This ease of use, combined with its “free to use” status and major vendor support, creates a powerful network effect. The simplicity and accessibility of FHIR are not merely technical advantages; they are economic accelerators. By lowering the barrier to entry for innovation, FHIR fosters a more competitive and dynamic health tech market, driving down the cost of developing and integrating new solutions, and ultimately benefiting healthcare organizations through a wider array of affordable, interoperable tools.
Furthermore, FHIR’s role in creating a “single source of truth” for patient data and standardizing its representation, irrespective of local EHR storage methods, directly addresses the pervasive problem of fragmented data and inconsistencies that plague current systems. This capability is foundational to unlocking systemic cost savings. It moves beyond mere data exchange to data cohesion, which is essential for accurate diagnoses, reduced errors, and efficient resource allocation across the entire care continuum. This semantic interoperability represents a higher-order benefit than simple data transfer, enabling a truly unified and efficient healthcare environment.
Breaking Down the $51+ Billion Opportunity
Conservative estimates suggest that full FHIR implementation could save the U.S. healthcare system $51+ billion annually. This isn’t theoretical—it’s based on measurable improvements across key cost categories:
Administrative Cost Reduction: The Biggest Win
Administrative inefficiencies represent the largest opportunity, with potential 60-70% reduction in administrative costs related to data sharing. Healthcare organizations currently spend enormous resources on:
- Manual data entry and phone calls to obtain records
- Faxing documents between providers
- Staff time spent tracking down patient information
- Redundant data collection across multiple systems
FHIR automates these processes, with organizations reporting dramatic reductions in administrative burden within months of implementation.
Medical Device Waste Elimination: $36 Billion Opportunity
One of the most frequent pain points and significant cost drivers in healthcare is the duplication of diagnostic tests, including lab work, imaging studies, and specialized screenings. Patients who transfer between different facilities or consult multiple specialists often undergo repeat tests simply due to a lack of accessible prior records.
The West Health Institute identified that widespread medical device interoperability could eliminate at least $36 billion of waste in inpatient settings alone through:
- Reducing adverse events through safety interlocks ($1.9 billion)
- Eliminating redundant testing ($1.5 billion)
- Reducing clinician time on manual data entry ($12 billion)
- Shortening length of stay through faster information transmission ($18 billion)
A regional network that utilized HL7 v2 (a precursor to FHIR, often bridged by FHIR for modern integration) to standardize data exchange among six affiliated hospitals successfully identified and eliminated duplicative imaging orders. This initiative resulted in a reduction of approximately 6% of overall imaging costs and freed up valuable staff time previously spent reconciling inconsistent patient records. More broadly, the automation of data exchange processes facilitated by FHIR has led to a 30% reduction in data processing costs across healthcare organizations.
A compelling case study involving a 300-bed community hospital illustrates this impact: by implementing a FHIR-based interface with an external lab provider, the hospital achieved a 20% reduction in lab turnaround times. This improvement directly led to an average one-day decrease in inpatient length of stay for certain conditions, resulting in a 10% reduction in lab-related costs and a faster bed turnover that boosted patient intake capacity.
Another study demonstrated a 25-35% reduction in referral leakage and saved 40+ staff hours per month with automation in referral management.
Prior Authorization: From $120 Cost to Automated Efficiency
Prior authorization represents one of healthcare’s most expensive administrative processes, with each transaction costing $80-120 for payers to process. The CMS estimates that automating prior authorizations could save the industry $15 billion annually.
FHIR-based prior authorization solutions are delivering remarkable results:
- Real-time authorization decisions replacing week-long waiting periods
- Dramatic reduction in physician administrative burden from the current 12 hours weekly
- Improved provider and patient satisfaction through streamlined processes
- Reduced claim rejections through better documentation and communication
Health Information Exchange: Measurable ROI
Studies of Health Information Exchange (HIE) platforms show concrete economic benefits:
- 25-26% reduction in laboratory tests when providers query HIE databases
- 26-47% reduction in radiology examinations in emergency departments
- Medicare spending dropped by 1.4% overall in regions with HIE systems
- 6.7% spending reduction in regions with mature exchange systems
New York’s statewide HIE alone has demonstrated significant cost reductions while improving care coordination across the state’s diverse healthcare landscape.
