Despite the rapid technology advancements, significant challenges persist in behavioural healthcare, particularly in community health clinics, outpatient clinics, and virtual clinics. This blog explores the growing role of technology in behavioral health, identifies current technology gaps, and outlines strategies to overcome these challenges. We will also delve into case studies and future innovations, highlighting how solutions like blueBriX's purpose-built behavioral health EHR can address these issues.

In recent years, behavioral health has taken center stage in the US healthcare landscape. This shift is driven by a growing recognition of the profound impact mental health has on overall well-being. According to the CDC, nearly 1 in 4 adults in the US live with a mental health condition. The increased focus on mental health is also reflected in policy changes, such as the Mental Health Parity and Addiction Equity Act, which aims to ensure mental health benefits are on par with physical health benefits.
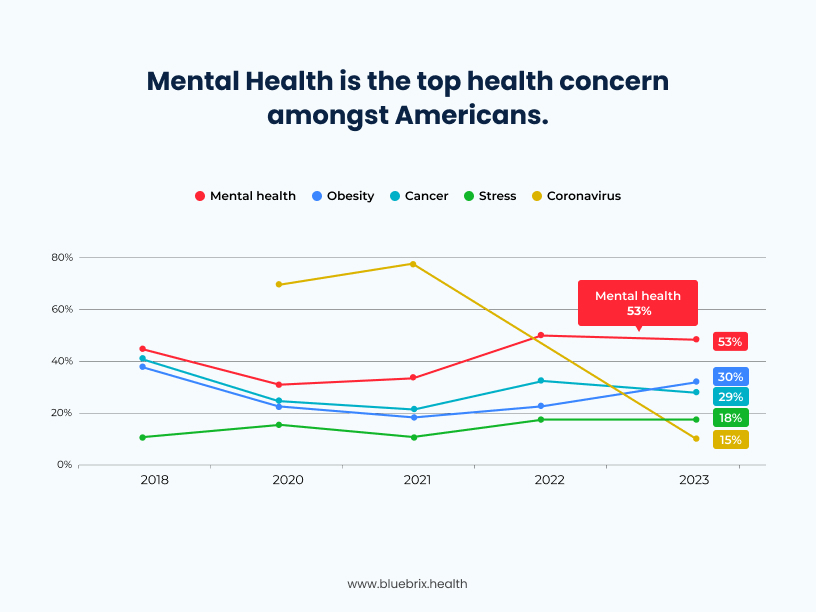
Source: https://www.statista.com
Technology has emerged as a game-changer in managing behavioral health clinics, offering innovative solutions to enhance patient care and streamline operations. For instance, AI-powered tools are revolutionizing clinical decision-making and patient interaction. A 2024 report from the American Medical Informatics Association revealed that 82% of behavioral health organizations are exploring AI to improve patient outcomes.
In this blog, we will examine the existing technological gaps in behavioral health care and propose strategies to bridge these divides. Furthermore, we will highlight real-world success stories where technology has significantly enhanced behavioral health services and explore future advancements poised to transform the field.
Technology Adoption in Behavioral Health Clinics
Technology is changing behavioral health, offering more efficient ways to improve patient care, make operations smoother, and get better outcomes. From telehealth to mobile health apps, technology is helping us bridge gaps in access and opening up new treatment possibilities. As we dive deeper into the digital age, using technology in behavioral health isn’t just a nice-to-have; it’s a must-have.
The COVID-19 pandemic accelerated the adoption of telehealth, with Medicare telehealth visits increasing dramatically from 840,000 in 2019 to over 52 million in 2020. Digital interventions, including telemedicine and mobile health applications, are transforming how care is delivered, making it more accessible and reducing stigma.
But here’s the thing: even with all these advancements, there are still some pretty big technology gaps in behavioral health. These gaps can make it tough to deliver the best care and take full advantage of tech innovations. We’re talking about issues like outdated infrastructure, systems that don’t talk to each other, and not enough training for healthcare providers.
However, significant technology gaps remain in behavioral health, including outdated infrastructure, interoperability issues, and insufficient training for healthcare providers. Addressing these gaps is crucial to fully leveraging technology in behavioral health.
What are the current technology gaps in behavioral health?
