In the past, the healthcare system operated primarily on a reactive model. Patients would seek care only when they were already sick, and providers would focus on treating the symptoms of an existing disease. While this approach has saved countless lives, it is often costly, inefficient, and fails to address the root causes of poor health.
Today, the healthcare industry is undergoing a fundamental shift towards a proactive and preventive model. This new era is driven by a desire to improve patient outcomes, manage escalating costs, and promote overall population health. At the heart of this transformation lies the strategic practice of risk stratification.
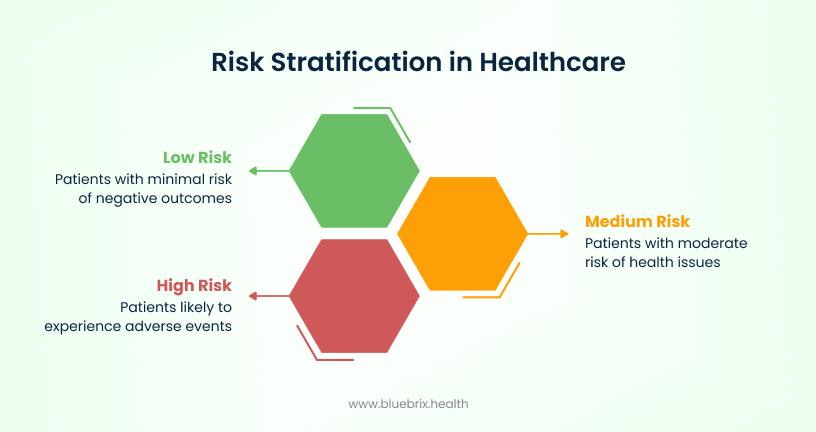
Risk stratification is the process of categorizing a population based on their predicted future health risks and needs. At its core, risk stratification aims to identify individuals who are most likely to experience adverse health events, utilize high levels of healthcare resources, or benefit most from specific interventions. It’s about segmenting a patient population into distinct groups – from low-risk, healthy individuals to high-risk patients with complex chronic conditions – to tailor care delivery appropriately.
Why risk stratification is an organizational imperative
For any modern healthcare organization, implementing a robust risk stratification strategy is a critical imperative for survival and success. It provides the foundation for smarter resource allocation, better patient care, and improved financial performance.
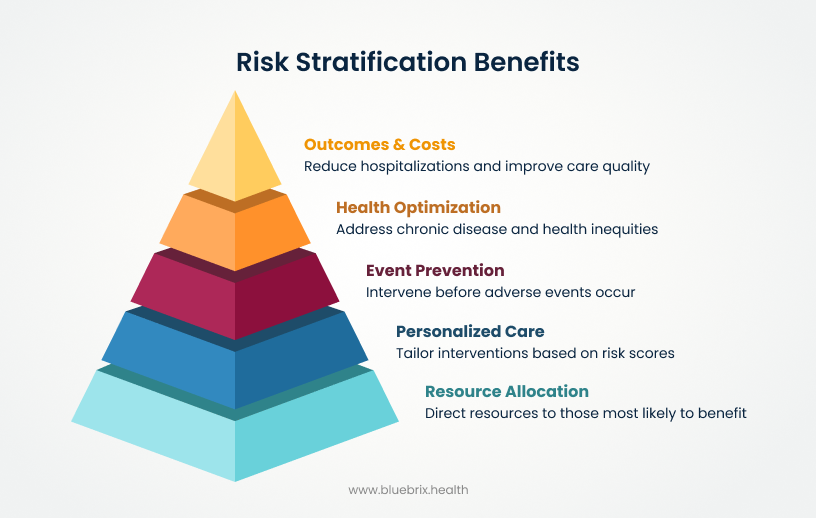
Optimizing resource allocation: the smart way to manage the patient population
One of the most significant challenges in healthcare is the uneven distribution of costs. The well-known “80/20 rule” suggests that roughly 80% of healthcare costs are attributable to just 20% of the patient population. Risk stratification allows organizations to address this disparity head-on by identifying the high-risk 20% and directing more intensive resources toward them. This proactive approach helps to prevent costly and unplanned hospital admissions and readmissions by addressing health issues early, before they escalate. By doing so, it ensures that the right level of care is provided to the right patient at the right time, leading to a more efficient system for everyone.