Clinical Efficiency: Time Equals Money
FHIR’s impact on clinical workflows translates directly to economic benefits:
- Physicians spend 16 minutes per patient encounter searching for external health information
- Seamless interoperability could reduce this to 3-4 minutes, allowing providers to see more patients or spend more quality time with each patient
- Emergency department length of stay reduced by 15-20 minutes per patient when providers have immediate access to medical histories
- 30% reduction in after-hours charting through automated documentation processes
Minimizing Medical Errors and Improving Patient Safety
Medical errors are a devastating and costly problem in healthcare, leading to adverse events, prolonged inpatient stays, and increased readmission rates. FHIR plays a crucial role in mitigating these risks.
- Single Source of Truth: FHIR, in conjunction with HL7 standards, facilitates the creation of a “single source of truth” for patient data. This unified data environment allows all stakeholders—from primary care physicians to cardiologists and endocrinologists—to collaborate effectively. This cohesive data access significantly reduces the risk of conflicting treatments or medication errors, which can otherwise lead to severe adverse events, extended hospitalizations, or readmissions, all of which drive up healthcare costs.
- Faster and Correct Diagnoses: When patient information flows more rapidly and is readily accessible, doctors are empowered to make more accurate and timely decisions, leading to fewer errors. This improved data access also helps prevent the ordering of unnecessary tests, further contributing to cost savings.
- Improved Patient Outcomes: The direct result of accurate diagnoses and a reduction in medical errors is a significant improvement in patient outcomes. Better outcomes, in turn, reduce the need for costly interventions, extended care, and subsequent readmissions, creating a virtuous cycle of efficiency and cost reduction.
Value-Based Care: FHIR’s Strategic Economic Impact
FHIR’s most significant economic impact may be its role in enabling value-based care (VBC) models. As healthcare shifts from fee-for-service to outcome-based payments, organizations need sophisticated data capabilities to succeed:
Quality Measure Automation
FHIR enables automated quality measure reporting, eliminating the manual processes that traditionally consume significant resources:
- Digital Quality Measures (dQMs) provide real-time insights instead of retrospective reporting
- Automated HEDIS reporting reduces administrative burden on health plans
- Real-time population health management enables proactive interventions
Risk Adjustment Optimization
Up to 30% of conditions affecting risk adjustment scores are underdocumented by providers. FHIR-based systems enable:
- Real-time clinical data integration for more accurate risk assessments
- Better documentation through automated prompts and suggestions
- More appropriate reimbursements based on complete patient pictures
Care Coordination at Scale
FHIR facilitates the kind of seamless care coordination that VBC models require:
- 37% reduction in preventable ER visits through better care coordination
- 25% reduction in hospital readmissions via improved transitions of care
- $83-106 monthly Medicare cost reduction per point increase in care coordination scores
Chronic Disease Management and Preventive Care
Chronic conditions represent a massive financial drain on the U.S. healthcare system, accounting for approximately 90% of the nation’s $4.5 trillion in annual healthcare expenditures. VBC models strategically emphasize proactive interventions aimed at preventing disease progression and complications, thereby reducing reliance on more expensive emergency and inpatient care.
FHIR is instrumental in the effective management of chronic diseases, enabling continuous monitoring and dynamic adjustments to care plans. For example, FHIR-enabled systems can seamlessly integrate data from a variety of sources, including wearables and home monitoring devices, into electronic health records (EHRs). This allows care managers to track patient progress in real-time and adjust treatments as needed, ensuring timely and personalized interventions. This advanced integration supports the proactive management of prevalent conditions like diabetes and heart disease, leading to a reduction in hospital admissions and a significant improvement in patients’ quality of life. Studies consistently show that digital health interventions, such as remote patient monitoring, can substantially reduce healthcare utilization for individuals with chronic conditions.
Reducing Hospital Readmissions and Emergency Department Utilization
Hospital readmissions are a persistent and costly challenge in healthcare, contributing to increased expenditures, significant resource strain, and poorer patient outcomes. In 2018, the U.S. experienced 3.8 million 30-day all-cause adult hospital readmissions, with an average cost of $15,200 per readmission. Notably, conditions such as septicemia, heart failure, diabetes, and COPD collectively accounted for one in five of all readmissions.