Identifying and addressing technology gaps is crucial for enhancing the efficiency and effectiveness of behavioral health services across various healthcare settings. Let’s delve into the specific challenges faced by community health clinics, outpatient clinics, and virtual clinics.

Common Issues in Community Health Clinics
Let’s start with community health clinics. These places often struggle with limited funding, old-school technology, and not enough IT support. They serve a ton of patients with all sorts of needs, which makes it hard to keep up with the latest tech. Plus, when different systems can’t share information, it leads to fragmented care and inefficiencies. Not ideal, right?
For example, CCBHCs are expanding rapidly with increased funding. There’s a big push to integrate behavioral health with primary care for a more holistic approach. Preventive care is becoming a priority, aiming to tackle mental health issues early on. Plus, there’s a strong focus on supporting vulnerable populations and using data to drive better decision-making. All these efforts are geared towards making behavioral health services more accessible and effective for everyone. But all of these need a strong technology support which is often lacking. Community health clinics such as CCBHCs and CHMCs encounter several technological challenges that impede optimal care delivery:
- Outdated Technology: Many clinics operate with legacy systems lacking modern functionalities, leading to inefficiencies and difficulties in managing patient information effectively. This typically results in inefficient workflows, more administrative work and less efficient care, everything adding up to physician burnout.
- Limited Resources: Financial constraints frequently hinder the adoption of advanced health information technologies (HIT), affecting clinics’ capacity to invest in necessary infrastructure and tools.
- Interoperability Issues: The inability of disparate systems to communicate seamlessly leads to fragmented care and hinders comprehensive patient management.
- Fragmented Data & Care: Data fragmentation, characterized by disparate and unintegrated health records, impedes clinicians’ ability to access comprehensive patient information, leading to potential treatment delays and errors. CCBHCs often struggle with fragmented care coordination. Care fragmentation, marked by uncoordinated services across multiple providers, often results in duplicated or unnecessary treatments, increasing healthcare costs and compromising patient outcomes.
- Compliance Issues: Ensuring compliance with state and federal regulations is a significant challenge, especially for CCBHCs. Clinics must adhere to state and federal reporting requirements and maintain accurate records. This adds to the administrative burden on staff.
Specific Challenges in Outpatient Clinics
Next up, outpatient clinics. These clinics face their own set of challenges! Outpatient care includes everything from primary care to specialty visits, diagnostics, and minor procedures. It’s a lot to juggle, and without standardized safety measures, patients can be at risk for preventable harm. Their unique technological hurdles include:
- Limited Health IT Adoption: Many outpatient clinics face significant challenges in implementing health information technology (IT), resulting in fewer opportunities for care coordination and data sharing. This gap often stems from inconsistent use of electronic health record (EHR) systems and sustainable funding challenges.
- Integration Difficulties: The development of digital mental health tools often occurs independently of mental health care providers and the broader health system context. This misalignment can lead to tools that are not well-designed for target users, hindering successful implementation and adoption.
- Data Privacy and Security Concerns: Behavioral health providers face challenges in accessing health IT capabilities due to concerns about data privacy and security. These challenges can impact their ability to provide services like telehealth effectively.
- Resource Constraints: Health information professionals encounter new responsibilities and challenges in bringing behavioral health platforms up to speed. Limited resources and training can impede the effective use of technology in these settings.
- Provider Shortages: The behavioral health landscape faces significant challenges, primarily stemming from a severe shortage of providers and increasing demand for services. This mismatch has led to long wait times, difficulty accessing care, and, in some cases, patients going without necessary treatment.
- Care Coordination: Managing patient information across various providers and settings is complex, especially when systems lack interoperability, leading to potential gaps in care.
- Patient Safety Risks: Without standardized safety measures and robust decision support systems, patients may be at risk for preventable harm during outpatient procedures.
Unique Barriers in Virtual Clinics
And then there are virtual clinics. While they offer great access to care, they also come with their own hurdles. Think technical issues, patients who aren’t super tech-savvy, and worries about privacy and data security. The COVID-19 pandemic really put these challenges in the spotlight, showing us just how important it is to have strong infrastructure and thorough training for both providers and patients. Virtual clinics, while expanding access to care, encounter distinct challenges such as:
- Technical Issues: Patients and providers may face difficulties with telemedicine platforms, such as connectivity problems and software incompatibilities, disrupting care delivery.