Enhancing patient outcomes: delivering personalized and safer care
Risk stratification provides the data and insights necessary to create truly personalized care. By identifying individuals who are “at-risk” (e.g., a patient with pre-diabetes and a family history of heart disease) and “rising risk” (e.g., a patient with well-controlled diabetes who just moved and lost their social support network), providers can intervene with a high degree of precision. This includes creating individualized care plans, providing dedicated care management support, and implementing targeted interventions to improve chronic disease management. The result is safer, more effective care that is tailored to each patient’s unique needs, leading to better health outcomes and a higher quality of life.
Driving operational efficiency & cost reduction: building a sustainable healthcare model
In a system where margins are tight, operational efficiency is key. Risk stratification helps healthcare organizations identify and minimize unnecessary services and waste, such as redundant tests or avoidable hospital visits. By proactively managing high-risk patients, organizations can reduce the overall cost of care while improving its quality. This approach streamlines workflows for clinicians and administrative staff, reduces administrative burdens, and ultimately builds a more financially sustainable healthcare model.
Empowering patients and promoting engagement: fostering a collaborative approach to health
Effective risk stratification is a two-way street. By providing patients with a clear and shared understanding of their own health risks, organizations can empower them to take a more active role in their care. When patients understand why a particular intervention or care plan is important, they are more likely to adhere to it. This boosts patient engagement, promotes self-management of chronic conditions, and fosters a collaborative relationship between patients and their care teams, leading to lasting improvements in health.
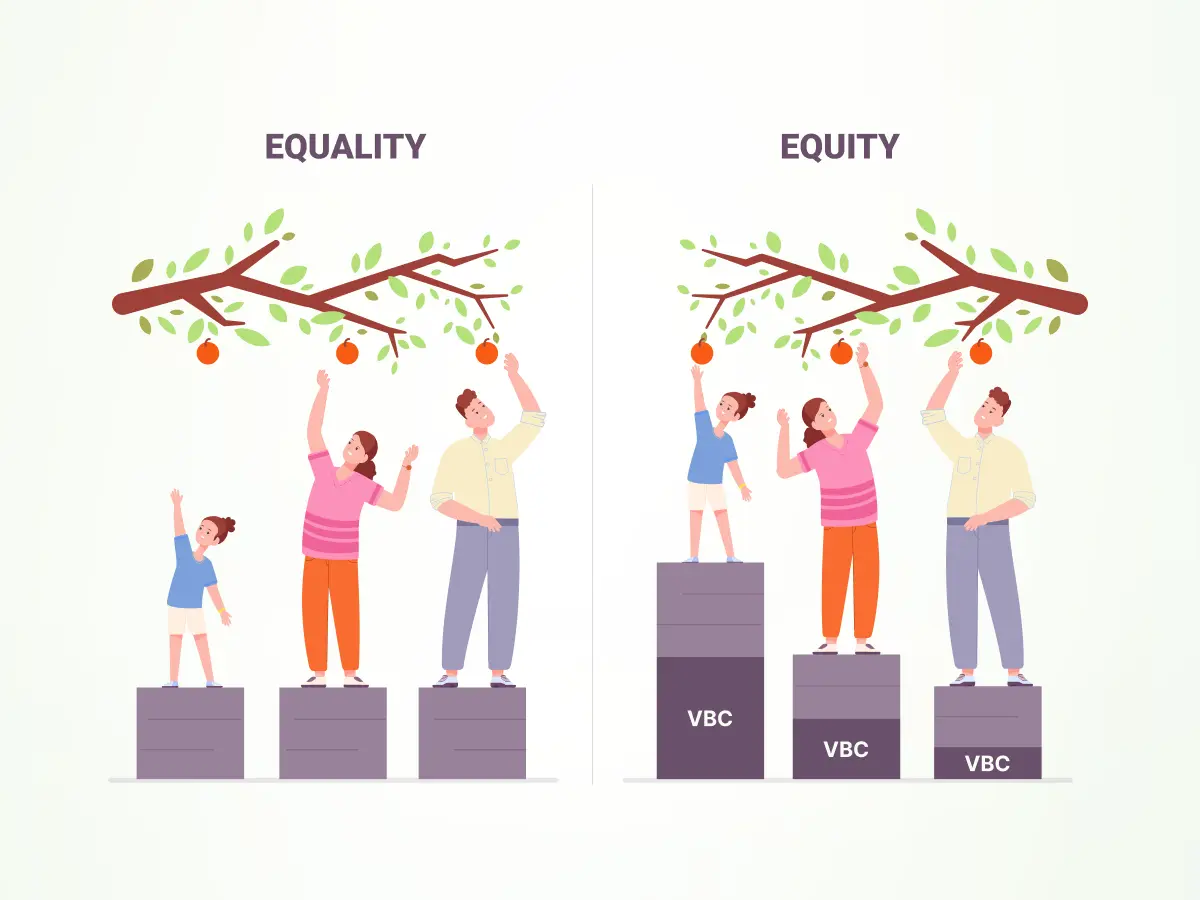
Promoting health equity: addressing disparities in care
Risk stratification can also be a powerful tool for promoting health equity. By incorporating data on social determinants of health (SDoH), organizations can identify vulnerable populations and uncover systemic barriers to care that may not be apparent from clinical data alone. This allows for the design of targeted interventions that address the unique challenges faced by these populations, helping to close existing gaps in care and ensure that all patients have an equitable opportunity to achieve their best possible health.
Consequences of not performing risk stratification in healthcare