VBC models actively leverage data-driven approaches, including predictive analytics and sophisticated care coordination strategies, to minimize both readmissions and unnecessary ED utilization. FHIR’s capacity to facilitate real-time data sharing ensures that providers possess a complete and up-to-date picture of a patient’s health status, thereby significantly reducing the likelihood of avoidable readmissions. A compelling study revealed that remote patient monitoring, made possible by interoperable data exchange, resulted in a remarkable
44% reduction in hospital readmissions and a 38% reduction in emergency room visits for patients managing chronic conditions. Another case study highlighted a 30% reduction in patient hospital readmissions achieved through effective care coordination and the strategic implementation of remote patient monitoring features.
Quantifiable Benefits of FHIR Implementation
Cost Savings
- Estimated savings from automating prior authorizations (industry-wide, 10 years): $15 billion
- Potential annual savings from administrative overhead and error reduction (US healthcare system): Up to $40 billion
- Annual savings for healthcare providers from reduced administrative tasks (AMA): Up to $200 million
- Reduction in data processing costs: 30%
- Decrease in IT maintenance costs: 30%
- Reduction in lab-related costs (case study): 10%
- Reduction in imaging costs (case study): ~6%
These savings show how interoperability directly cuts waste, reduces overhead, and frees up resources for better care delivery.
Efficiency Gains
- Increase in clinical efficiency: 20%
- Reduction in lab turnaround times (case study): 20%
- Average decrease in inpatient length of stay (case study): 1 day
- Staff hours saved per month from referral automation: 40+ hours
- Automation of prior authorization requests (payer case study): Up to 70%
- Faster identification and closure of care gaps: 83%
Efficiency improvements highlight how FHIR accelerates workflows, shortens timelines, and enables clinicians to focus more on patients than paperwork.
Clinical & Patient Outcomes
- Reduction in hospital readmissions (remote patient monitoring): 44%
- Reduction in emergency room visits (remote patient monitoring): 38%
- Reduction in patient hospital readmissions (care coordination case study): 30%
- Reduction in referral leakage: 25–35%
- Improved HEDIS measure scores: 41%
️Better outcomes make the economic case even stronger—when interoperability improves care, both patients and organizations win.
The Regulatory Imperative: Mandating Interoperability
The journey to a truly connected healthcare system is being accelerated not just by innovation, but by powerful regulatory mandates. While the clinical and economic benefits of interoperability have long been understood, a series of federal rules have turned the abstract idea of data sharing into a non-negotiable requirement. This regulatory push is fundamentally shifting the incentives for every player in the healthcare ecosystem, from data hoarding to data liquidity.
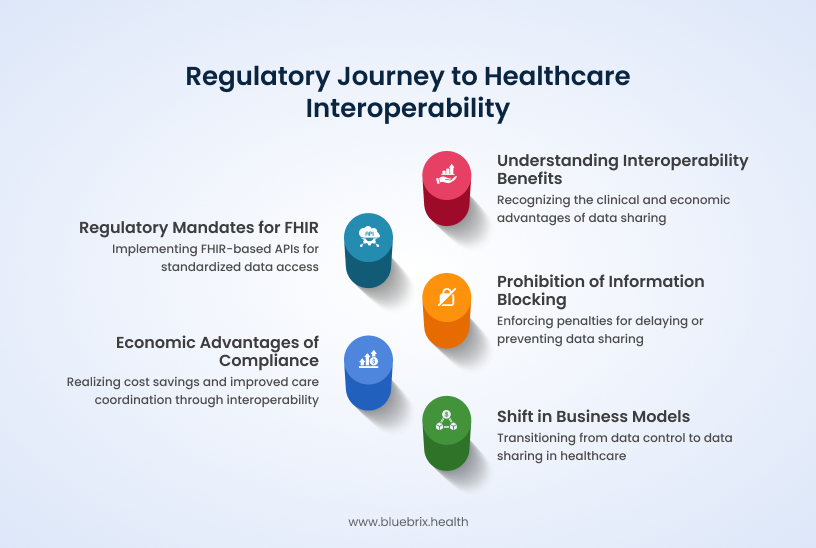
- The Mandate for FHIR: Landmark legislation like the 21st Century Cures Act and subsequent rules from the ONC and CMS have mandated the use of FHIR-based APIs. These mandates require health IT vendors, EHRs, and even payers to make patient data available in a standardized, accessible format, creating a baseline level of interoperability across the industry.