- Bandwidth Limitations: Inadequate broadband access, especially in rural areas, can hinder the delivery of virtual care services. This limitation can deter organizations from deploying telehealth technologies and restrict patients’ ability to participate in virtual consultations.
- Digital Literacy: Not all patients possess the necessary skills to navigate telehealth technologies effectively, potentially limiting their access to virtual care services. Notably, up to 38% of older patients are unprepared for telemedicine.
- Data Privacy and Security Concerns: Ensuring the confidentiality and security of patient information is crucial. Virtual clinics must adhere to stringent data protection regulations to maintain trust and comply with legal requirements.
- Integration with Existing Systems: Aligning digital mental health tools with current healthcare systems is challenging. Misalignment can lead to tools that are not well-designed for target users, hindering successful implementation and adoption.
With such diverse set of challenges within different behavioral health care settings, addressing these technology gaps demands targeted strategies. Depending upon their requirements, they should be looking at securing adequate funding, investing in modern and interoperable systems, enhancing IT support, and providing comprehensive training for both healthcare providers and patients. By tackling these challenges, healthcare facilities can improve the quality and accessibility of behavioral health services across all care settings.
How can Behavioral Health Clinics benefit from technology?
Choosing the Right Electronic Health Records (EHR) Systems
Upgrading to advanced EHR systems is essential for enhancing care coordination and improving patient outcomes. Purpose-built behavioral health EHRs, like blueBriX, are specifically designed to address the unique needs of behavioral health providers. These systems offer comprehensive features such as detailed progress notes, treatment plans, and outcome measurements that helps the provider focus better on patient-centric care than on administrative works. Additionally, they support interoperability, facilitating seamless data sharing between different care providers.
Benefits include:
1. Streamlined Administrative Processes:
- Reduced Paperwork: Automates documentation and administrative tasks, freeing up time for staff to focus on patient care.
- Efficient Patient Flow Management: Helps manage patient appointments, reduce wait times, and streamline check-ins and check-outs, improving overall clinic efficiency.
2. Improved Care Coordination:
- Interoperability: Supports seamless data sharing between different care providers, ensuring all providers have access to up-to-date patient information.
- Continuity of Care: Enhances communication and coordination among care teams, leading to better patient outcomes.
3. Enhanced Patient Engagement:
- Patient Portals: Provides patients with access to their medical records, communication tools with providers, and resources to support their care journey.
- Better Accessibility: EHRs with integrated telehealth features allow for continuous patient engagement through virtual visits, remote monitoring, and secure messaging, ensuring patients remain connected and involved in their care.
- Active Participation: Encourages patients to take an active role in their health management, fostering a sense of ownership and responsibility.
4. Accurate Data Management:
- Data Accuracy: Ensures that patient data is accurately recorded and easily accessible, reducing the risk of errors and improving the quality of care.
- Regulatory Compliance: Designed to comply with healthcare regulations such as HIPAA, ensuring that patient data is securely stored and managed.
5. Reliable Technology Integration:
- Telehealth Platforms: Offers robust telehealth solutions that minimize technical issues and provide a smooth user experience for both patients and providers.
- Virtual Care: Facilitates continuous patient engagement through virtual visits, remote monitoring, and secure messaging, ensuring patients remain connected and involved in their care.
6. Enhanced Privacy and Security:
- Compliance with Privacy Regulations: Safeguards patient information during virtual consultations, building trust in telehealth services.
- Secure Data Management: Ensures that all patient data is protected, fostering confidence in the clinic’s ability to maintain confidentiality.
Healthcare organizations are rapidly adopting EHR solutions, as evidenced by the U.S. behavioral health EHR market’s projected compound annual growth rate of 10.37% from 2025 to 2030. This trend highlights the growing recognition of the benefits that EHR systems bring to the behavioral health sector. A purpose-built EHR system can transform the operations of community, outpatient, and virtual behavioral clinics, leading to more efficient workflows, better patient outcomes, and enhanced overall care quality.
Leveraging Mobile Health (mHealth) Applications
mHealth apps are another fantastic tool for supporting patient self-management and treatment adherence. These apps can send medication reminders, track symptoms, and offer therapeutic exercises like cognitive-behavioral therapy (CBT). By integrating mHealth apps into their practice, clinics can boost patient engagement and improve health outcomes.