Failing to implement risk stratification in healthcare settings can lead to worse patient outcomes, increased costs, and inefficient resource allocation.
Clinical and patient safety impacts
Without risk stratification, high-risk patients may be overlooked, leading to:
- Increased preventable hospital admissions: Prioritizing interventions for all patients equally fails to identify those most likely to deteriorate, resulting in avoidable admissions.
- Higher rates of adverse outcomes: Lack of systematic risk profiling removes early warning signals for severe events, increasing morbidity and mortality among vulnerable subgroups.
- Worse post-discharge transitions: In acute heart failure, absence of risk stratification before emergency department disposition has been linked to poorer outcomes for discharged patients.
Resource utilization and cost inefficiencies
Risk stratification aligns resource intensity with patient needs. Its absence results in:
- Higher overall healthcare spending: Predictive allocation based on risk can prevent a significant portion of spending driven by a small percentage of patients. Without stratification, high-need patients remain unmanaged.
- Poor cost-effectiveness: Systematic reviews reveal that population health programs relying on unvalidated or absent risk stratification show no clinical benefits and may even cause harm, undermining cost-effectiveness in constrained systems.
Care management and population health implications
In population health initiatives, neglecting risk stratification leads to:
- Inequitable care delivery: Social determinants and comorbidities intensify risk, but without stratification, vulnerable subgroups are not identified, perpetuating health disparities.
- Increased provider workload: Time-consuming blanket interventions lack precision, burdening staff with ineffective measures and diverting attention from patients who need intensive management.
Methodologies and approaches for risk stratification
Once the data is collected, it must be analyzed using a methodology that is appropriate for the organization’s goals and resources.
Assessment tools & clinical data: The “what” of illness
This approach utilizes readily available clinical information from electronic health records, such as:
- Diagnoses: Chronic conditions like diabetes, heart failure, COPD.
- Lab results: A1C levels, cholesterol, kidney function.
- Medication history: Polypharmacy, adherence patterns.
- Past Medical history: Previous hospitalizations, surgeries.
- Demographics: Age, gender.
Various tools have been developed to quantify risk based on clinical data. Examples include the Charlson Comorbidity Index, which predicts mortality based on co-existing conditions, or specific disease risk scores for cardiovascular disease or stroke.