- Penalizing Information Blocking: A core component of this regulatory framework is the explicit prohibition of “information blocking”—the intentional act of delaying or preventing the sharing of electronic health information. The government is backing this with stiff penalties, including fines of up to $1 million per instance for health IT developers and health information networks. This threat of severe financial repercussions creates a powerful incentive to invest in data-sharing solutions.
- From Burden to Benefit: While regulations can feel like a burden, compliance with FHIR mandates offers significant economic advantages. By embracing interoperability, healthcare organizations can streamline claims processing, reduce operational costs, and improve care coordination. The regulatory pressure is fostering a more competitive market, ultimately leading to lower interoperability costs and a wider array of innovative solutions.
- Reshaping the Business Model: The ongoing regulatory focus on information blocking signals a fundamental shift in the competitive landscape. It rewards those who embrace interoperability and penalizes those who resist, compelling a change in business models from data control to data sharing—a necessary step for the success of collaborative care and value-based payment initiatives.
Implementation Economics: Getting Started with FHIR
The economic case for FHIR implementation is compelling, but organizations need to understand the investment required and timeline for returns:
Implementation Costs and Timelines
- FHIR implementation typically takes 2-8 weeks for standard deployments
- No licensing costs for using the FHIR framework itself
- Reduced integration costs compared to custom interface development
- Scalable architecture that grows with organizational needs
ROI Timeline and Measurement
Organizations implementing FHIR-based solutions report:
- ROI within 14 months on average
- $3.20 return for every $1 invested across multiple studies
- Immediate administrative cost savings from day one of implementation
- Cumulative benefits that increase over time as more systems connect
The Competitive Advantage of Early FHIR Adoption
Healthcare organizations that implement FHIR early gain significant competitive advantages:
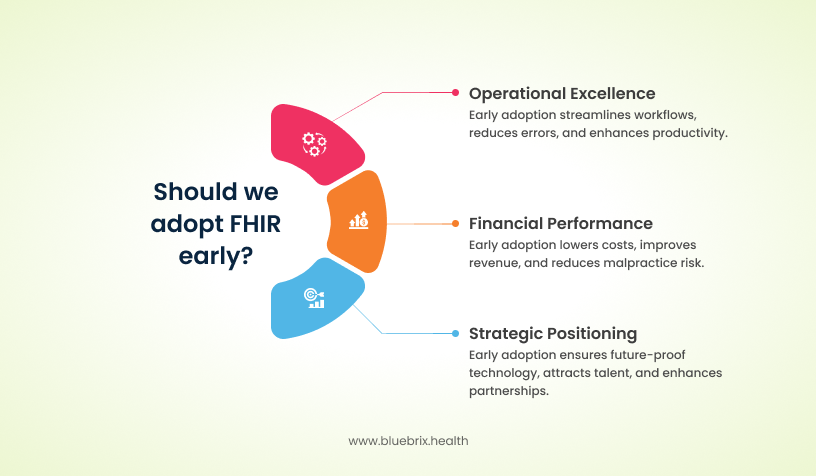
Operational Excellence
- Streamlined workflows that reduce staff burden and improve job satisfaction
- Faster clinical decision-making through complete patient information
- Reduced errors and improved patient safety outcomes
- Enhanced productivity allowing organizations to do more with existing resources
Financial Performance
- Lower administrative costs compared to organizations with fragmented systems
- Improved revenue cycle performance through better documentation and reduced claim rejections
- Enhanced ability to succeed in value-based contracts through better data and coordination capabilities
- Reduced malpractice risk through improved information sharing and care coordination
Strategic Positioning
- Future-proof technology architecture that adapts to new requirements
- Ability to attract and retain top talent through modern, efficient workflows
- Enhanced partnerships with other organizations through seamless data sharing
- Regulatory compliance that positions organizations ahead of future requirements
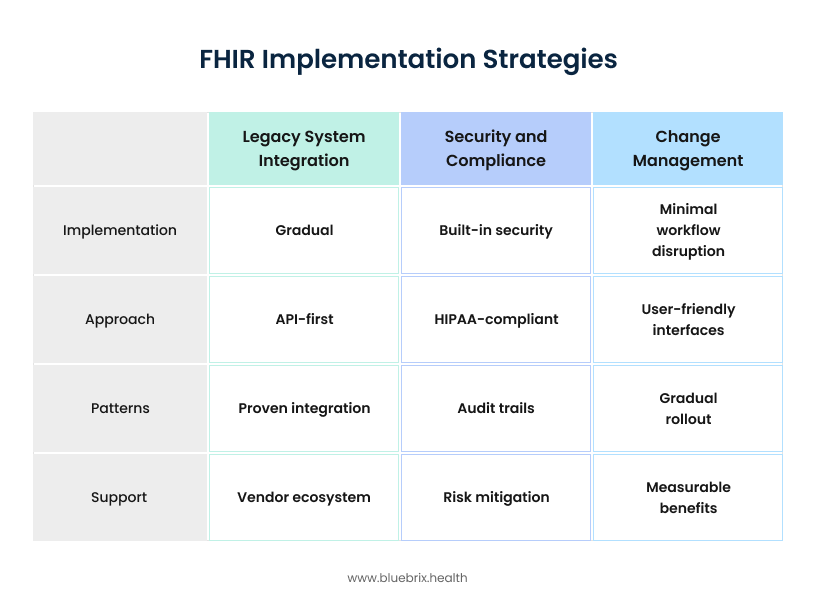
How to Conquer FHIR Implementation Headaches
While FHIR’s economic benefits are substantial, organizations often face implementation challenges that can be addressed through strategic planning.