1. Convenience and Accessibility
- 24/7 Access to Care: mHealth apps allow patients to access healthcare services and resources anytime, anywhere, making it easier for them to receive support when they need it.
- Remote Patient Monitoring (RPM): Clinics can monitor patients’ conditions remotely, enabling timely interventions and reducing the need for frequent in-person visits.
2. Empowerment and Active Engagement
- Patient Empowerment: mHealth apps empower patients to take an active role in their health management by providing tools for tracking symptoms, medication adherence, and progress.
- Interactive Tools: Features like medication reminders, symptom trackers, and therapeutic exercises (e.g., cognitive-behavioral therapy) help patients stay engaged in their treatment plans.
3. Improved Health Monitoring
- Real-Time Data Collection: mHealth apps can collect real-time data on patients’ health status, providing clinicians with valuable insights for personalized care.
- Early Detection: Continuous monitoring can help detect early signs of deterioration, allowing for prompt interventions and better management of behavioral health conditions.
4. Enhanced Communication
- Patient-Provider Communication: mHealth apps facilitate secure communication between patients and providers, enabling timely consultations and support.
- Family and Caregiver Involvement: These apps can also involve family members and caregivers in the care process, improving overall support for the patient.
5. Medication Adherence
- Reminders and Alerts: mHealth apps can send medication reminders and alerts to patients, helping them adhere to their prescribed treatment plans.
- Tracking Adherence: Clinics can track patients’ medication adherence and intervene if they notice any issues, ensuring better treatment outcomes.
6. Personalized Approach
- Tailored Interventions: mHealth apps can offer personalized interventions based on individual patient data, improving the effectiveness of treatment plans.
- Customizable Features: Patients can customize app features to suit their preferences and needs, enhancing their engagement and satisfaction.
7. Support for Remote and Underserved Areas
- Access to Care: mHealth apps can bridge the gap for patients in remote or underserved areas, providing them with access to behavioral health services that might otherwise be unavailable.
- Cost-Effective Solutions: These apps offer cost-effective solutions for delivering care, reducing the financial burden on both patients and clinics.
8. Health Education and Awareness
- Educational Resources: mHealth apps can provide patients with educational resources about their conditions, treatment options, and self-care strategies.
- Awareness Campaigns: Clinics can use these apps to run awareness campaigns, promoting mental health and reducing stigma.
Implementing Telehealth Solutions
Telehealth has become a game-changer in behavioral health, letting patients access therapy, counseling, and medication management from the comfort of their homes. Telehealth addresses barriers such as transportation challenges and stigma associated with in-person visits, promoting consistent care. A study by Harvard Medical School found that patients at practices with high telemedicine use had more mental health visits and better continuity of care.
To make telehealth work, clinics need to invest in reliable tech, follow privacy regulations, and train both providers and patients. To effectively implement telehealth, clinics should:
- Invest in Reliable Technology: Ensuring robust telehealth platforms minimizes technical issues, enhancing the patient experience.
- Adhere to Privacy Regulations: Compliance with regulations like HIPAA safeguards patient information, fostering trust in telehealth services.
- Provide Training: Educating both providers and patients on using telehealth platforms ensures smooth interactions and maximizes the benefits of virtual care.
By embracing these strategies, behavioral health clinics can bridge technology gaps, leading to more efficient operations and improved patient care.
What are the other key aspects supporting the adoption of technology in Behavioral Health?
Policy Implications in Behavioral Health
Policy changes, such as funding initiatives and regulatory adjustments, play a crucial role in supporting the adoption of technology in behavioral health. Increased funding can help clinics invest in modern infrastructure and advanced health information technologies. Regulatory adjustments can streamline the implementation of telehealth and mHealth applications, ensuring they comply with privacy and security standards. Policies that promote interoperability and data sharing can enhance care coordination and improve patient outcomes.
Patient Perspectives in Behavioral Health
Including patient experiences and feedback on using technology in behavioral health settings provides a more holistic view of the impact. Patients have reported increased convenience and accessibility with telehealth services, allowing them to receive care from the comfort of their homes. mHealth apps have empowered patients to take an active role in managing their health, with features like medication reminders and symptom tracking. However, some patients face challenges with digital literacy and accessing reliable internet, highlighting the need for comprehensive training and support.