While clinical data provides a vital snapshot of a patient’s medical status, relying solely on it presents significant challenges:
- Missing the “Why” behind health issues: Clinical data tells us what a patient’s medical conditions are, but it rarely explains why those conditions developed or why a patient might struggle to manage them. For instance, high blood pressure could be due to genetic predisposition, or it could be exacerbated by chronic stress from an unstable housing situation.
- Data silos and interoperability challenges: Clinical data often resides in disparate systems – hospital EHRs, practice management software, lab systems – making it incredibly difficult to get a complete, unified view of a patient’s health journey. This fragmentation hinders comprehensive risk assessment.
Social determinants of health (SDOH): The “why” of wellness
In recent years, the healthcare industry has increasingly recognized the monumental influence of Social Determinants of Health (SDOH) on an individual’s well-being. SDOH are the non-medical factors that influence health outcomes. These include:
- Economic stability: employment, income, debt, food security.
- Education access and quality: literacy, higher education.
- Healthcare access and quality: insurance coverage, access to providers, linguistic barriers.
- Neighborhood and built environment: housing stability, transportation, safety, access to healthy foods.
- Social and community context: support systems, discrimination, civic participation.
How is SDOH Data collected and utilized for risk assessment?
SDOH data can be collected through patient surveys, community-level data, postal codes, and screening tools. When integrated, this data can highlight vulnerabilities that clinical data might miss, such as a patient’s inability to afford medications, lack of reliable transportation to appointments, or living in an unsafe neighborhood that limits physical activity. Despite its immense value, SDOH-only stratification faces its own set of hurdles:
- Lack of standardized SDOH data collection: There’s no universal standard for how SDOH data is collected, making it inconsistent and difficult to compare across different settings or populations.
- Difficulty in integrating qualitative SDOH data with quantitative clinical data: Much of SDOH information is qualitative (e.g., “feels unsafe in neighborhood”), which is challenging to combine with quantitative clinical metrics (e.g., blood pressure readings) for a holistic risk score.
- Stigma and privacy concerns around SDOH data: Patients may be hesitant to share sensitive information about their social or economic circumstances due to privacy concerns or fear of judgment.
Clubbing clinical data and SDOH
Advanced platforms can break down traditional data silos, ingesting, cleansing, and integrating vast amounts of data from various sources – EHRs, claims data, patient-reported outcomes, community data, and SDOH screenings – into a single, unified patient record. This provides an unprecedented 360-degree view of each individual’s health and life circumstances.
Such comprehensive systems don’t stop at just identifying risk; they translate those insights into actionable strategies through dynamic cohort management. Once stratified, patients can be automatically grouped into dynamic cohorts based on shared risks, conditions, and needs (e.g., “High-Risk CHF with Transportation Barriers,” “Diabetic Patients with Food Insecurity,” “Post-Surgical Patients needing Home Support”). This segmentation allows for highly targeted, efficient interventions.
Intuitive dashboards can provide care teams with real-time visibility into their patient cohorts. They can monitor key metrics, track progress, identify emerging needs, and engage directly with patients through integrated communication tools. Customizable workflows ensure that the right interventions are triggered at the right time, whether it’s scheduling a social worker visit, initiating a telehealth consultation, or providing educational resources. Flexible form builders allow organizations to create custom assessment tools to gather additional, highly specific data relevant to their patient population or specific initiatives. This ensures that risk stratification remains dynamic and responsive to evolving patient needs.