- Data Standardization and Legacy Systems: Many hospitals operate on legacy EHR systems with siloed data stored in non-standard formats, making mapping to FHIR resources complex. Effective solutions involve conducting thorough data inventory and mapping exercises, utilizing middleware platforms or FHIR adapters to translate legacy formats, and implementing a Master Patient Index (MPI) to resolve duplicate records.
- Inconsistent FHIR Implementation: Different EHR vendors may implement FHIR resources inconsistently, hindering seamless interoperability. Aligning on the US Core Implementation Guide (IG) and actively engaging with FHIR Accelerators like the Da Vinci Project can provide crucial guidance and promote standardization.
- Security and Privacy Concerns: FHIR’s open, API-first architecture necessitates robust security measures to prevent data breaches and unauthorized access. Implementing SMART on FHIR protocols with strong OAuth2 authentication, applying role-based access controls (RBAC), and conducting regular penetration testing and security audits are critical safeguards.
- Staffing Shortages and Lack of FHIR Expertise: The implementation of FHIR requires specialized skills in architecture, development, and data analysis, which can be scarce. Investing in FHIR training programs and certifications, partnering with experienced interoperability consultants or health IT vendors, or leveraging low-code/no-code FHIR platforms can address this talent gap.
- Change Management and Workflow Integration: Technical integration alone is insufficient; successful FHIR adoption requires a redesign of clinical workflows to ensure applications are effectively utilized by staff and do not disrupt care delivery. Involving clinical stakeholders early in the design phase, conducting pilot testing with iterative feedback loops, and integrating FHIR apps seamlessly into existing EHR interfaces are essential.
- Versioning and Upgrades: FHIR is a dynamic standard, with new versions (R4, R5, and R6 in development) introducing changes. Hospitals must ensure their systems remain compatible over time. Standardizing on normative versions like R4 and implementing robust version control policies are best practices for managing this evolution.
- Upfront Investment: Initiating FHIR implementation requires an initial investment of time, dedicated staff, and financial resources. However, the evidence suggests that investing early yields significant long-term returns through improved efficiency and superior patient outcomes.
The high adoption rates among hospitals and clinicians by 2019 and the continued anticipated increase demonstrate a growing momentum. The quantifiable ROI figures from early adopters provide a strong incentive for others. Conversely, the challenges faced by those still relying on legacy systems highlight the increasing cost of not adopting FHIR. Organizations that proactively invest in FHIR implementation are gaining a significant “early adopter advantage” in terms of cost savings and efficiency. Those lagging behind face not only higher operational costs but also increasing competitive disadvantage and potential regulatory non-compliance risks, effectively turning inaction into a growing financial liability.
The challenges section emphasizes “staffing shortages and lack of FHIR expertise” and “change management and workflow integration.” The solutions provided, such as investing in training and involving stakeholders, are not purely technical. This highlights that successful FHIR adoption and the realization of its economic benefits depend heavily on organizational readiness and human factors, not just technology. The ROI of FHIR is not solely dependent on the technology itself, but on the strategic investment in “soft” factors like workforce training, robust change management, and cultivating a culture that values data sharing. These investments are critical for maximizing the quantifiable financial returns and ensuring the long-term success of interoperability initiatives.