Training and Education in Behavioral Health
Training healthcare providers and patients in using new technologies effectively is essential for maximizing the benefits of technological advancements in behavioral health. Providers need to be proficient in using EHR systems, telehealth platforms, and mHealth apps to deliver high-quality care. Patients require guidance on navigating these technologies to ensure they can fully participate in their treatment plans. Continuous professional development and patient education programs can bridge the knowledge gap and enhance the overall effectiveness of technology in behavioral health.
How can Behavioral Health Clinics become future-ready?
The future of behavioral health technology looks bright, with advancements in artificial intelligence (AI), machine learning, and data analytics set to transform care delivery. AI-powered tools can help with clinical decision-making, predict patient outcomes, and personalize treatment plans. Plus, emerging technologies like virtual reality (VR) and augmented reality (AR) offer exciting new possibilities for therapeutic interventions. These innovations are reshaping care delivery, offering tools for clinicians and enhanced experiences for patients.
AI-Powered Tools in Behavioral Health
Artificial intelligence is playing a pivotal role in various aspects of behavioral health care:
- Clinical Decision Support: AI algorithms can analyze patient data to assist clinicians in making informed decisions. For example, AI has demonstrated high accuracy in predicting suicidal thoughts and significant mental health issues, enabling timely interventions.
- Outcome Prediction: Machine learning models can forecast patient outcomes based on historical data, aiding in the development of proactive care plans.
- Personalized Treatment Plans: AI facilitates the creation of tailored treatment strategies by analyzing individual patient profiles, leading to more effective interventions.
Emerging Technologies: VR and AR
Virtual reality (VR) and augmented reality (AR) are introducing new dimensions to therapeutic interventions:
- Exposure Therapy: VR enables controlled exposure to anxiety-inducing stimuli in a safe environment, benefiting patients with phobias or PTSD.
- Skill Development: AR applications can simulate real-world scenarios, helping patients develop coping mechanisms and social skills.
Generative AI and AI Agents
Generative AI and AI agents are emerging as influential tools in behavioral health:
- Therpaeutic Support: AI-driven chatbots offer immediate, judgment-free support to individuals seeking mental health assistance. For instance, AI chatbots are increasingly being used for mental health support, providing a cost-effective and accessible alternative to traditional therapy.
- Content Creation: Generative AI can develop personalized therapeutic content, such as guided meditations or cognitive behavioral exercises, enhancing patient engagement.
- Administrative Efficiency: AI agents can automate routine tasks like appointment scheduling and documentation, allowing clinicians to focus more on patient care.
Preparing for Technological Advancements
To effectively integrate these technologies, behavioral health clinics should:
- Invest in Education and Training: Continuous professional development ensures staff are proficient in utilizing new tools and understanding their implications.
- Stay Updated on Regulations: Keeping abreast of evolving policies ensures compliance and ethical application of technologies.
- Foster a Culture of Innovation: Encouraging openness to new ideas and technologies promotes adaptability and continuous improvement.
- Collaborate with Technology Providers: Engaging with tech developers through partnerships and pilot programs facilitates the customization of solutions to meet specific clinical needs.
By embracing these strategies, behavioral health clinics can effectively navigate the evolving technological landscape, ultimately enhancing patient outcomes and operational efficiency.
Conclusion
Bridging the technology gaps in behavioral health isn’t just a technical upgrade; it’s a transformative journey. By embracing telehealth solutions, enhancing Electronic Health Record (EHR) systems, and integrating mobile health (mHealth) applications, clinics can revolutionize patient care and streamline operations. Using the right technologies, behavioral health clinics have improved documentation efficiency, enabling clinicians to dedicate more time to direct patient care.
As the landscape of behavioral health continues to evolve, it’s essential for clinics to stay ahead by adopting these technological advancements. By proactively addressing existing technology gaps and staying informed about emerging trends, clinics can enhance patient care and operational efficiency, ultimately better serving their communities.
If your clinic is looking to overcome technology gaps and enhance patient care, consider partnering with blueBriX. Our purpose-built behavioral health EHR system is designed to tackle the unique challenges of behavioral health providers, offering comprehensive solutions to streamline operations and improve outcomes.
Contact us today to learn more about how we can support your clinic’s technological needs.