The critical connection: how risk stratification enables VBC success
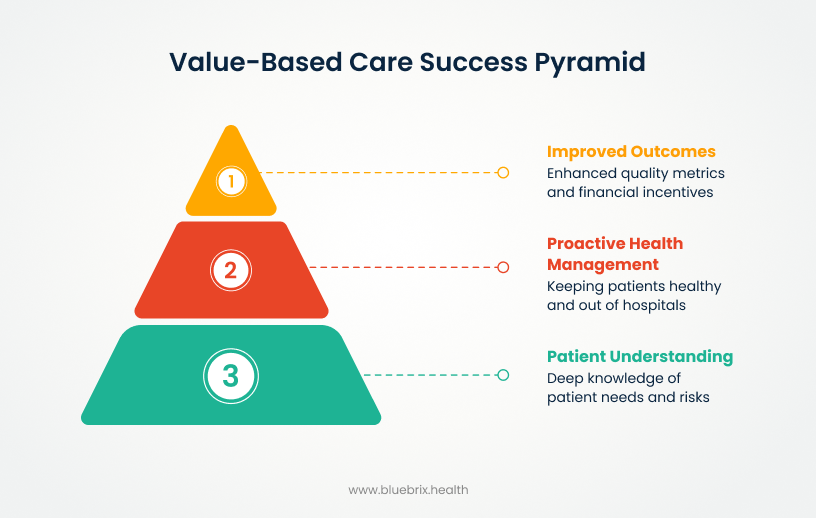
Risk stratification is the engine that drives a successful VBC program. It provides the actionable intelligence needed to manage a population-level contract. By segmenting the patient population, organizations can:
- Align with quality metrics and performance incentives: VBC contracts often include performance incentives tied to specific quality metrics, such as blood pressure control for hypertensive patients or A1c levels for diabetic patients. Risk stratification helps identify the patients who are most at risk of not meeting these targets, allowing for targeted interventions that can improve these metrics and secure bonus payments.
- The shift from volume to outcomes: Risk stratification is the key to managing the shift from a volume-based to an outcomes-based mindset. Instead of simply performing as many services as possible, providers can use risk data to focus their efforts on the patients who will benefit most from a specific intervention, ultimately leading to better health outcomes and a more efficient use of resources.
- Achieving the triple aim in a VBC framework: The Triple Aim—improving the patient experience, improving population health, and reducing per capita healthcare costs—is the guiding principle of VBC. Risk stratification is the foundational tool that makes this possible by enabling providers to identify, manage, and care for high-risk patients in a way that simultaneously improves health, enhances patient satisfaction, and controls costs.
blueBriX: your partner in simplifying risk stratification
Implementing a comprehensive risk stratification program can be complex, often hindered by fragmented data, manual processes, and the lack of a centralized platform. blueBriX is an intelligent and integrated platform designed to address these challenges and serve as a healthcare organization’s essential partner in the journey to proactive, value-based care.
Addressing common implementation challenges
- Breaking down data silos and integration headaches: The single greatest hurdle to effective risk stratification is the inability to combine disparate data sources. Patient data is often scattered across different EHRs, claims databases, and social services records. blueBriX solves this by providing a unified platform that seamlessly integrates clinical, claims, SDoH, and patient-reported data, creating a single, comprehensive view of the patient population.
- Eliminating manual processes: Without an automated solution, the process of identifying at-risk patients, generating care plans, and tracking outcomes is manual, time-consuming, and prone to human error. blueBriX automates these workflows, freeing up valuable time for clinicians and care managers to focus on what matters most: patient care.
The bluebrix advantage: an intelligent and integrated platform
blueBriX is more than just a data aggregator; it is a full-featured, end-to-end solution built to empower healthcare providers.
- Advanced AI and predictive analytics for unmatched accuracy: The platform uses proprietary AI and machine learning models to analyze the integrated data. This allows for highly accurate predictive risk scores that go beyond simple clinical assessments, identifying both at-risk and rising-risk individuals with a high degree of precision.
- Customizable dashboards for actionable, real-time Insights: blueBriX provides intuitive, customizable dashboards that give care teams a real-time, actionable view of their patient population. Clinicians can filter by risk level, disease state, or SDoH factors, allowing them to quickly identify patients who need immediate attention.
- Automated workflows and care plan generation: The platform automates the creation of personalized care plans based on a patient’s unique risk factors. It can also automate outreach, appointment scheduling, and referrals to social services, ensuring that no patient falls through the cracks.
- A No-code app builder for tailored solutions: The no-code app builder allows organizations to create their own custom workflows and applications without the need for a developer. This enables rapid deployment of new programs and solutions tailored to the specific needs of a community or patient population.