Looking Forward: The Future Economics of FHIR
FHIR isn’t a static solution; it’s a dynamic framework that continuously evolves to meet the complex demands of healthcare. While FHIR Release 4 (R4) is the current standard, newer versions like R5 and the upcoming R6 are designed to improve security, streamline workflows, and ensure long-term stability with greater backward compatibility. This constant evolution ensures FHIR’s role as the indispensable foundation for future innovations.
Powering AI and Advanced Analytics
FHIR is the essential enabler for unleashing the full potential of AI in healthcare. AI models rely on accurate, real-time, and standardized data, which is precisely what FHIR provides. This powerful partnership between FHIR and AI enables several transformative capabilities:
- Predictive Analytics: FHIR-fueled AI can identify at-risk patients, allowing providers to proactively intervene and prevent costly complications.
- Clinical Decision Support: FHIR’s architecture allows AI systems to provide real-time recommendations directly within EHRs, improving diagnostic accuracy and patient outcomes.
- Population Health Management: By analyzing vast amounts of standardized health data, AI can help organizations identify trends and effectively manage chronic conditions across entire patient populations.
- Personalized Medicine: FHIR’s ability to aggregate comprehensive data from multiple systems enables AI to create highly tailored treatment plans, moving healthcare toward a truly personalized approach.
A Vision for a Truly Interconnected Ecosystem
The widespread adoption of FHIR is paving the way for a major shift in healthcare, moving from a reactive model of treating illness to a proactive one focused on prevention. By connecting with community-based organizations and incorporating data on social determinants of health (SDOH), FHIR allows for a holistic view of a patient’s well-being. This vision of a “fully digital health system” and “unified data platforms” suggests a future where data flows effortlessly, enabling true care coordination and unlocking new avenues for cost reduction. The economic potential of this ecosystem, fueled by FHIR’s pervasive adoption, is expected to drive substantial growth in the healthcare interoperability market.
As FHIR adoption accelerates, the economic benefits will compound:
Network Effects
- Value increases as more organizations connect to FHIR-enabled networks
- Reduced costs for integration as standards become more widespread
- Enhanced capabilities through shared development and innovation
- Industry-wide efficiencies that benefit all participants
Innovation Enablement
- AI and machine learning applications powered by standardized, accessible data
- New care delivery models enabled by seamless information sharing
- Patient engagement tools that leverage comprehensive health records
- Population health insights that drive system-wide improvements
Regulatory Alignment
- CMS requirements that mandate FHIR adoption for certain programs
- Quality reporting that becomes automated rather than manual
- Public health integration that enables better disease surveillance and response
- Research capabilities that accelerate medical discoveries
The Strategic Imperative: Acting on FHIR’s Economic Promise
The economic case for FHIR is clear and compelling. With potential savings of $77.8 billion annually and proven ROI within 14 months, the question isn’t whether to implement FHIR—it’s how quickly organizations can begin realizing these benefits.
For healthcare organizations serious about financial sustainability and competitive advantage, FHIR represents more than a technology upgrade—it’s a strategic imperative that will determine success in an increasingly value-based healthcare landscape.
The organizations that embrace FHIR now will be the ones that thrive in tomorrow’s healthcare economy. Those that wait risk being left behind in an increasingly connected, efficient, and economically optimized healthcare ecosystem.
The economics are clear. The technology is proven. The time is now.
Healthcare organizations ready to unlock FHIR’s economic potential need partners who understand both the technology and the business case. The future of healthcare economics depends on making the right interoperability choices today.
Let’s talk about how you can start realizing the $77.8B opportunity—today.
Sources:
https://pubmed.ncbi.nlm.nih.gov/31589283/
https://westhealth.org/news/interoperability-a-call-to-action-hci-dc-2014/
https://www.precedenceresearch.com/healthcare-interoperability-solutions-market
https://healthcred.co.in/blogs/explaining-fhir
https://pmc.ncbi.nlm.nih.gov/articles/PMC9113654/
https://cartometric.com/statistical-impact-of-fhir-on-healthcare-costs-and-efficiency/
https://fire.ly/blog/8-key-insights-from-the-2024-state-of-fhir-survey/